The cause of true bony fissure formation in the spine in the region of the interarticular portion, spondylolysis and consecutive spondylolisthesis vera, is a congenital bony defect of the articular processes of the vertebrae. Among the white population, about 7% of people are affected.
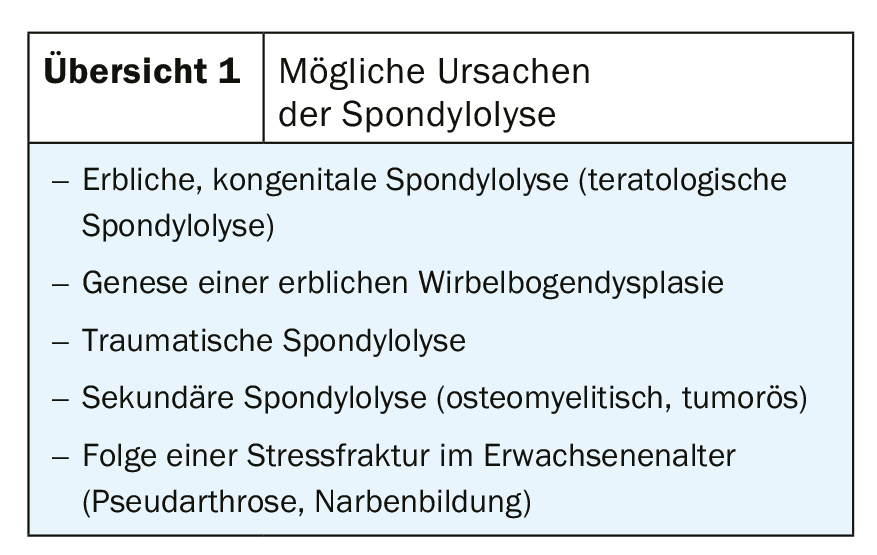
Lysis dominates in segments L4/5 and especially L5/S1 [1,2,16]. Among Alaska Natives, about 34% of the population is affected. In rare cases, the anomaly is conspicuous even in young children [10,15]. The anomaly was first described by Herbinaux as early as 1782 [9]. The incidence is reported to be as low as 4-5% at 6 years of age. Up to 50% of affected individuals show no increase in lysis or listhesis throughout life, and approximately 80% are asymptomatic. Unilateral spondylolysis may be associated with mild malrotation of the vertebra. Overview 1 lists possible causes of spondylolysis [2].
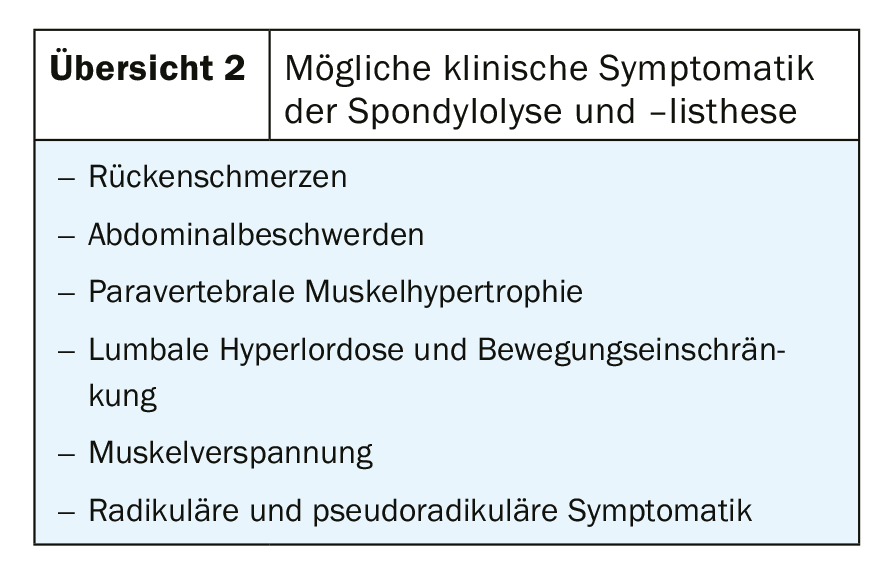
If spondylolysis and resulting listhesis becomes symptomatic [13], it is usually in adulthood. Due to mechanical loading, age, gender, body mass index, and disc and vertebral joint degeneration, the clinical presentation can range from minor nonspecific complaints to significant neurologic problems (Overview 2).
