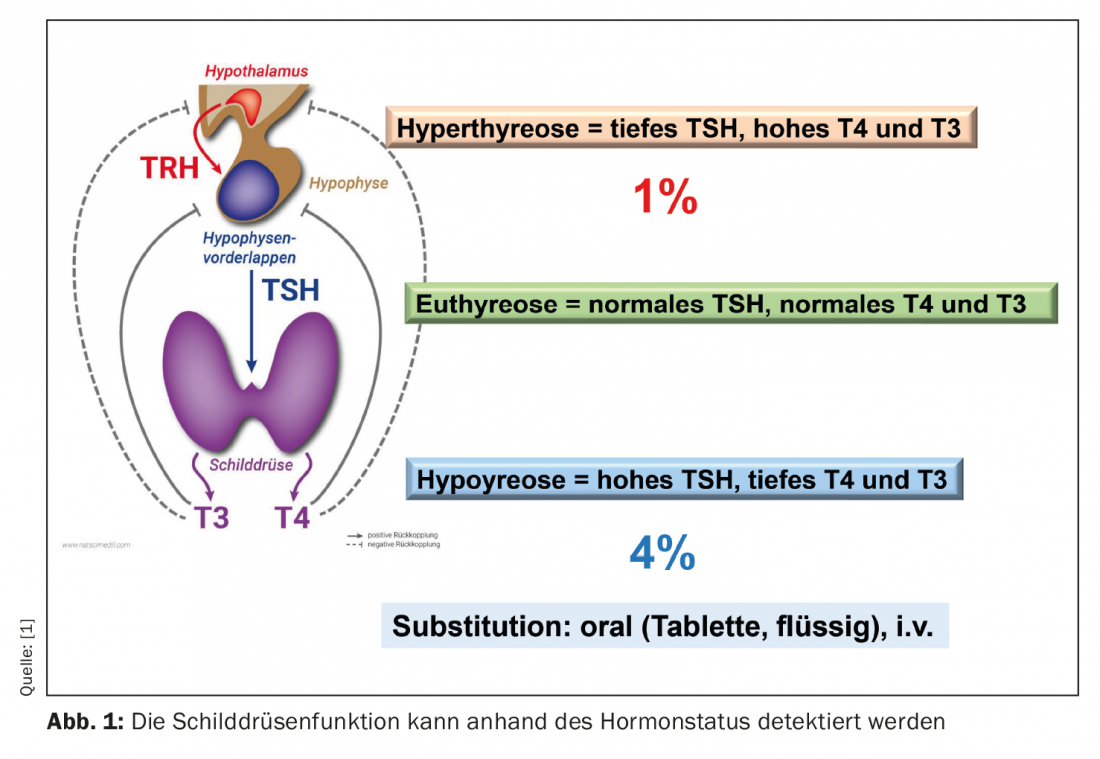
Hypothyroidism is a common condition that has significant effects on the body’s metabolic processes. Impaired performance is a result of deficient hormone production by the thyroid gland. Accordingly, thyroid hormone replacement therapy is indicated.
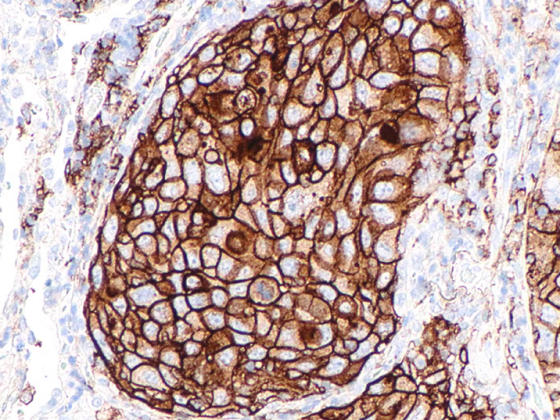
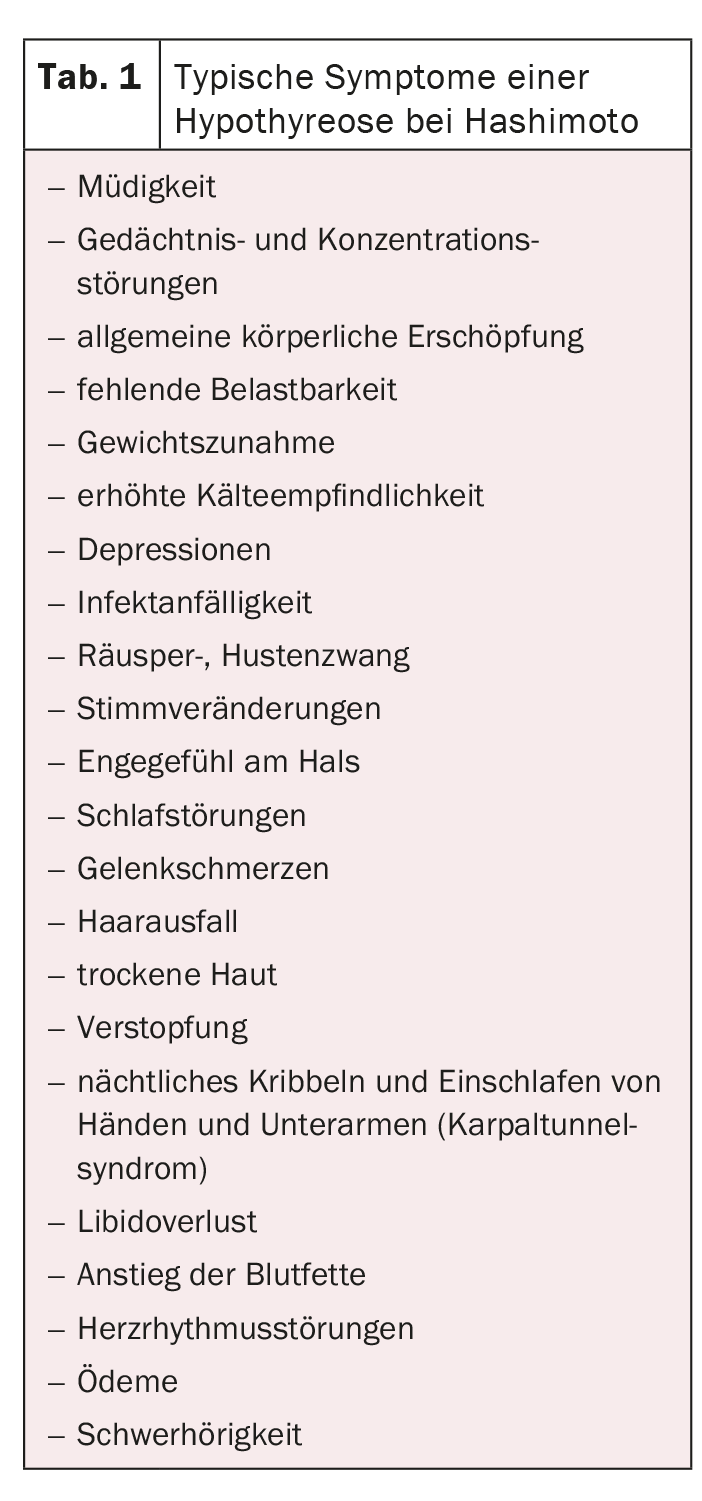
We speak of manifest hypothyroidism when the TSH level is elevated, but T4 and T3 are reduced. Clinical signs manifest as bradycardia, hypertension, hyporeflexia, hypothermia, a deep, hoarse voice, and a pale yellowish skin coloration. In 41% of cases, the cause can be traced back to autoimmune thyroiditis, as Prof. Roger Lehmann, MD, Zurich, Switzerland, pointed out. First described by Hakaru Hashimoto in 1912, the disease is characterized by chronic inflammation of the thyroid gland. It is possible that at the beginning of the disease, due to inflammation, hyperfunction may be seen, which is called “hashitoxicosis”. In the further course, however, this always turns into hypothyroidism, since due to the destruction of the thyroid cells, sufficient hormones can no longer be produced and, in addition, these are often released in an uncontrolled manner. Immunopathogenetically, CD4+ T cells and their differentiations into Th1, Th2, Th17, and Treg play a particularly important role. Stimulation and production of B cells and plasma cells is the result, which form antibodies against the thyroid cells. In addition, lymphocytes, macrophages and cytokines such as interferon or TNF-α are activated. This increases the autoimmune process and leads to destruction of the thyroid gland. A genetic predisposition