The surgical techniques used to rehabilitate peripheral arterial disease (PAVD) are thromboendarterectomy and bypass grafting. Which procedure is used when, how does the operation proceed and what should be taken into account?
Peripheral arterial disease (PAVD) is a systemic disease that leads to structural and functional remodeling of arterial vessels [1]. This results in reduced blood flow, which may be asymptomatic for a long time or manifest with symptoms such as intermittent claudication, ischemic rest pain, or gangrene. The pathophysiological correlate of PAVD is atherosclerosis, a chronic inflammation of the vessel wall in which a plaque composed of lipids, smooth muscle cells, and macrophages is deposited subendothelially. As it progresses, this plaque may lead to stenosis of the vascular lumen or induce local thrombus formation via rupture [2].
Because it is a systemic disease, PAVD is often associated with coronary artery disease (CAD) and cerebrovascular occlusive disease (CVI). Decreased ankle-brachial index (ABI) is associated with increased cardiovascular mortality [3]. The prevalence of PAVD is reported to be 7-15% [4,5]. Nicotinabuse, diabetes mellitus, arterial hypertension, and hypercholesterolemia are the most relevant risk factors [6].
For classification purposes, the classification according to Fontaine has proven useful in everyday clinical practice. On the basis of the symptoms and the ABI and oscillography measurements, a distinction is made between four stages. Stage I (asymptomatic, status after interventional or surgical revascularization) and II (intermittent claudication) are non-critical situations. Stage III (rest pain) and IV (gangrene), on the other hand, present a critical perfusion defect that can lead to limb loss if left untreated.
Diagnostics
In the anamnesis, the pain-free walking distance and any risk and concomitant factors are asked. In addition, the type, localization and time of the pain (nocturnal rest pain?) are asked. Clinical examination includes ipsi- and contralateral pulse status, sensorimotor function, skin coloration, and (acral) lesions. ABI, occlusion pressure measurement, and oscillography can be used to confirm the suspected diagnosis on the one hand and to classify the patient into non-critical and critical perfusion defects on the other. Finally, duplex sonography allows precise localization of the stenosis and its assessment in terms of extent and degree. Complementary angiography is used to confirm the duplex findings and to evaluate the in- and outflow vessels for catheterization or surgical repair.
Endovascular or surgical rehabilitation?
In the non-critical stage, therapy consists of modification of the risk profile (nicotine cessation, diabetes control), drug therapy in the sense of “best medical treatment” (platelet aggregation inhibition and plaque stabilization), and supervised gait training. The decision for surgical or endovascular repair depends on the symptoms, the anatomical location, the extent of the lesion, and the patient’s general condition. Invasive intervention should not be performed in asymptomatic patients or those with only mild claudication symptoms. Percutaneous or surgical intervention is indicated for:
- Claudication symptoms with significant reduction in quality of life,
- Critical ischemia with impending limb loss,
- previous surgical revascularization and new onset of stenosis and/or occlusion in the operated area and in the in-flow and out-flow vessels.