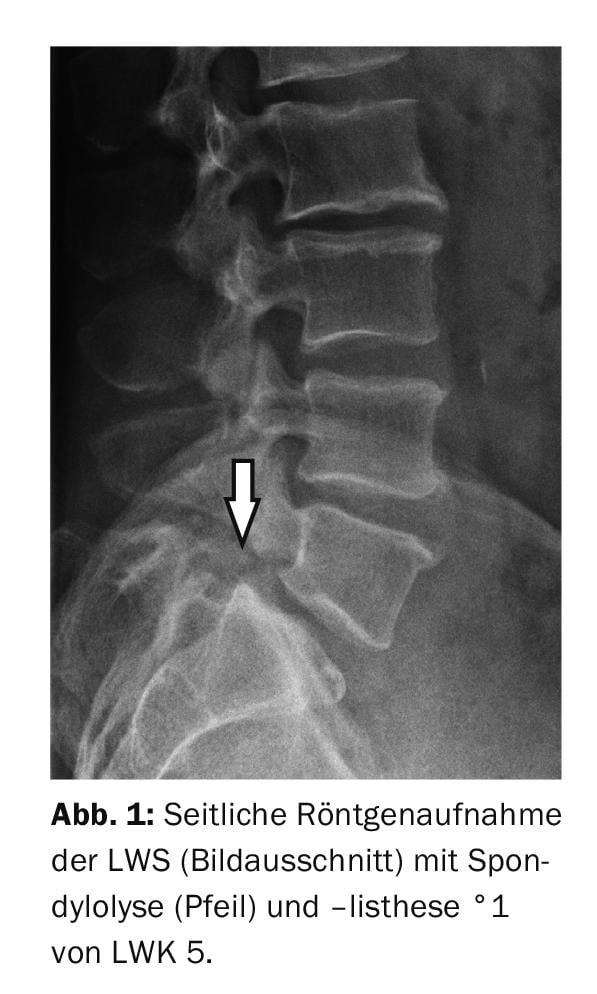
Spondylolysis and spondylolisthesis can already be demonstrated with the x-rays in 2 planes. Further imaging diagnostics are performed with CT and MRI. Concomitant degenerative changes are also assessed and all information needed for staging listhesis is obtained [7,12]. The staging established by Meyerding as early as 1932, based on the extent of vertebral displacement in relation to the underlying vertebral termination plate, has stood the test of time [2,3,8,13].
Therapeutic consequences result from corresponding neurological symptoms. If the symptoms cannot be controlled conservatively or if progressive structural disturbances can be documented, the indication for surgical treatment is given. Minimally invasive fusion should be favored [11]. Radiographically, listhesis is primarily seen in lateral projection, direct evidence of bony cleavage in the oblique radiographs that have been practiced for decades (“Scotch-Terrier”).
