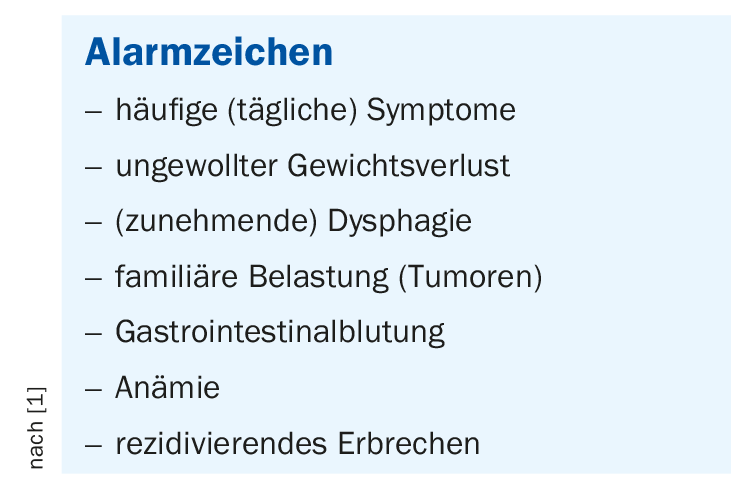
In patients over 50 years of age with reflux symptoms or if alarm signs are present, an endoscopic examination should be performed directly. In most other cases, a PPI therapy trial can be performed combined with support for lifestyle modification. If symptoms persist, endoscopic examination is indicated, as well as 24-h impedance pH-metry if necessary.
Gastroesophageal reflux disease (GERD) is a pathological reflux of gastric juice or duodenal contents into the esophagus without vomiting. The following complaints are subsumed under the collective term GERD [1]:
- Erosive reflux esophagitis
- Non-erosive reflux disease (NERD).
- Reflux hypersensitivity
- (formerly: hypersensitive esophagus)
- Functional reflux complaints
- Extraesophageal manifestations
- Complications of GERD
- Barrett’s esophagus
Typical symptoms of reflux syndrome include heartburn, regurgitation and acid regurgitation. Other common manifestations include upper abdominal pain and sleep disturbances due to nocturnal reflux. Atypical symptoms include globus sensation and throat clearing. Visible inflammation of varying severity (Los Angeles grades A through D) and peptic stenosis may develop in the esophagus. Common causes include dysfunction of the lower esophageal sphincter closure function, esophageal clearance, or gastric emptying [2]. During the anamnesis, in addition to the type of symptoms and frequency, correlations to the factors nutrition (e.g. volume of a meal, energy density, eating speed) and stress can be queried [3]. There is no diagnostic gold standard for GERD, but a work-up algorithm proposed by gastroenterologists provides guidance.
Diagnosis is not trivial
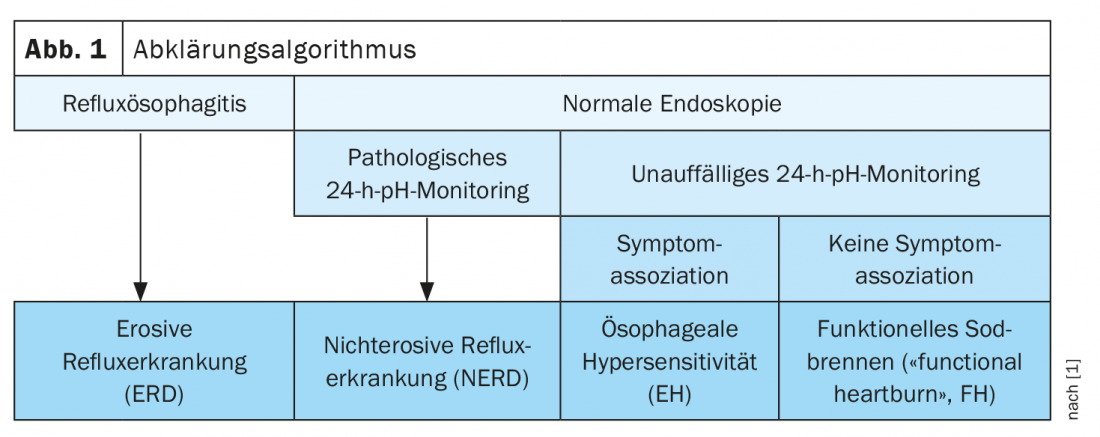
In patients with reflux symptoms who are older than 50 and/or show alarm signs (box) , it is recommended to perform gastroscopy directly [1]. In most other patients, PPI therapy can be tried first, as well as counseling regarding lifestyle changes (e.g., weight loss) [1]. In case of lack of response to empiric PPI therapy and for an evaluation of possible complications and differential diagnoses, endoscopic examination is indicated [3]. About half of all reflux patients develop esophagitis, and this is a benign complication [2]. The extent of damage in the esophagus can only be determined by endoscopy, because there is no significant correlation between severity and frequency of symptoms and lesions in the esophagus [4]. High-grade esophagitis (Los-Angeles classification grade C or D), Barrett’s esophagus, or peptic strictures are evidence of the presence of reflux disease. Barrett’s esophagus is a potentially malignant complication that is considered a precancerous condition for the development of adenocarcinoma of the distal esophagus (Barrett’s carcinoma). If the endoscopic findings are unremarkable, ambulatory reflux monitoring can be performed. For this purpose, there is on the one hand the method of “wireless ph monitoring” (Bravo capsule). An acquisition time of up to 96 hours increases diagnostic confidence [3]. Endoscopy is required for placement. On the other hand, 24h-impendance pH-metry can be performed. This allows specification of the type of refluxes (liquid, gaseous, mixed, acidic, non-acidic). Depending on the case, 24-h impendance pH-metry is performed without PPI (gold standard for primary diagnosis, preoperatively before surgery=fundoplicatio) or with PPI (refractory reflux symptoms, extraesophageal symptoms) [3,5]. The results of 24-h ph monitoring allow differentiation into nonosseous reflux disease (NERD), esophageal hypersensitivity, or functional heartburn [1] (Fig. 1).
