Various topical preparations are available for the treatment of seborrheic dermatitis in the capillitium area. Ketoconazole 1-2% is often used, which, among other things, leads to a reduction in Malassezia spp . colonization and alleviates symptoms. However, relapse often occurs after treatment is discontinued. Shampoo containing selenium disulfide has also been shown to be effective for mild to moderate seborrheic dermatitis. A recent study investigated the effects of a two-step treatment consisting of ketaconazole followed by selenium disulfide, with a particular focus on changes in the scalp microbiome.
Approximately 5% of the general adult population is affected by seborrheic dermatitis, with a higher prevalence in immunocompromised patients and those with neurologic disease [1,2]. Classic clinical features include erythematous plaques with mild pityriasiform scaling. The foci of inflammation occur particularly in the areas of the skin rich in sebaceous glands. The efflorescences may confluence and be accompanied by varying degrees of pruritus. Depending on the localization, some peculiarities appear. In the area of the capillitium, scarcely sharply defined redness with dense, non-adherent scaling is typical, although there is usually no crossing of the hairline boundaries and usually only minor itching.

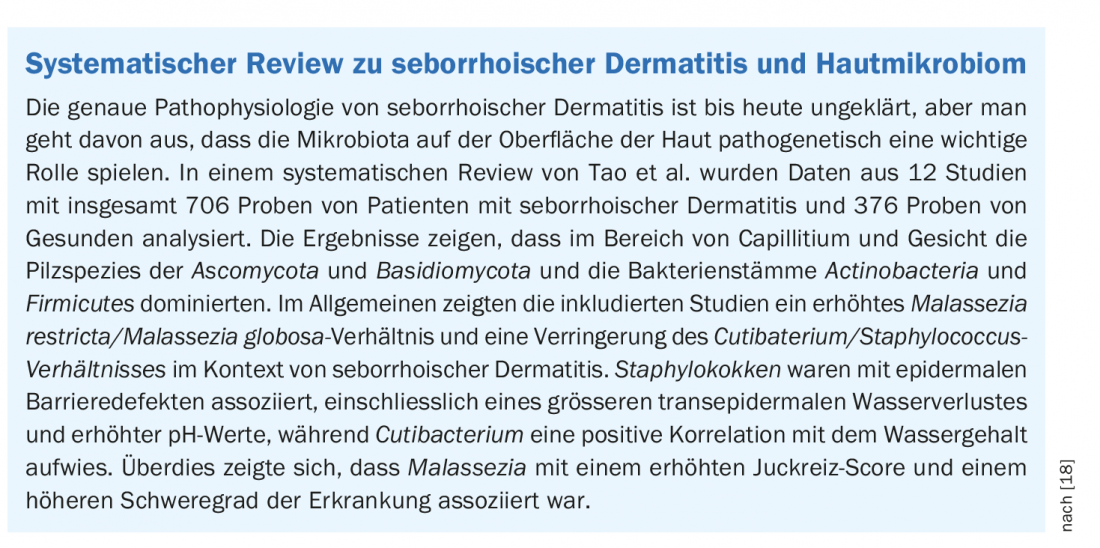
Pathophysiological role of the microbiota as a therapeutic target.
Various external and internal factors play a role in the etiopathogenesis of seborrheic dermatitis. There are changes in sebaceous gland activity, epidermal barrier function and fungal colonization on the skin surface, resulting in inflammation. Lipophilic Malassezia yeastsappear to play a key role in the disease process. Malassezia species, especially M. restricta show cytotoxic effects on keratinocytes in vitro, suggesting an active role in accelerated desquamation [10]. In addition, bacterial alterations of the skin microbiota may be involved in the pathogenesis of seborrheic dermatitis [3–5].
Current treatment options include topical applications of antifungal and anti-inflammatory preparations [6]. Ketoconazole is a fungistatic agent that leads to a reduction of Malassezia restricta, M. globosa, and M. furfur without inhibiting S. epidermidis or S. aureus [7]. In vivo, treatment with ketoconazole 1-2% has been shown to result in short-term symptom relief accompanied by a reduction in Malassezia spp. colonization, supporting the notion that this fungal species plays a pathophysiologically important role in seborrheic dermatitis [8,9]. However, relapse of symptoms often occurs after discontinuation of ketaconazole treatment [10,11].
Another remedy that has proven effective against the scaling that occurs in the context of mild seborrheic dermatitis is selenium disulfide shampoo. In addition to antifungal properties against Malassezia furfur , inhibition of staphylococcal colonization on the epidermis was also observed in vitro [12,13]. Moreover, salicylic acid contained in selenium disulfide shampoo has keratolytic activity, which promotes reduced dandruff on the skin.