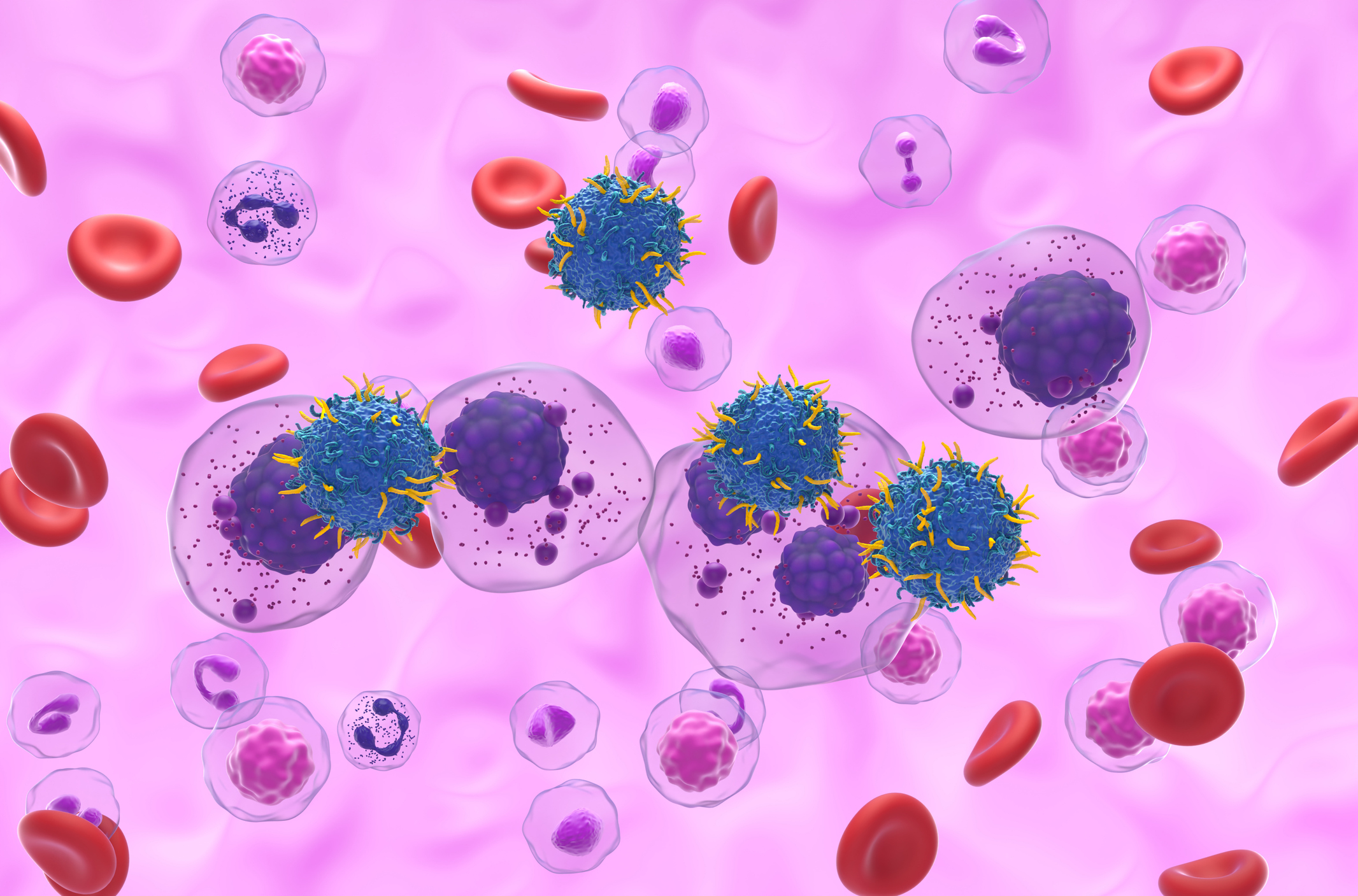
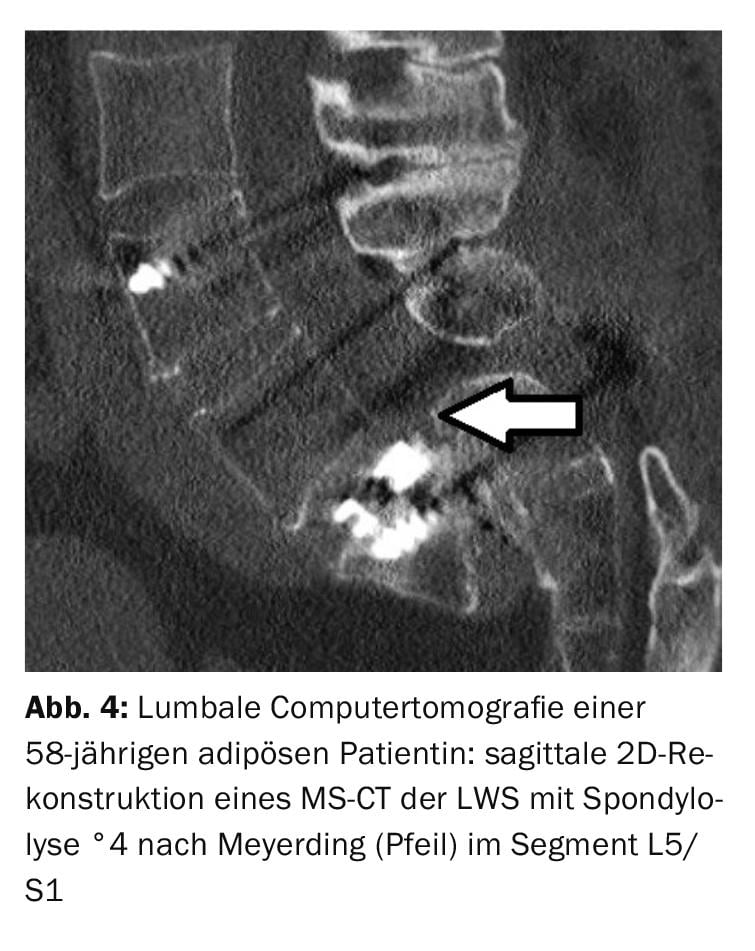
Computed tomographic examinations demonstrate spondylolysis, particularly in the bone scan. Sagittal reconstructions reproducibly demonstrate lysis and determine the degree of listhesis [4]. To be differentiated is hypertrophic facet joint arthrosis in case of increased bone reactions in the bone gap.
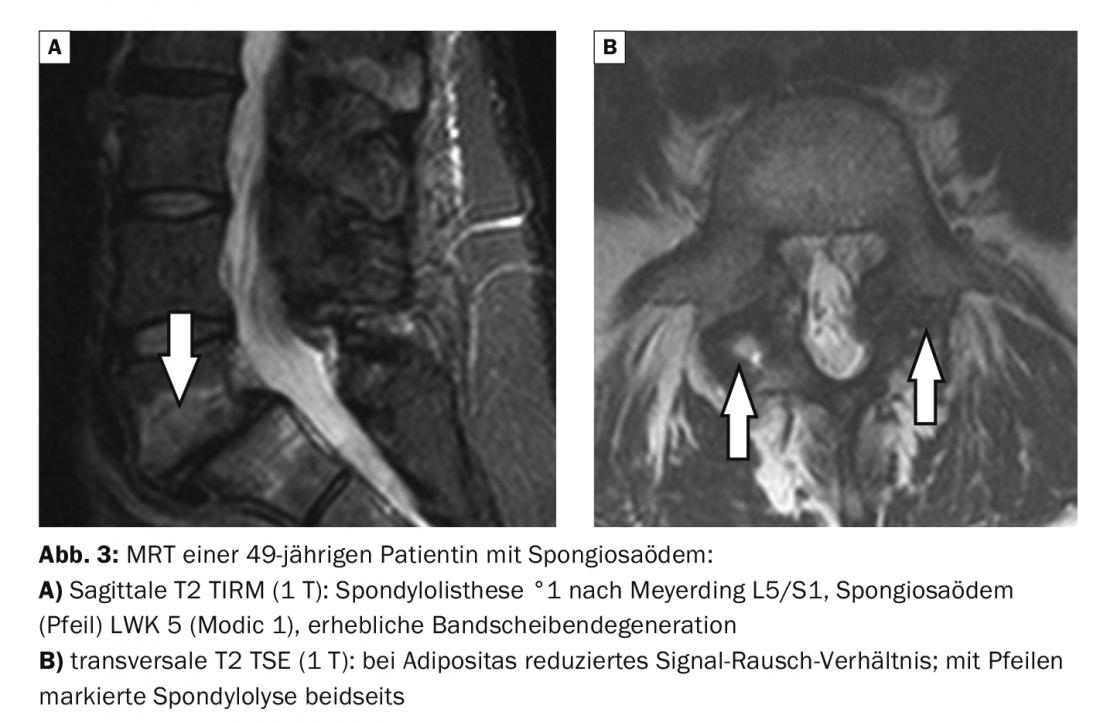
Magnetic resonance imaging also demonstrates lysis and listhesis very well, preferably in T1w or PDW sequences [11]. Appropriate mechanical loading and overloading in the segment with instability results in subdiscal spongiosa edema of the vertebrae (Modic 1) with detectable signal changes in the T1w, T2w, and fat suppression sequences [1]. Contrast administration is not obligatory, but would lead to signal increase in the edema zones. The simultaneous frequent irritant effusion in the small vertebral joints is hyperintense recognizable in T2w [12]. This can also occur with pseudospondylolisthesis, which is primarily found in the L4/5 segment.