Therapy monitoring very important
Drug treatment may include locally acting substances such as antiazides (e.g., Alucol, Rennie, Sucralan), alginate (e.g., Gaviscon), or mucoprotectants (e.g., Ziverel, Sucralan). In some cases, histamine H2 receptor blockers are helpful. Proton pump inhibitors (PPIs), which have been on the market for many years, have proven to be the most effective [1]. Standard PPI therapy consists of 40 mg omeprazole (1×/day) for a period of 6-8 weeks [3]. It should be taken 30 minutes before a meal. If PPI in normal dose and lifestyle change do not lead to relief of symptoms, the following options are available: Doubling the PPI dose, changing the PPI (e.g., dual release PPI), combining PPI and H2 receptor blocker (especially for nocturnal symptoms), combining PPI and alginate/mucoprotectants, or a combined use of these methods. In terms of lifestyle changes, in addition to weight reduction, avoidance of excessive food intake, stress reduction, and smoking cessation have been shown to alleviate symptoms [3]. When taking meals, in addition to a small portion size, make sure you take enough time to eat and chew your food well. In overweight people, weight loss can lead to a decrease in reflux symptoms by reducing pressure in the abdomen. Exercise and sport not only serve to control weight, but endurance training of low to moderate intensity also strengthens the diaphragm and promotes gastric emptying. Another lifestyle factor relates to stress reduction, stress has been shown to increase the sensitivity of the esophageal lining to reflux. Quitting smoking can also reduce reflux activity. In case of nocturnal reflux symptoms, the head end of the bed should be raised and food should be avoided until at least two hours before the night’s rest.
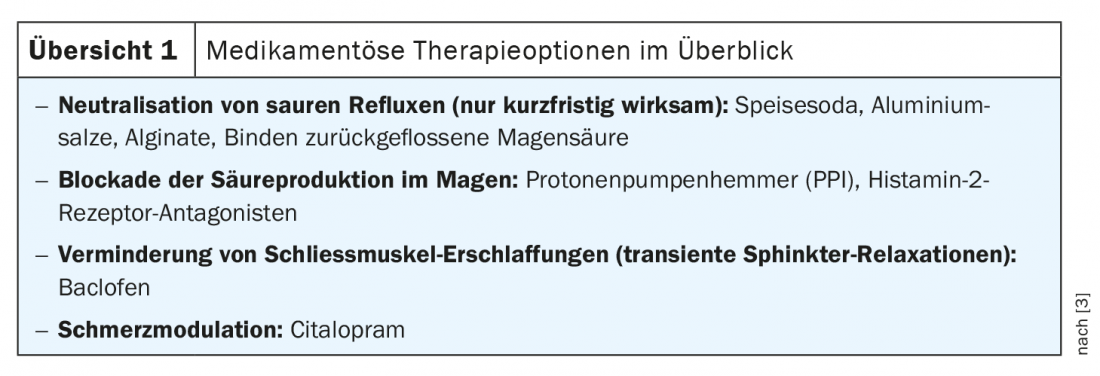
If drug treatment options have been exhausted, surgical intervention may be considered. Endostim® is an electrostimulation of the sphincter muscle between the esophagus and the stomach. For this purpose, two electrodes are implanted as subcutaneous pacemakers in the distal esophagus. Linx® refers to a mechanical closure of the gastroesophageal junction by a chain of titanium-encapsulated permanent magnets [1,3].
Literature:
- Burri E: Reflux disease, PD Dr. med. Emanuel Burri, Kantonsspital Baselland. medArt19, 18.06.2019.
- Taubert D, Schömig E: Gastrointestinal diseases, chapter 20, pp 333-345, in Pharmacotherapy Clinical Pharmacology: Lemmer B, Brune K: 2004: Springer, 12th edition.
- Lengliger J: Gastroesophageal reflux disease. Johannes Lenglinger, MD, Inselspital Bern. FOMF Basel, 29.01.2020.
- Labenz J, Labenz Ch: Reflux disease: PPI not always first choice, Pharmazeutische Zeitung, May 02, 2019. www.pharmazeutische-zeitung.de
- Gyawali CP, Fass R: Management of Gastroesophageal Reflux Disease. Gastroesophageal Reflux Diseas 2018; 154(2): 302-318.
HAUSARZT PRAXIS 2020; 15(10): 39-40