Malignancies of the male breast are very rare. In case of a suspected diagnosis, a careful clarification of clinical symptoms and anamnestic data is very important. Information sharing with the radiologist can be critical. Imaging examination is primarily performed by mammography, with sonography providing complementary information.
Benign and malignant tumors of the mammae of women were reported in detail in issues 6/2019 and 7/2019 of HAUSARZT PRAXIS. The criteria of imaging evaluation were discussed there and are also valid for masculine breast tumors. Spacious lesions of the male breast are relatively rare. In most cases, they are benign changes (gynecomastia, pseudogynecomastia), and breast carcinomas are relatively rare. For example, in the United States, the prevalence of male breast carcinomas is reported to be 1% of all malignant breast tumors [1]. This figure also applies to the other Western countries [2], with the rate of new cases increasing with increasing age per year. It is 0.1:100,000 for 35-year-olds and 11:100,000 for 85-year-olds. The main age of onset is between 61 and 65 years.
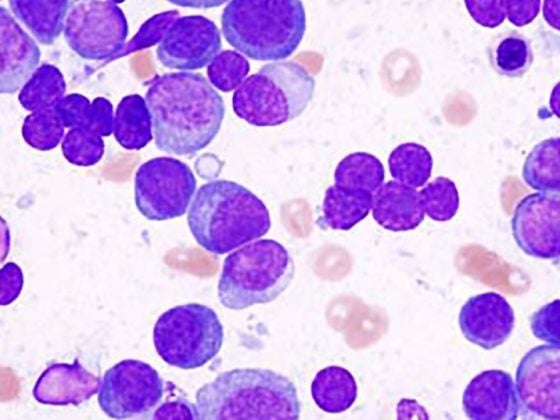
In principle, mainly three different entities can lead to space-occupying changes in the male breast (Table 1).
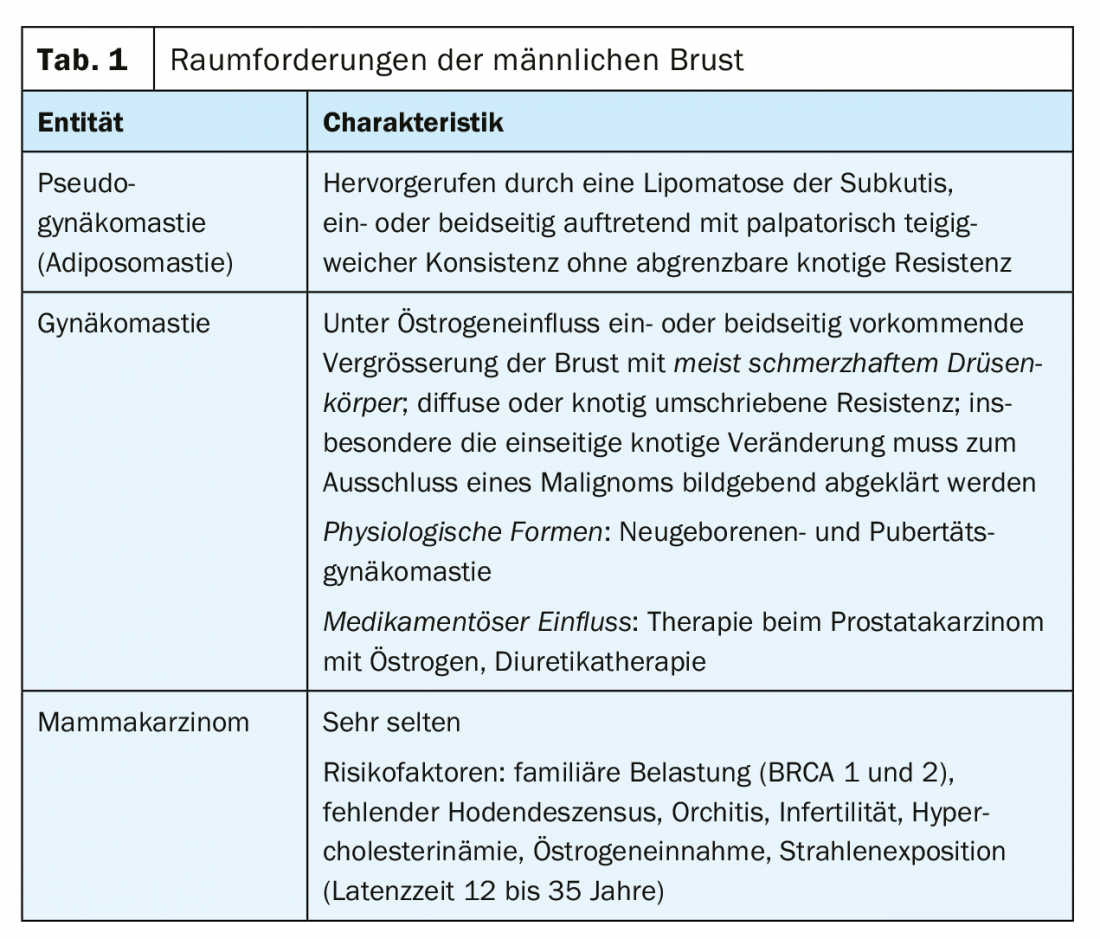
