A sudden change in weather can trigger symptoms in asthmatics and lead to exacerbations. Affected persons must therefore adapt to the different seasons and, if necessary, also change their medication. Because the worse the control, the more severe the symptoms.
In the fall – as well as in the spring – thunderstorms and storms can trigger an attack in asthmatics. Especially during pollen season, stormy weather can cause pollen to swirl very high, only to break up in the moist air and be pushed back to earth, where asthmatics breathe in the particles. Some patients also report respiratory problems and coughing that are triggered independently of pollen by the humid air, which is perceived as dense as a result.
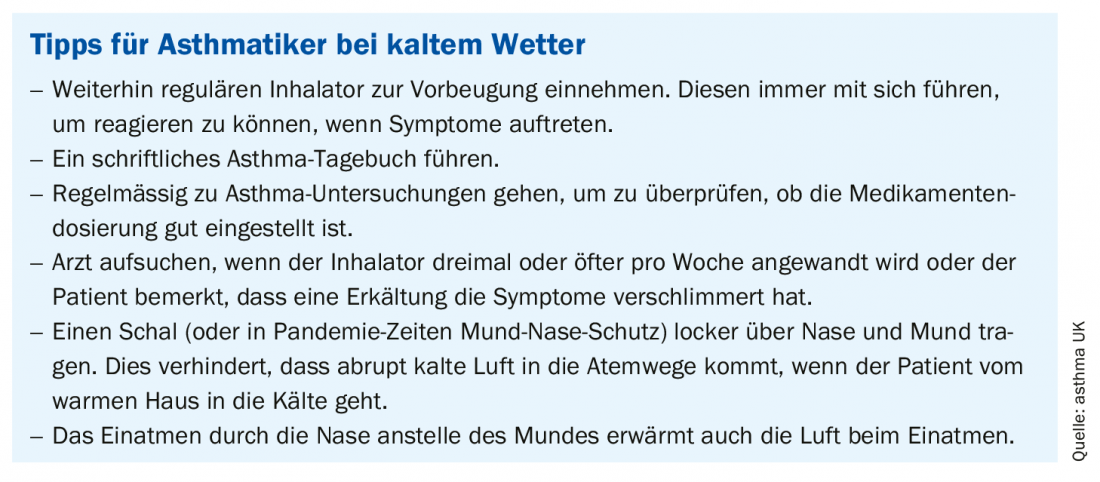
Although a change in weather from cold to warm can also have an impact, it is more common for falling temperatures to have a negative effect on asthmatics. Cold, humidity or even fog often trigger symptoms. Factors such as pollutant emissions and air pollution can have more severe effects in cold air. For many patients, it is therefore advisable to adjust their behavior and possibly also their medication starting in the fall. Some institutions issue recommendations to help asthmatics get through the cold season better ( box).
In order to find out to what extent patients with poor asthma control are more susceptible to cold weather-related respiratory symptoms than well-controlled patients, a Finnish research team led by Prof. Dr. Jouni J. K. Jaakkola, Center for Environmental and Respiratory Health Research, University of Oulu, conducted a cross-sectional study of nearly 2000 adult asthmatics living in Northern Finland via questionnaire, in which cold weather-related respiratory symptoms and questions about asthma control were asked [1]. About 40% of those approached answered the questions. The asthma control test (ACT) was defined using five questions (including occurrence of asthma symptoms, awakening due to asthma symptoms, use of rescue medication) and was divided into quartiles.
The key outcomes that researchers were interested in were five cold-related respiratory symptoms. To define these outcomes, the following questions were applied: “Do asthma symptoms occur more than normal in cold weather: almost always, frequently, occasionally, rarely, or never?” If the subject answered yes, a follow-up question asked about symptoms (shortness of breath, persistent cough, wheezing, mucus production, chest pain), and more than one response option could be given.
Previous studies have shown that breathing cold air can trigger adverse functional changes in the upper and lower airways. The sensitivity of asthmatics to cold air has been further suggested by clinical provocation studies using hyperventilation and cold dry air, during cold weather exercise testing, or when cold exposure is combined with high altitude. Wheezing, shortness of breath, coughing, and mucus production were considered typical symptoms of asthma. They were thought to indicate airway obstruction and an inflammatory process that may occur during an asthma exacerbation due to environmental factors, exercise, or inadequate medication. Therefore, it is likely that the presence of these symptoms is related to asthma control per se. On the other hand, patients with asthma with poor asthma control may be more sensitive to the adverse effects of respiratory stimuli, such as exposure to cold or tobacco smoke, write Jaakkola et al. Therefore, a combination of poor asthma control and unusually severe adverse environmental exposures could lead to a vicious cycle of intense cold weather symptoms.
The more symptoms, the worse the control
The evaluation revealed that the lower the asthma control, the higher the prevalence of symptoms associated with cold weather, from never to almost always (fig. 1) . Symptom prevalences were lowest in the highest ACT quartiles, representing the best asthma control. The Finnish study thus provided evidence that poor asthma control increases the risk of cold-related respiratory symptoms in both men and women. The relative effect of poor asthma control was strongest for cold weather-induced chest pain (adjusted prevalence ratio, aPR, 4.47 in men and 2.60 in women) and weakest for cough in men (aPR 1.10) and women (aPR 1.18) and shortness of breath (aPR 1.18) in women.

Therefore, the authors said, the study shows that asthmatics whose asthma is poorly controlled are more susceptible to cold-weather-related respiratory symptoms, and even a slight worsening of asthma control appears to increase the occurrence of cold-weather respiratory-related symptoms. This finding is important for asthmatics, he said, who should be informed about appropriate protection from cold weather and receive appropriate medications to reduce cold weather symptoms and avoid potentially more serious health effects. On the other hand, an increase in symptoms in asthmatics during the cold season may indicate worsening asthma control and suggest that the person is in immediate need of more comprehensive medical care.
Literature:
- Jaakkola JJK, et al: Respiratory Medicine 2016; 113: 1-7; doi: 10.1016/j.rmed.2016.02.005.
InFo PNEUMOLOGY & ALLERGOLOGY 2020; 2(3): 22-23.











