Antibiotic resistance is an increasing global problem with significant consequences for the healthcare system. While antibiotics are indicated for complicated UTI, treatment without antibiotics may be considered for uncomplicated cystitis. Experts agree that it is important to avoid the untargeted use of antibiotics.
The most common pathogens of urinary tract infections include Escherichia coli; other Enterobacteriaceae, as well as other Gram-negative (e.g., pseudomonads) or Gram-positive (e.g., staphylococci, enterococci) bacterial strains, are found much less frequently. For some years now, an increased occurrence of germs that form resistances to different substance classes of antibiotics has been observed worldwide. This also affects antibiotic agents used in the treatment of urinary tract infections. In complicated courses, antibiosis is usually indicated, standardly used here are fosfomycin (3 g, single), nitrofurantoin (2× 100 mg, 5 days), trimethoprim/sulfamethoxazole (2×, 160/180 mg, 3 days). Prof. Dr. med. Martin Krause, Chief Medical Officer, Münsterlingen Cantonal Hospital, points out that the use of nitrofurantoin should be limited to one week due to the risk of side effects (pulmonary fibrosis) in the case of long-term use [1]. If it is uncomplicated cystitis, however, treatment without antibiotics can be considered, the speaker said. Exceptions are severe pain in the lumbar region, poor general health, evidence of pyelonephritis, or pregnancy.