in combination with unfavorable external influences ensure the onset of the disease. Triggers include hormonal fluctuations – especially during pregnancy – high iodine intake, stress, infections, medications, or severe illness. Since almost all organs are affected by the metabolic disorder, the symptoms are very varied (Table 1) .
Antibody detection not always sufficient
Hashimoto’s is diagnosed by blood work and ultrasound. In the blood, the thyroid antibodies TPO-AK, TG-AK and TR-AK produced by the immune system are determined. In manifest disease, these values are elevated. However, 10-20% of affected individuals do not form antibodies, so ultrasound examination should always be performed. In addition, the hormones TSH, fT3 and fT4 are determined. In the case of hypofunction, the TSH value is above 2.0.
Improvement of complaints through hormone substitution
Therapy with thyroid hormones is indicated to alleviate symptoms. As a rule, monotherapy with the storage hormone L-thyroxine is started. The start should be with the expected maintenance dose. This is equivalent to 1.6 µg/kg bw and should be taken 30 minutes before breakfast. Older patients >60 years of age or those with CHD should be started on a reduced dose. After two weeks, a dose adjustment can be made with regard to fT4. The target value here is 14-16 nmol/l. After six weeks at the earliest, the TSH level can be monitored in the long-term. A target value of 0.5-2 µU/l should be aimed for here.
Congress: FomF UpDate Refresher
Source:
- General Internal Medicine, Update Refresher, 08/18/2021, Hyper- and Hypothyroidism, Roger Lehmann.
CARDIOVASC 2021; 20(3): 36 (published 8/9/21, ahead of print).