Study proves benefit of maintenance therapy with selenium disulfide shampoo
In the present study, after 4 weeks of initial treatment with ketoconazole, 8 weeks of maintenance therapy with selenium disulfide shampoo or vehicle subszance was performed [14,15]. To investigate the effects of treatment on the capillitium microbiome, “next-generation sequencing” and qPCR* quantification were performed with respect to Staphylococcus, Cutibacterium, and Malassezia, the three main microbial markers of scalp seborrheic dermatitis [16]. A total of 68 individuals with mild to moderate seborrheic dermatitis were included in the study. Initially, treatment with 2% ketoconazole was administered over the one-month period, and either 1% selenium disulfide shampoo or vehicle was used during the subsequent two-month maintenance phase.
* PCR=Polymerase Chain Reaction
There were 31 subjects included in the active treatment arm (21 women, 10 men, mean age 40.2 years) and 37 in the vehicle control group (29 women, 8 men, mean age 42.2 years). Treatment with ketoconazole resulted in improvement of clinical symptoms including scaling and erythema. Moreover, an increase in the diversity of fungal species and a significant reduction in Malassezia spp . were observed. During the course of maintenance therapy, additional clinical improvement was achieved in the selenium disulfide group compared with the vehicle control group, with a significant reduction in scaling at day 84. This effect was accompanied by low levels of Malassezia spp . and substantial reductions in Staphylococcus spp .
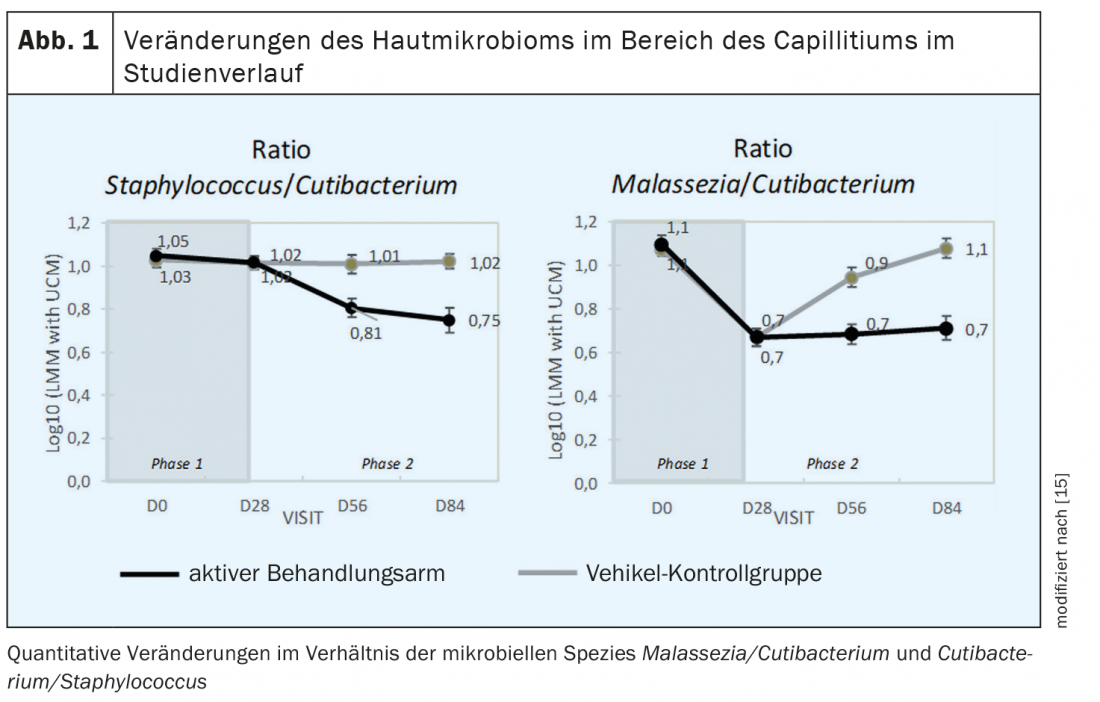
The ratio of Malassezia/Cutibacterium spp. was significantly lower after ketoconazole treatment compared to baseline (t=0) and remained at similar levels in the active treatment arm during the maintenance phase, while in the vehicle control group this ratio shifted upward and approached the value at baseline (Fig.1). The ratio of Staphylococcus/Cutibacterium from day 28 to day 84 decreased significantly only in the active treatment arm (p<0.05) (Fig. 1) . This is an interesting finding, as previous therapy studies on seborrheic dermatitis on the scalp usually focused only on colonization with the yeast Malassezia spp , while the bacterial microflora was not addressed. [12,17].