Resistance level of Gram-negative pathogens has increased
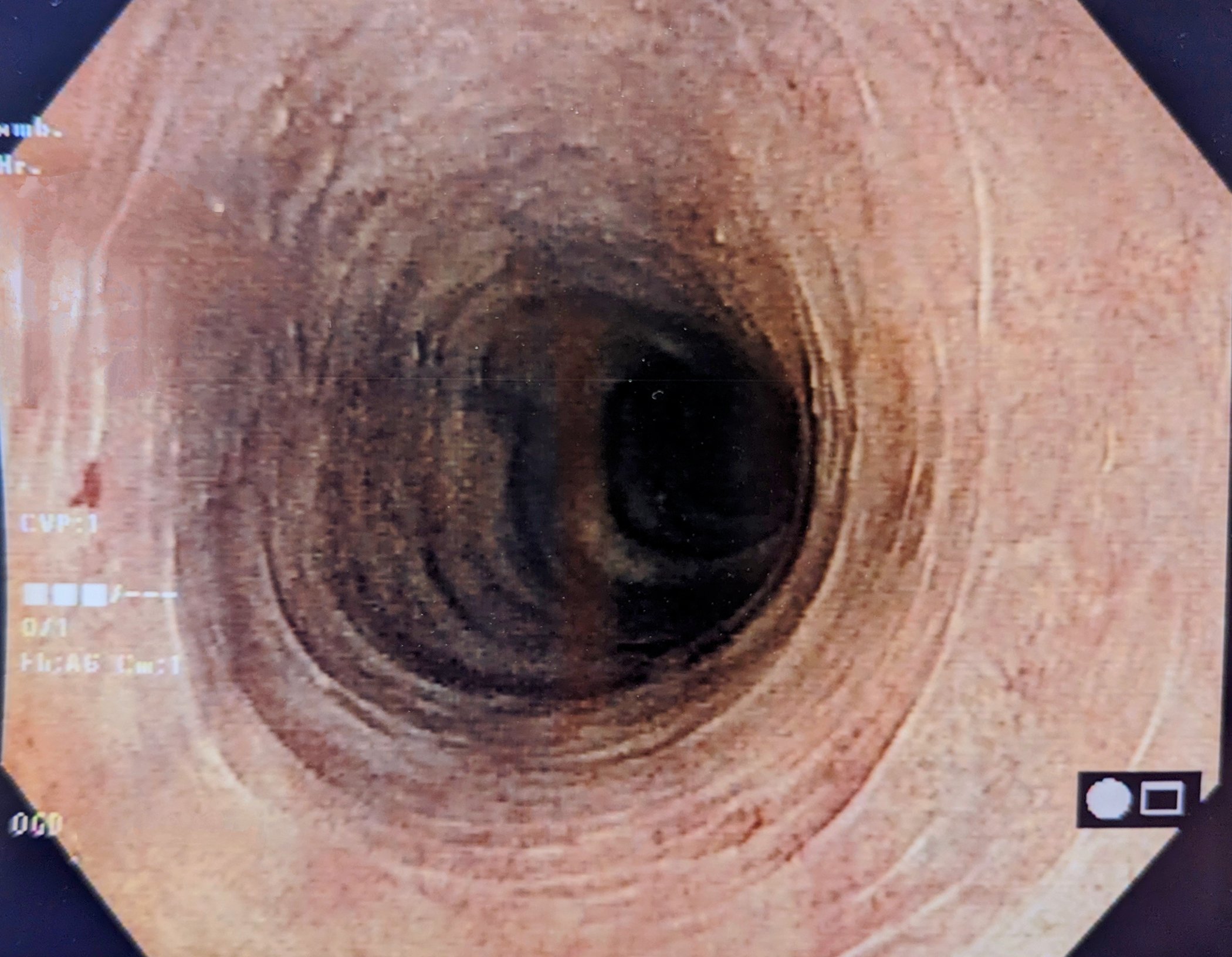
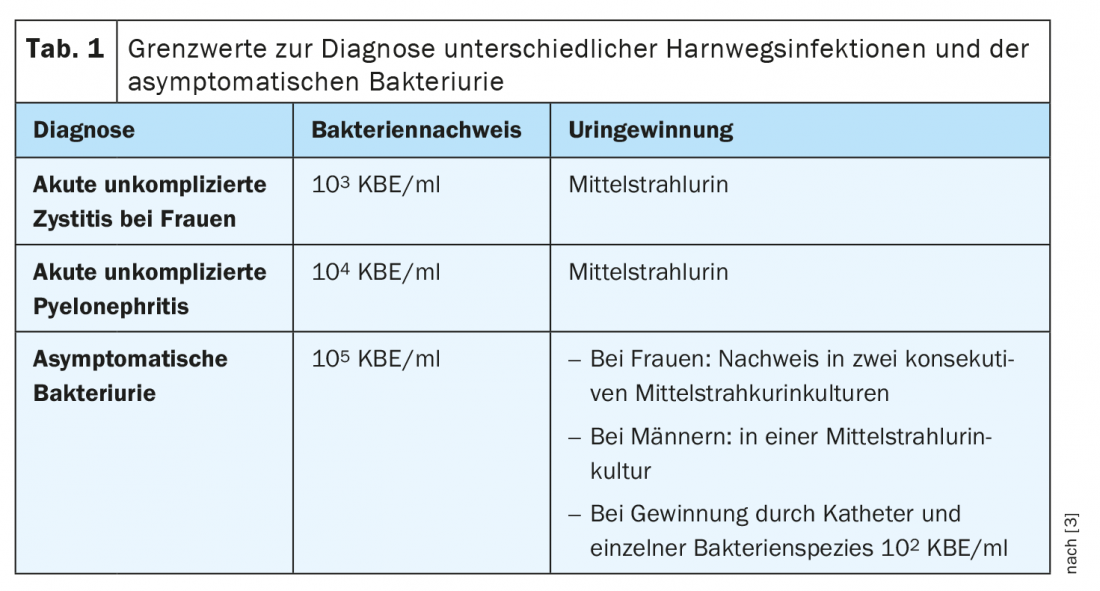
The gold standard for the diagnosis of a urinary tract infection is urine examination, including quantitative urine culture and its evaluation, if the patient has an appropriate history and typical symptoms. Pathogen counts as low as103-104CFU/ml can be clinically relevant with corresponding clinical symptoms if pure cultures are involved, i.e. only one type of bacteria of typical uropathogens (Tab. 1). Untargeted use of antibiotics is one of the main causes of the increase in resistance of UTI-associated bacteria [2]. This can be countered by more rapid and thorough pathogen diagnosis and resistance testing [3]. In view of the fact that the resistance level of Gram-negative pathogens (e.g. Escherichia coli) has increased significantly in recent years and that antibiotic resistance is an increasing global problem, the current S3 guideline of the Association of the Scientific Medical Societies in Germany (AWMF) aims to promote the rational use of antimicrobial substances in urinary tract infections and thus counteract the development of resistance. [2,3]. “The diagnosis of a urinary tract infection and the indication for antibiotic therapy should be made critically in order to avoid unnecessary therapies and reduce the development of resistance,” reads one of the expert recommendations in this set of rules.
Acute uncomplicated cystitis: Is antibiosis really necessary?