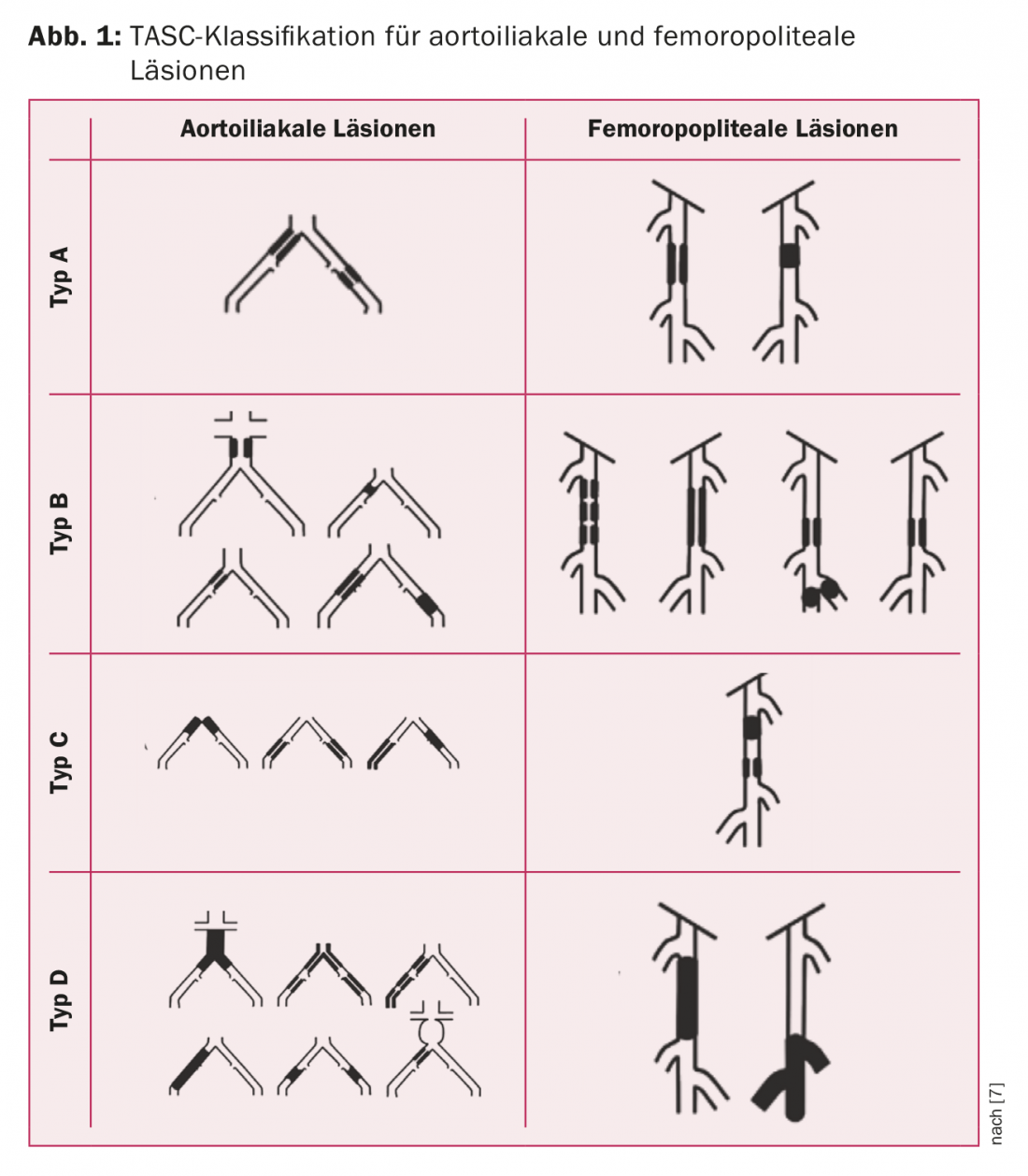
The therapeutic decision should be made in an interdisciplinary discussion of the treating disciplines angiology, interventional radiology and vascular surgery. The basis for the decision is the TASC classification [7]. As a “rule of thumb”, type A and B lesions should be primarily rehabilitated endovascularly and type C and D lesions primarily surgically (Fig. 1) . Additional criteria are the age as well as comorbidities of the patient and the presence of a good quality vein for bypass. Table 1 summarizes the procedure recommended in the ESC guidelines.