In addition to taking an exact medical history, especially with regard to drug therapies, relevant previous diseases and possible family history of tumors, clinical examinations and mammography are of decisive importance. Breast ultrasonography can provide complementary information on soft tissue structures and local lymph node status. For imaging purposes, the same malignancy criteria apply in men as in women. Adiposomastia (pseudogynecomastia) usually occurs in connection with increased fatty tissue of the body trunk, whereas true gynecomastia can be observed even without further fatty tissue increase of the body. In principle, enlargements of the male breast can trigger psychological problems of the patients, which then also lead to surgical corrections [4]. Surgical treatment of male breast carcinoma is inevitable, adjuvant therapy measures included. The prevalence of breast carcinoma in preexisting gynecomastia is reported to be 0.11 to 0.18%. Unilateral cases dominate.
Computed tomographic and magnetic resonance imaging examinations play no role in the primary diagnosis of male breast tumors.
Case studies
The cases listed here document the different causalities of male breast space-occupying lesions. History and clinical examination may already be indicative, but do not preclude imaging for definite verification of tissue proliferation.
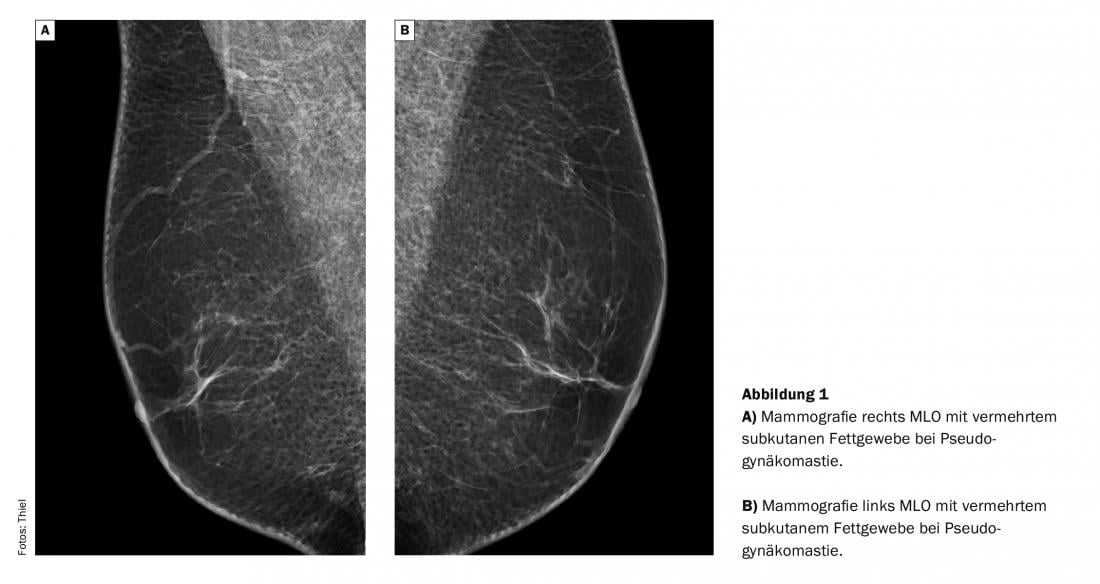
Case 1 (Fig. 1) shows mediolateral oblique (MLO) imaging of the right and left mamma (Figs. 1A and 1B) of a 68-year-old obese man in whom gynecomastia should be excluded. Disposing factors were not present, nor were there any pain symptoms with doughy-lipomatous palpation.
