Numerous empirical studies confirm that there is a causal relationship between high LDL cholesterol levels and cardiac events. The current motto with regard to LDL cholesterol reduction is “the lower, the better”. In the current ESC/EAS dyslipidemia guidelines, target values have been significantly revised downward for certain high-risk groups. If statin therapy is not sufficient, ezetimibe or PCSK9 inhibitors may be added.
Cardiovascular disease is the second leading cause of death in Switzerland. High LDL cholesterol levels (LDL-C, “low density lipoprotein cholesterol”) are one of the most important risk factors that can be influenced, along with hypertension. Whereas congenital hypercholesterolemia is associated with a higher risk than acquired later in life [1]. Therefore, analogous to the “pack years” in smokers, the term “LDL cholesterol years” was introduced. The goal of lipid-lowering treatment is to reduce the risk of cardiovascular events as much as possible. New studies show that the lower the LDL-C, the lower the cardiovascular risk. Accordingly, there is no lowest LDL-C concentration limit below which cardiovascular risk does not decrease further. This has been incorporated into the 2019 revised ESC/EAS guidelines, with expert recommendations focusing on high-risk patients [1]. Prof. Dr. med. Franz R. Eberli, Chief Physician Cardiology, Stadtspital Waid und Triemli, Zurich, gave an up-to-date overview of the most important points.
ESC-SCORE for risk stratification
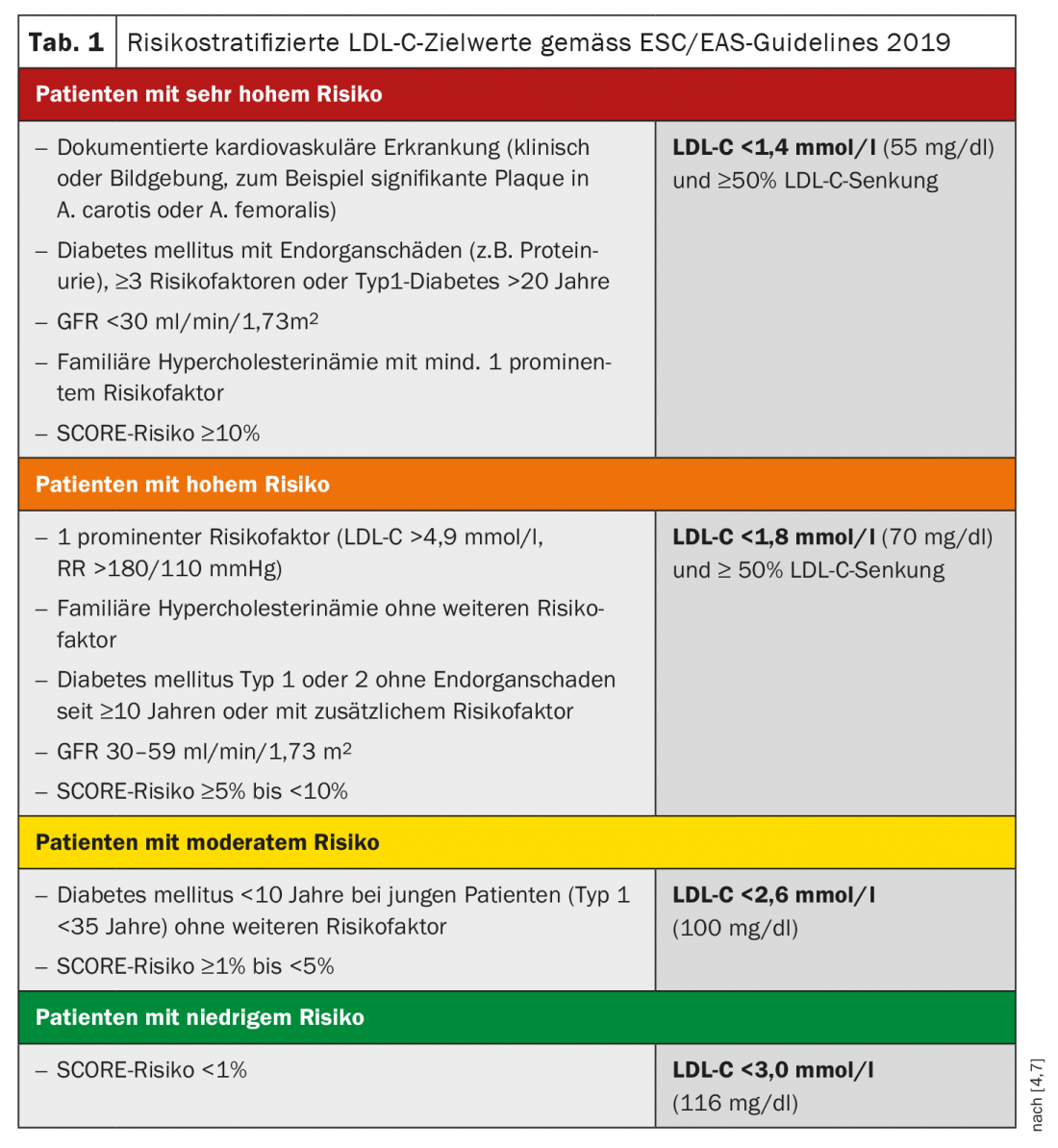
The ESC-SCORE (“systematic coronary risk estimation”) for cardiovascular risk stratification is available as an online tool and as a point table and gives the absolute 10-year risk in percent for a fatal atherosclerotic event (including sudden cardiac death) [8 .9]. LDL cholesterol target values for patients at very high risk were adjusted to <1.4 mmol/l and ≥50% reduction (Table 1) [1]. This treatment goal is most likely achievable with ezetimibe or anti-PCSK9 antibodies as an add-on to statin therapy, as current scientific evidence shows. Statins, however, remain highly valued for lipid management.