Case studies
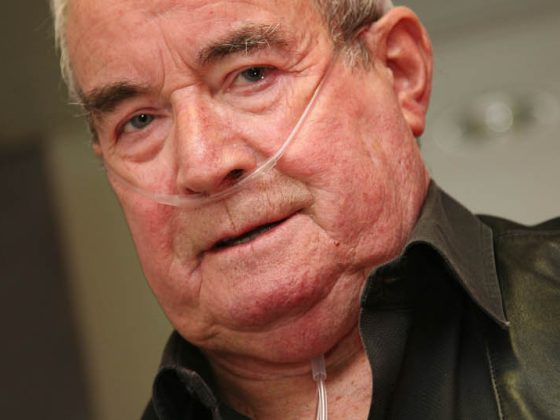
In the cases presented here, lumbar instability was manifested by gait-dependent leg pain (claudication) accompanied by radiculopathy with motion-dependent lumbalgia. Neurological deficits with sensory disturbances and paralysis or loss of bladder and rectal continence did not exist. In the case of the concomitant vertebral edema reaction (Modic 1), the lumbalgia intensified with increasing stress during the day.
The case example 1 shows a spondylolysis and -listhesis °1 according to Meyerding in a 52-year-old who was referred for examination because of deep-seated back pain (Fig. 1).
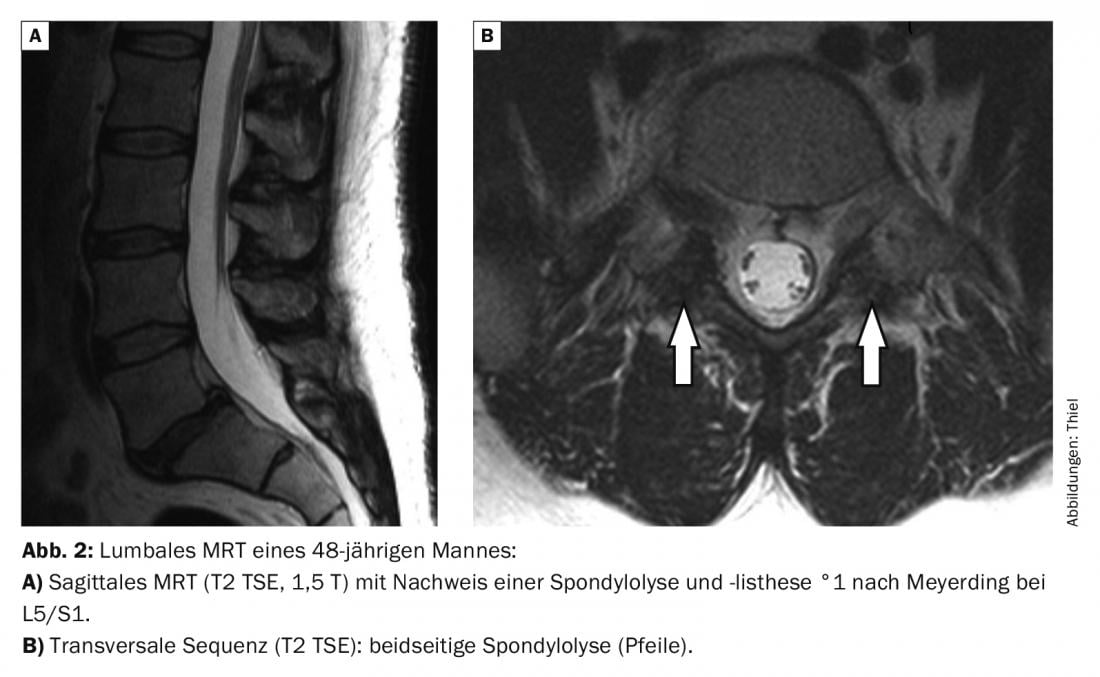
Documentation of spondylolysis and spondylolisthesis in case report 2 (Fig. 2) on lumbar MRI of a 48-year-old male demonstrates °1 without subdiscal spongiosa edema; MRI in case report 3 with a significantly degenerated disc demonstrates °1 to 2 in a 49-year-old female patient with spongiosa edema (Modic 1) (Fig. 3).
In case example 4 , spondylolisthesis vera °4 (Fig. 4) with complete ventral displacement from LWK5 to SWK1 is seen in the sagittal reconstruction of a lumbar computed tomography scan. Partial spondylodesis captures L4-S1. In discrepancy to the image morphology, the clinical symptoms in the 58-year-old obese patient were mild with moderate lumbaralgias.
Take-Home Messages
- Spondylolysis is a congenital change with bony cleavage of the interarticular portion of the vertebrae.
- In many cases, the anomaly is asymptomatic. With increasing age, load-dependent symptomatology may develop in combination with other degenerative changes.
