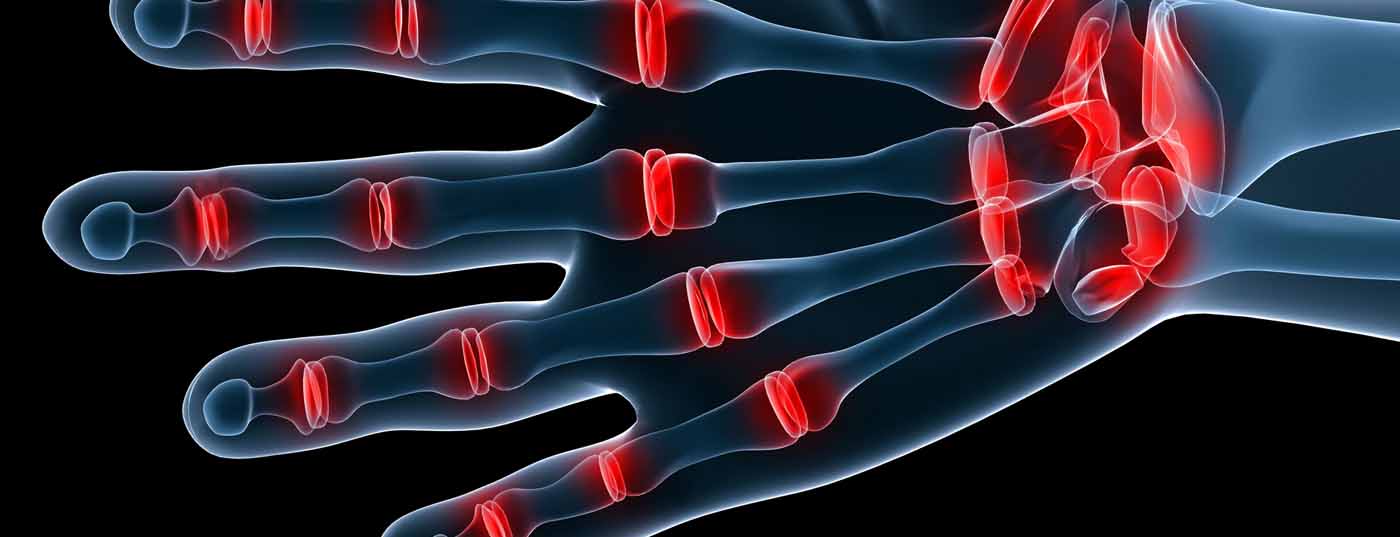
Rheumatoid arthritis (RA) is a chronic disease that causes swelling and, consequently, restricted movement and joint pain. It is twice as common in women as in men, and the incidence is high worldwide. Although RA primarily affects the joints, the inflammation can also spread to other organs. Disease severity and inflammation are associated with increased risk of coronary heart disease compared with the normal population, so effective management of these factors is critical. At the ACR Congress in San Diego, the results of new studies were discussed in this regard. It was about a possible effect of previous RA therapy for other disease entities.
(ag) Tumor necrosis factor (TNF) inhibitors such as infliximab, adalimumab, golimumab, and certolizumab pegol, and the genetically engineered protein etanercept, form a class of drugs that have been in use for ten years. It is used worldwide to treat inflammatory diseases such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), juvenile arthritis, Crohn’s disease, ankylosing spondylitis (ankylosing spondylitis) and psoriasis. As current treatment options in RA lead to good control of joint inflammation, the question is whether this can also address certain comorbidities.
Can TNF inhibitors reduce ACS risk?
A group of researchers from Sweden has now investigated whether TNF inhibitors in the treatment of RA patients also reduce the increased risk of acute coronary heart disease (ACS). The results were presented by Lotta Ljung, MD, Umeå, at this year’s ACR Congress [1]. Specifically, a cohort of 7704 patients was formed from the Swedish Biologics Registry who had no history of ischemic heart disease up to that time and who started their treatment for the first time with a TNF inhibitor between 2001 and 2010. The weighted comparison cohorts included 23 112 patients with RA from the national patient registry who had never taken a biologic and 38 520 individuals from the general population registry. Patients were considered “active” if they took TNF inhibitors until the defined endpoint and for an additional 90 days.