Conclusion
The results of this study confirm that the use of a selenium disulfide shampoo for several weeks following ketoconazole treatment in seborrheic dermatitis has an additional benefit on the clinical symptoms as well as on the normalization of the scalp microbiome [14,15]. Evidence suggests that Staphylococcus spp. plays an important role in the pathophysiology of seborrheic dermatitis. Overall, these study results potentially open a new treatment pathway for the prevention of recurrence in patients with mild-to-moderate capillitial seborrheic dermatitis.
Congress: European Academy of Dermatology and Venereology
Literature:
- Gaitanis G, et al: The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev 2012; 25(1): 106-141.
- Hay RJ: Malassezia, dandruff and seborrheic dermatitis: an overview. Br J Dermatol 2011; 165(Suppl 2): 2-8.
- Park T, et al: Collapse of human scalp microbiome network in dandruff and seborrheic dermatitis. Exp Dermatol 2017; 26(9): 835-838.
- Soares RC, et al: Malassezia intra-specific diversity and potentially new species in the skin microbiota from Brazilian healthy subjects and seborrheic dermatitis patients. PLoS One 2015; 10(2):e0117921.
- Tanaka A, et al: Comprehensive pyrosequencing analysis of the bacterial microbiota of the skin of patients with seborrheic dermatitis. Microbiol Immunol 2016; 60(8): 521-526.
- Borda LJ, Perper M, Keri JE: Treatment of seborrheic dermatitis: a comprehensive review. J Dermatolog Treat 2019; 30(2): 158-169.
- Leong C, et al: In vitro efficacy of antifungal agents alone and in shampoo formulation against dandruff-associated Malassezia spp. and Staphylococcus spp. Int J Cosmet Sci. 2019; 41(3): 221-227.
- Pierard GE, et al: Prolonged effects of antidandruff shampoos – time to recurrence of Malassezia ovalis colonization of skin. Int J Cosmet Sci 1997; 19(3): 111-117.
- Pierard-Franchimont C, et al: Effect of ketoconazole 1% and 2% shampoos on severe dandruff and seborrheic dermatitis: clinical, squamometric and mycological assessments. Dermatology. 2001; 202(2): 171-176.
- Donnarumma G, et al: Analysis of the response of human keratinocytes to Malassezia globosa and restricta strains. Arch Dermatol Res 2014 ;306(8): 763-768.
- Ortonne JP, et al: Efficacious and safe management of moderate to severe scalp seborrhoeic dermatitis using clobetasol propionate shampoo 0.05% combined with ketoconazole shampoo 2%: a randomized, controlled study. Br J Dermatol 2011; 165(1): 171-176.
- Zani MB, et al: Ketoconazole does not decrease fungal amount in patients with seborrhoeic dermatitis. Br J Dermatol 2016; 175(2): 417-421.
- Schmidt A, Rühl-Hörster B: In vitro susceptibility of Malassezia furfur. Drug Research 1996; 46(4): 442-444.
- Massiot P, et al: Continuous clinical improvement of mild to moderate seborrheic dermatitis together with rebalancing of the full scalp microbiome using a Selenium Disulfidebased shampoo after an initial treatment with Ketoconazole: results from a randomized, double-blind, clinical trial. Abstract N°: 776, EADV Annual Meeting, 29.9.-2.10.21
- Massiot P, et al: Continuous clinical improvement of mild-to-moderate seborrheic dermatitis and rebalancing of the scalp microbiome using a selenium disulfide-based shampoo after an initial treatment with ketoconazole. J Cosmet Dermatol 2021 Aug 20. doi: 10.1111/jocd.14362. epub ahead of print.
- Grimshaw SG, et al: The diversity and abundance of fungi and bacteria on the healthy and dandruff affected human scalp. PLoS One 2019; 14(12): e0225796.
- Kamamoto CSL, et al: Cutaneous fungal microbiome: Malassezia yeasts in seborrheic dermatitis scalp in a randomized, comparative and therapeutic trial. Dermatoendocrinol 2017; 9(1):e1361573.
- Tao R, Li R, Wang R: Skin microbiome alterations in seborrheic dermatitis and dandruff: A systematic review. Exp Dermatol 2021; 30(10): 1546-1553.
DERMATOLOGIE PRAXIS 2022; 32(1): 46-47 (published 10.2.22, ahead of print).