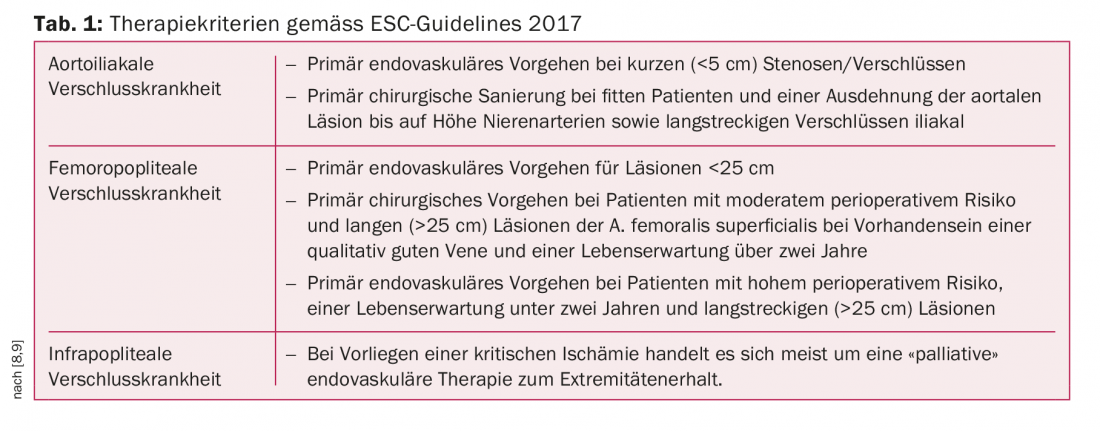
In isolated symptomatic stenoses of the femoral bifurcation, which often present as claudication symptoms, endovascular therapy has little value because the outcome is significantly better after surgical repair. In the presence of additional iliac occlusive disease, a hybrid procedure is used to openly surgically repair the femoral bifurcation and retrograde endovascular recanalization of the iliac axis.
Thromboendarterectomy and bypass grafting, or a combination of both procedures, are the surgical approaches used to rehabilitate PAVD.
Thromboendarterectomy (TEA)
The typical localization is the femoral bifurcation. Both the common femoral artery (AFC) and the branches of the profunda femoris (APF) and superficial femoral artery (AFS) are frequently involved. After a slightly curved, longitudinal approach, the vascular axis is dissected, with mobilization of the lymph node package medially. The AFC is opened longitudinally and the incision is passed into the AFP if necessary. In the endarterectomy that follows, the atherosclerotic plaque is peeled out, leaving only the adventitia as the vessel wall. A distally developing intima-media step is fixed by suturing to prevent dissection once blood flow is released. Closure of the longitudinal arteriotomy is performed with the insertion of a patch to avoid stenosis from a direct suture. If TEA of both the APF and AFS outlets is necessary, a femoral fork transposition can be performed if the anatomy is favorable. In the same session, hemodynamically relevant stenoses of the in- and outflow vessels are repaired retrogradely (iliac axis) or antegradely (femoropopliteal axis) via the inguinal approach using PTA or stent.
Bypass surgery
With few exceptions, bypass surgery is reserved for patients with stage III and IV PAVD and is the treatment of choice for long-stretch, femoropopliteal, and infragenicular occlusions. The following steps are part of performing a bypass surgery:
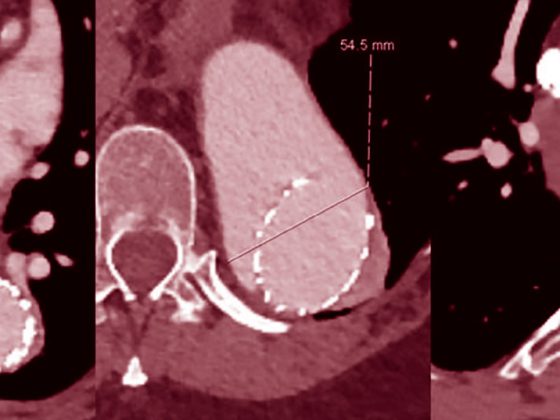
Preoperative imaging: angiography (conventional, CT, or MR) should be available to assess the in- and outflow vessels and to plan proximal and distal anastomosis. The most common location of proximal anastomosis of femoropopliteal bypass is AFC. If the anastomosis is performed distal to the tibiofibular trunk, the best “foot-bearing” connection is used. This means using preoperative imaging to decide which transtibial artery extends to the foot without relevant stenosis or occlusion. Accordingly, a medial or lateral approach is performed on the lower leg.