ACS was defined as a primary struck diagnosis of myocardial infarction, unstable angina, or myocardial infarction resulting in death. In the general population, these occurred at a rate of 3.3/1000 persons per year, compared with 5.7/1000 in RA patients who had “active” status and 8.6/1000 in RA patients who never took a biologic. After controlling for other contributing factors, the likelihood of suffering an ACS was 50% higher in those RA patients who were “actively” taking TNF inhibitors and twice as high in those who never did, compared with the general population. Compared to those who abstained from biologics, the risk was consequently 27% lower for patients with “active” status. This study shows that taking TNF inhibitors also has an effect on cardiovascular comorbidities, but it says nothing about whether the lower risk is due to the drugs themselves or to better control of inflammation.
British study confirms effect
Audrey Low, Manchester, presented the results of a UK study that compared the risk and severity of myocardial infarction in RA patients on TNF inhibitors with those on nonbiologic disease-modifying anti-rheumatic drugs (DMARDs) [2]. This was based on data from the ongoing prospective BSRBR-RA trial, which is looking at the safety of biologic therapy in RA, and from the Myocardial Ischaemia National Audit Project (MINAP), a national data collection of heart attack hospitalizations in England and Wales.
The analysis compared RA patients recruited between 2001 and 2008 who started TNF inhibitor therapy (etanercept, infliximab, adalimumab) and those treated with nonbiologic DMARDs. The result is similar to the previously mentioned study: patients treated with TNF inhibitors had a reduced risk of heart attack compared to the other group. However, the severity of infarcts that nevertheless occurred was the same in both groups.
Enhanced efficacy of RA treatment
Rituximab is a drug commonly used in RA, but also in granulomatosis with polyangiitis and some cancers. The suggestion that the therapeutic pathway is also safe and effective for IgG4-associated diseases was discussed at the ACR Congress. John Stone, MD, Boston, presented the results of a study [3] that looked at just that.
IgG4-associated disease (IgG4-RD) has only recently been discovered. It is a multi-organic condition that mimics numerous rheumatologic disease states, among others. It can affect almost all organs in the body. The most common rheumatologic mimics are Sjögren’s syndrome, granulomatosis with polyangiitis, systemic lupus erythematosus, and sarcoidosis. In addition, IgG4-RD also mimics infections and malignancies, especially lymphoma, pancreatic, renal or lung carcinomas. IgG4-RD is now defined as a distinct disease entity, uniting over a dozen conditions previously considered single-organ entities.
A team of researchers led by Stone now investigated whether classic RA therapy with rituximab also helps against IgG4-RD. “New therapeutic strategies are urgently needed in this disease,” Stone said. “The patients in our study had multiple affected organs (e.g., salivary glands, lungs, lymph nodes, pancreas, kidneys, prostate), and their IgG4-RD was pathologically confirmed. They were treated with 1000 mg rituximab at baseline and day 15, but not with a maintenance dose after day 15. With each rituximab dose, they also received 100 mg methylprednisolone. Only two patients were treated with prednisone in addition to rituximab.”
Patients were assessed at one, three, five, six, eight, ten, and twelve months after the first dose of rituximab for three items: Disease response to the drug, disease flare-up by month six, and the need to add a steroid between months two and six. These factors (response, no flare, no need for steroids) formed the primary endpoint.
Twenty-six of the 28 patients followed for at least one month and 22 of 24 followed for three months achieved a reduction in disease activity without the use of steroids. Among the 23 patients followed up to six months, 20 met the three conditions of the primary endpoint. Only two of the 28 participants required an increase in prednisone after the first month of study. Stone’s team did not find any severe or unexpected side effects with rituximab.
“This study represents an important step for patients with IgG4-RD and opens interesting research perspectives. Rituximab seems to represent an important new treatment option for them, which could replace protracted and even indefinite therapy with steroids, often combined with other potentially toxic drugs of uncertain value. Of course, however, the results need to be verified in a large randomized trial and also the pathways of action of rituximab in the context of this disease need to be clarified,” Stone concluded his presentation.
Source: ACR/ARHP Annual Meeting, October 26-30, 2013, San Diego.
Literature:
- Ljung L, et al: Tumour Necrosis Factor Inhibitors And The Risk Of Acute Coronary Syndrome In Rheumatoid Arthritis – a National Cohort Study. ACR Abstract #804.
- Low ASL, et al: Incidence and Severity Of Myocardial Infarction In Subjects Receiving Anti Tumour Necrosis Factor Drugs For Rheumatoid Arthritis: Results From Linking the British Society For Rheumatology Biologics Register For Rheumatoid Arthritis and Myocardial Ischaemia National Audit Project. ACR Abstract #2760.
- Stone J, et al: Rituximab For The Treatment Of IgG4-Related Disease: A Prospective Clinical Trial. ACR Abstract #2649.
CONGRESS SPECIAL 2014; 6(1): 2-3