Statins still first choice
Statin therapy reduces cholesterol synthesis by inhibiting HMG-CoA reductase [10]. The intensity of LDL lowering varies depending on statin, dosage, and genetic predisposition. Atorvastatin, rosuvastatin, and pitavastatin are considered potent statins. All statins except pravastatin, rosuvastatin, and pitavastatin are metabolized hepatically via enzymes of the cytochrome P450 family [10]. In case of drug interactions or contraindications, lowering the dose or using another statin is recommended. In statin intolerance characterized by myopathy, a trial of therapy with low-dose pravastatin or fluvastatin is reasonable.
Combination with ezetimibe has evidence-based added benefit
Ezetimibe inhibits the absorption of cholesterol through the intestine. Studies have demonstrated the added benefit of ezetimibe combined with statin therapy compared with statin monotherapy in high-risk patients. For example, the IMPROVE-IT trial showed that ezetimibe 10 mg/d in addition to statin therapy 40 mg/d reduced the rate of cardiovascular events more than statin monotherapy in patients with acute coronary syndrome without increasing the rate of adverse events [2,3]. “It makes sense that if you don’t reach the target value with statins, add ezetimibe,” Prof. Eberli summarized [4]. This applies to patients who have had clinically manifest coronary artery disease or stroke, he said. The combination of statin plus ezetimibe is usually not only associated with an additional benefit for lipid lowering, but is associated with fewer side effects than a further increase in statin dose. In the case of high LDL-C values (>3.9 mmol/l), it is recommended to primarily treat with a combination preparation.
PCSK9 antibody as an alternative add-on option
If the target value cannot be reached with the combination therapy ezetimibe plus statins, an anti-PCSK9 antibody should be considered as an alternative supplement. PCSK9 inhibitors are agents that result in the inhibition of LDL receptor formation at the liver. However, the limitations of the Federal Office of Public Health currently do not allow a 1:1 implementation of the ESC/EAS recommendations for the prescription of PCSK9 inhibitors in Switzerland [1]. For evolocumab and alirocumab, reimbursement by the health insurance fund is only provided if the following LDL-C values cannot be achieved over at least three months with the maximum tolerated dosage of intensified LDL-C-lowering therapy with at least two different statins with or without ezetimibe (or ezetimibe with or without other lipid-lowering agents in the case of statin intolerance): In secondary prevention after a clinically manifest ischemic cardiovascular event due to atherosclerosis LDL-C. >2.6 mmol/l. For primary prevention LDL-C >5.0 mmol/L in heterozygous or homozygous familial hypercholesterolemia;
LDL-C >4.5 mmol/L in adults with severe heterozygous familial hypercholesterolemia with at least one of the following additional risk factors: diabetes mellitus, lipoprotein (a) >50 mg/dL or >120 nmol/L, and marked arterial hypertension.
That evolocumab has additional benefit on top of standard therapy in patients with stable coronary artery disease on future cardiovascular events was demonstrated in the FOURIER trial [5]. And in the ODYSSEY trial, alirocumab in addition to maximal statin therapy led to a 15% reduction in myocardial infarction, stroke, unstable angina, and cardiovascular-related death. [6]. The reduction in LDL-C by the PCSK9 inhibitors depends on the baseline level, Prof. Eberli explained. The lower the LDL-C can be lowered with statins, the more likely the target value can be reached with the addition of a PCSK9 inhibitor.
Source: FomF General and Internal Medicine
Literature:
- Riesen WF, et al: An annotated review of the AGLA. New ESC/EAS dyslipidemia guidelines. Swiss Med Forum 2020; 20(0910): 140-148.
- Giugliano RP, et al. (IMPROVE-IT): Circulation 2018 (10); 137(15): 1571-1582.
- DGK: Intensified lipid lowering with statin plus ezetimibe: who benefits most, 29.07.2019, www.kardiologie.org
- Eberli FR: Lipid therapy 2020. Prof. Franz R. Eberli, MD, FOMF 6/23-27/20.
- Sabatine MS, et al. (FOURIER): Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. NEJM 2017; 376(18): 1713-1722.
- Lüscher TF, et al: Modern lipid management. Cardiovasc Med 2020; 23:w02102. DOI: https://doi.org/10.4414/cvm.2020.02102
- Weingärtner O, et al: Commentary on the ESC/EAS guidelines (2019) on diagnosis and therapy of dyslipidemias. The Cardiologist 2020; 14: 256-266.
- EAPC: HeartScore, www.heartscore.org
- ESC: SCORE: European High Risk Chart, www.escardio.org/static_file/Escardio/Subspecialty/EACPR/Documents/score-charts.pdf
- Medix: Guideline: Hyperlipidemia, last revised: 07/2020, www.medix.ch
HAUSARZT PRAXIS 2021; 16(2): 18-19 (published 2/19-21, ahead of print).