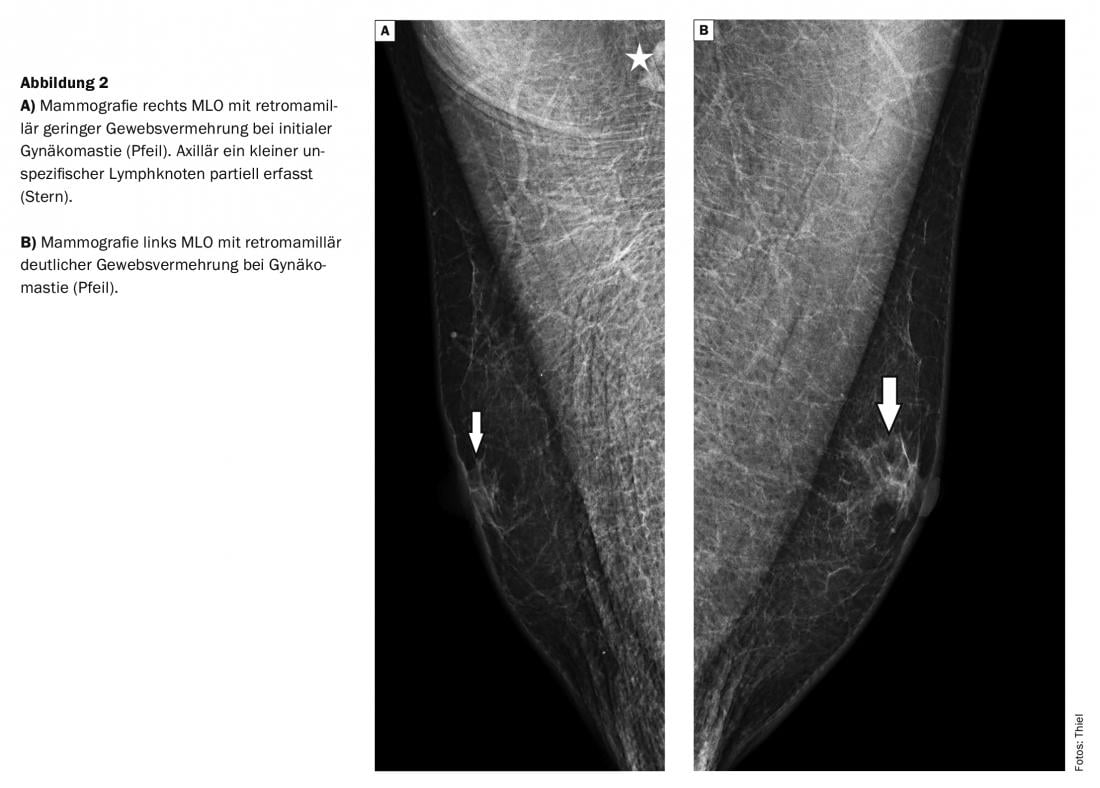
In case 2 (Fig. 2), a 49-year-old man without an obese habitus complained of a painful nodular retromammary change on the left side for several weeks. He received antihypertensive drug therapy. Mammography (Fig. 2A and 2B) each MLO images) demonstrated bilateral left dominant gynecomastia. A small nonspecific fatty degenerated axillary lymph node was included on the right axillary side.