By definition, cystitis is present when acute symptoms are limited to the lower urinary tract, for example, new onset of pain on urination (alguria), imperative urination, pollakiuria, or pain above the symphysis [2]. Acute uncomplicated cystitis is often self-limiting. After one week, spontaneous remission occurs in about 30-50% of cases [3]. Therefore, the primary goal of therapy is to accelerate the resolution of symptoms. Whether to implement a treatment strategy using antibiotics or symptomatic therapy alone should be determined through participatory decision making with patients [3]. Offering nonantibiotic treatment is guideline-compliant and evidence-based for mild or moderate symptoms. In one study, 70% of patients were symptom-free after one week of primarily symptomatic treatment with ibuprofen; this proportion was only 10% higher with antibiotic treatment [4]. On the other hand, acute uncomplicated cystitis may also be the clinical precursor of pyelonephritis, which can be prevented by timely antibiotic therapy. This should definitely be taken into account during the inspection. The empirical findings are not entirely consistent. While some authors report an increased incidence of pyelonephritis with primarily symptomatic treatment with ibuprofen compared with immediate antibiotic treatment [4–6], data from controlled trials can be found in the literature indicating that no increased rate of pyelonephritis occurred in the placebo condition compared with the antibiotic treatment arm [7,8].
For symptomatic treatment, various phyototherapeutic preparations are available in addition to NSAIDs. Regarding the option of antibiotic therapy, it is important to consider that there is a correlation between the resistance rate and treatment failure. For example, it was found that therapy with cotrimoxazole resulted in about twice the cure and elimination rates within a week for susceptible Escherichia coli than for resistant Escherichia coli [3,9]. This means that with a resistance rate of 10-20%, a 5% or 10% higher failure rate must be expected based on the resistance situation alone. According to experts, an antibiotic is no longer suitable for empirical therapy of acute uncomplicated cystitis when the sensitivity rate falls below 80%. As part of the ARESC study (“Antimicrobial Resistance Epidemiological Survey”), an analysis of pathogen susceptibility to various antibiotics used to treat uncomplicated urinary tract infections was performed (box).

Pyelonephritis: antibiosis is required
To be distinguished from cystitis is pyelonephritis, in which acute typical symptoms such as flank pain are accompanied by a palpitating renal bed and/or fever >38°C, occasionally nausea and vomiting also occur [2]. Urine culture and resistance testing are usually useful in pyelonephritis, and ultrasonography may be useful to rule out congestion [1]. Antibiotics are always indicated in the presence of pyelonephritis and should be used as early as possible, in part to reduce the risk of renal damage [1,3].
Source: FOMF Internal Medicine 2020
Literature:
- Krause M: Urinary tract infections. Prof. Dr. med. Martin Krause, Chief Physician Medicine, Münsterlingen Cantonal Hospital. FOMF Internal Medicine Update Refresher (Livestream), Dec. 03, 2020.
- Kranz J, Schmidt S, Naber K: S3 guideline: uncomplicated urinary tract infections, Bayerisches Ärzteblatt 11/2017; 552-559.
- AWMF: Interdisciplinary S3 Guideline: Epidemiology, Diagnosis, Therapy, Prevention, and Management of Uncomplicated, Bacterial, Community-Acquired Urinary Tract Infections in Adult Patients. Update 2017. AWMF Register No. 043/044. Update 04/2017.
- Gágyor I, et al: Ibuprofen versus fosfomycin for uncomplicated urinary tract infection in women: randomised controlled trial. BMJ 2015; 351: h6544.
- Bleidorn J, et al: Symptomatic treatment (ibuprofen) or antibiotics (ciprofloxacin) for uncomplicated urinary tract infection?-results of a rndomized controlled pilot trial. BMC Med 2010; 26; 8: 30.
- Gágyor I, et al: Immediate versus conditional treatment of uncomplicated urinary tract infection – a randomized-controlled comparative effectiveness study in general practices. BMC Infect Dis 2012; 28; 12: 146.
- Christiaens TC, et al: Randomised controlled trial of nitrofurantoin versus placebo in the treatment of uncomplicated urinary tract infection in adult women. Br J Gen Pract 2002; 52(482): 729-734.
- Falagas ME, et al: Antibiotics versus placebo in the treatment of women with uncomplicated cystitis: a meta-analysis of randomized controlled trials. J Infect 2009; 58(2): 91-102.
- Raz R, et al: Empiric use of trimethoprim-sulfamethoxazole (TMP-SMX) in the treatment of women with uncomplicated urinary tract infections, in a geographical area with a high prevalence of TMP-SMXresistant uropathogens. Clin Infect Dis 2002; 34(9): 1165-1169.
- Naber KG, et al: Surveillance study in Europe and Brazil on clinical aspects and antimicrobial resistance epidemiology in females with cystitis (ARESC): Implications for empiric therapy. European Urology 2008; 54: 164-178.
HAUSARZT PRAXIS 2021; 16(1): 20-22 (published Jan 25-21, ahead of print).