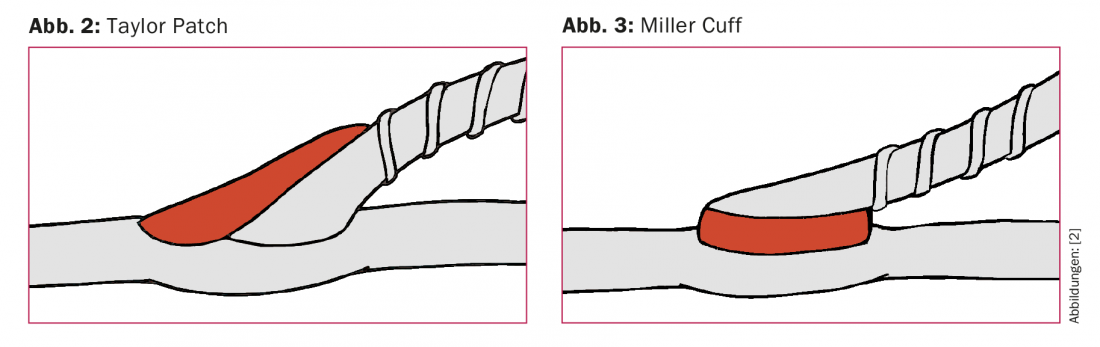
Planning Bypass Material: The conduit of choice is the ipsilateral autologous great saphenous vein (VSM). If it is too low in caliber or has already been used for another procedure, the contralateral VSM, parietal saphenous vein (VSP), or brachial veins may be used as alternatives. If necessary, multiple vein segments can be assembled to form a composite bypass. In the case of femoropopliteal bypass with supragenicular connection to the P1 segment, the use of a prosthesis is recommended in the absence of VSM [10]. If the prosthesis is the only possible bypass material and the connection is infragenicular, a short vein segment should be interposed as a patch or cuff in the area of the distal anastomosis to improve the openness rate [11] (Figs. 2 and 3).
Vein harvesting: Preoperatively, the course of the vein is marked sonographically. If the VSM is ipsilateral, the incision for vein harvesting also provides access to the supra- or infragenicular popliteal segment for anastomosis.
“Reversed” vs. “Non-reversed”: If the decision is made to use the vein “reversed”, the removed segment is rotated and the valve opening now occurs in the arterial flow direction. The advantage here is that the venous valves do not have to be resected. The disadvantage, however, is that a narrower distal vein end is anastomosed to the large caliber artery proximally and vice versa.
If a “non-reversed” bypass is chosen, the valves are valvulotomized after vein harvesting. This can be done angioscopically to simultaneously assess the vein endoluminally (thrombus buildup, wall sclerosis).
A special situation exists with in situ bypass. Here, the VSM is left in its fascial duplication and the preoperatively marked side branches are ligated via small incisions. The proximal and distal vein ends are mobilized sufficiently wide for arterial connection. Here, too, a valvulotomy is necessary.
There is no clear preference in the literature for any of the techniques described. In our hospital, bypass is usually performed in a “non-reversed” technique after prior angioscopically controlled valvulotomy along the vessel axis.
Bypass course: A distinction is made between the anatomical (orthotopic) and extraanatomical bypass course. If possible, the femoropopliteal bypass should be orthotopic in the course of the native vessel axis. It is important to prevent torquing or kinking of the distally directed vein. Extraanatomic bypasses often run subcutaneously and away from the actual vascular axis. Examples include axillofemoral bypass or crossover bypass for aortoiliac occlusion. These are usually patients with high perioperative risk, an unresolved infectious situation in the course of the vascular axis, or multiple prior surgeries.