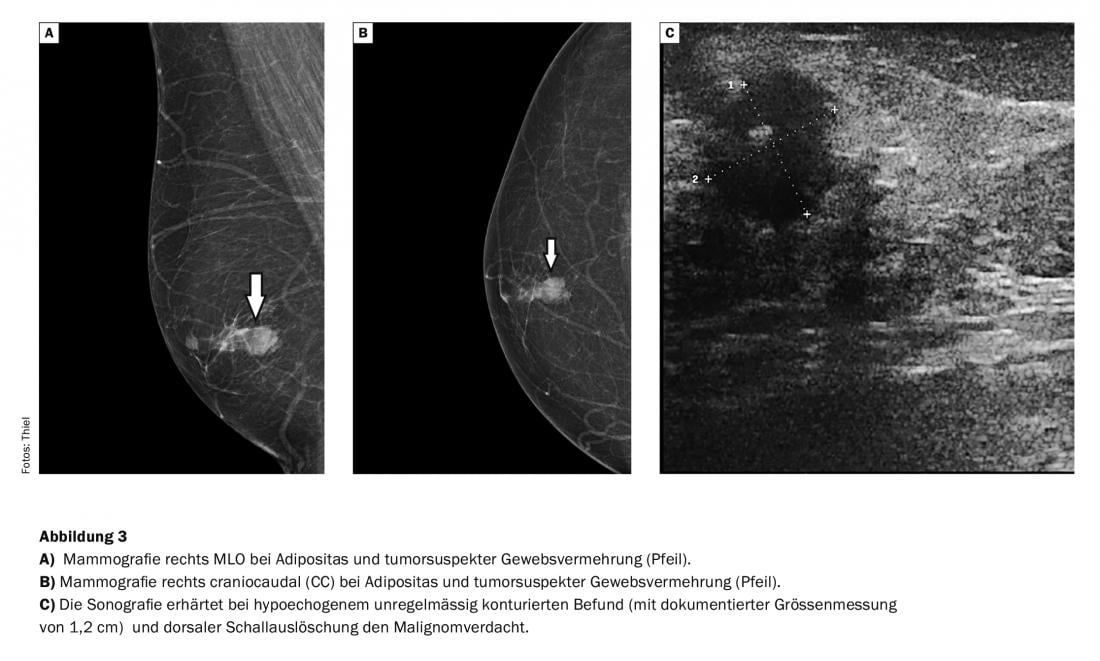
In case 3 (Fig. 3), a routine examination of a 66-year-old severely obese man revealed an indolent mobile retromammillary nodule that appeared tumor-suspect mammographically (Figs. 3A and 3B) . Supplementary sonography (Fig. 3C) confirmed the malignant findings. Histology confirmed the image morphologic diagnosis.
Take-Home Messages
- When diagnosing tissue proliferation of the male breast, the exact recording of family and personal history, clarification of drug therapy and clinical symptoms are very important and should also be reported to the radiologist.
- Malignancies of the male breast are very rare, and the risk of degeneration of gynecomastia is low.
- Imaging assessment of male breast tissue proliferation is primarily performed by mammography, with sonography providing complementary information.
- BI-RADS classification is the same for breast tumors of both sexes.
Literature:
- Leon-Ferre RA, et al: A contemporary review of male breast cancer: current evidence and unanswered questions. Cancer Metastasis Rev 2018; 37(4): 599-614.
- Fischer U (ed.): X-ray mammography. Georg Thieme Verlag Stuttgart, New York, 2003: 226-227.
- Heywang-Köbrunner SH, Schreer I: Imaging breast diagnostics. Georg Thieme Verlag Stuttgart, New York, 2996: 143-145.
- Lapid O, Jolink F, Meijer SL: Pathological findings in gynecomastia: analysis of 5113 breasts. Ann Plast Surg 2015; 74(2): 163-166.
HAUSARZT PRAXIS 2020; 15(7): 46-48