Anastomoses: Typically, the proximal and distal anastomoses are created in an end-to-side (E/S) configuration. In this procedure, the end of the vein is sutured into the artery that has been arteriotomized longitudinally. The advantage is that antegrade and retrograde perfusion of proximal and distal collaterals is still maintained.
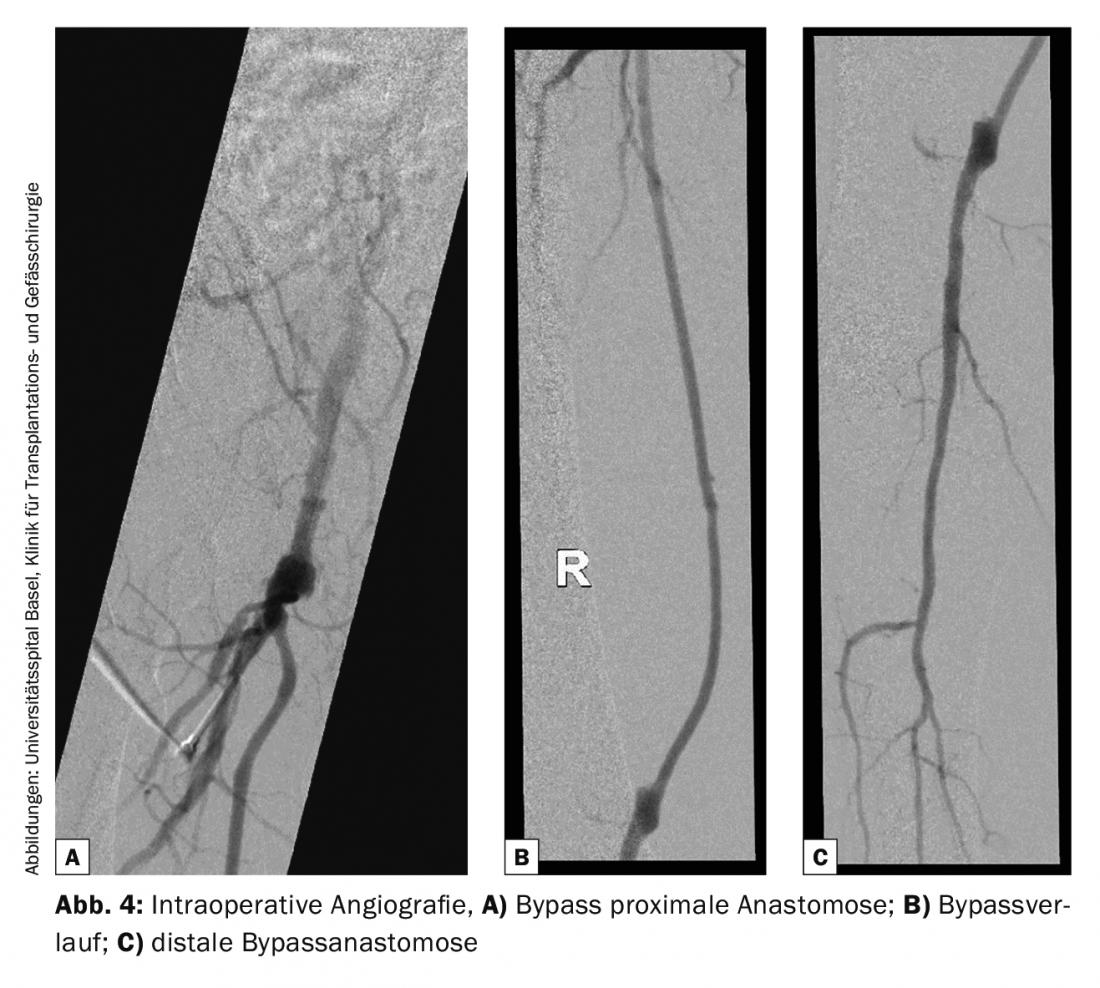
Bypass control: The intraoperative control of the bypass is performed on the one hand with the Doppler device and on the other hand angiographically to assess the anastomoses as well as the course of the bypass and the run-off situation at the lower leg. Angiography is not standard in all clinics (Fig. 4).
Postoperative management: Postoperative bypass control is performed by duplex sonography at three, six, and twelve months, and annually if bypass function is good. With regard to platelet inhibition and oral anticoagulation after bypass, there are several treatment approaches. The Dutch BOA study showed that there was no significant difference between Aspirin® and Marcoumar® in the rate of infragenicular bypass opening. However, in a subgroup analysis, patients with a venous conduit showed a better openness rate with oral anticoagulation, whereas patients with prosthetic bypasses had a better outcome with antiplatelet therapy [12].
In our clinic, patients with a distal bypass connection up to and including the truncus tibiofibularis usually receive Aspirin®, unless there is already oral anticoagulation due to another indication. When a venous bypass with a crural or pedal distal connection is created, patients are orally anticoagulated. All patients with prosthetic bypasses receive Aspirin® or Plavix®, if necessary in addition to pre-existing anticoagulation.
Take-Home Messages
- PAVD is often associated with CHD and CVI. Decreased ABI is associated with increased cardiovascular mortality.
- While stage I and II represent a non-critical circulation situation, stage III and IV can lead to limb loss if left untreated.
- Whether primary endovascular or primary surgical therapy is performed depends on the location and extent of the lesion, general condition, perioperative risk, patient life expectancy, and presence of a good quality vein (bypass device).
- Surgical techniques for rehabilitation of PAVD include thromboendarterectomy (TEA) and bypass grafting for long-segment occlusion and critical perfusion. If necessary, the two procedures are combined. If necessary, catheter-based revascularization of the in-flow and out-flow vessels is performed in the same session.
- Patients with crural or pedal venous bypass should receive oral anticoagulation postoperatively, and patients with prosthetic bypasses should receive single or dual antiplatelet therapy.
Literature:
- Donnelly R, Powell J: Epidemiology and risk factor management of peripheral arterial disease. In: Vascular and Endovascular Surgery, 5th Edition. Edinburgh: Saunders Elsevier, 2014: 1-15.
- Owens C: Atherosclerosis. In: Rutherford’s Vascular Surgery, Volume 1, 8th Edition. Philadelphia: Saunders Elsevier 2014: 66-77.
- McKenna M, Wolfson S, Kuller L: The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis 1991; 87: 119-128.
- Fowkes F, et al: Edinburgh Artery Study: Prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol 1991; 20: 384-392.
- Newman AB, et al: Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Heart Study (CHS) Collaborative Research Group. Circulation 1993; 88: 837-845.
- Bhatt DL, et al: International prevalence, recognition and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006; 295: 180-189.
- Norgren L, et al: Inter-Society Consensus for the management of peripheral Arterial Disease (TASC II). J Vasc Surg 2007; 45: 5-67.
- Aboyans V, et al: 2017 ECS Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). European Heart Journal 2018; 39: 763-816.
- Adam AJ, et al: Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 2005; 366: 1925-1934.
- Klinkert P, et al: Saphenous vein versus PTFE for above-knee femoropopliteal bypass. A review of the literature. Eur J Vasc Endovasc Surg 2004; 27: 357-362.
- Griffiths GD, et al: Randomized clinical trial of distal anastomotic interposition vein cuff in infrainguinal polytetrafluoroethylene bypass grafting. Br J Surg 2004; 91: 560-562.
- Dutch BOA trial: Efficacy of oral anticoagulants compared with aspirin after infrainguinal bypass surgery (The Dutch Bypass Oral Anticoagulants or Aspirin Study): a randomised trial. Lancet 2000; 355: 346-351.
CARDIOVASC 2018; 17(5): 22-25