- CT and MRI, as cross-sectional imaging techniques, can verify the totality of segmental changes, and radiographs in 2 planes can already demonstrate spondylolisthesis.
- In most symptomatic patients, conservative treatment is sufficient; surgical stabilization is reserved for severe courses.
Literature:
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Differential diagnosis in MRI. Stuttgart, New York: Georg Thieme Verlag 2002; 316.
- Dihlmann W: Joints – vertebral connections. 3rd, revised and expanded edition. Stuttgart, New York: Georg Thieme Verlag 1987: 494-501.
- Fatyga M, Majcher P, Krupski W, Gawda P: Value of the CT and MRI evaluations in diagnosis of patients with spondylolisthesis. Ortop Traumatol Rehabil 2002; 4(5): 575-581.
- Galanski M, Prokop M: Whole-body computed tomography. Stuttgart, New York: Georg Thieme Verlag 1998: 482.
- Kalpakcioglu B, Altinbilek T, Senel K: Determination of spondylolisthesis in low back pain by clinical evaluation. J Back Musculoskelet Rehabil 2009; 22(1): 27-32.
- Kim MW, Lee KY, Lee S: Factors Associated with the Symptoms of Young Adults with L5 Spondylolysis. Asian Spine J 2018; 12(3): 476-483.
- Krupski W, Majcher P: Radiological diagnosis of lumbar spondylolysis. Ortop Traumatol Rehabil 2004; 6(6): 809-818.
- Lasserre A: Memorix radiodiagnostics. Weinheim: Chapman&Hall GmbH 1997: 287-288.
- Logroscino G, et al: Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst 2001; 17(11): 644-655.
- O’Donnell M, Lavelle WF, Sun MH. Spondylolisthesis with spondylolysis in a 17-month-old: a case report. J Spine Surg 2017; 3(4): 689-692.
- Park Y, Seok SO, Lee SB, Ha JW: Minimally Invasive Lumbar Spinal Fusion Is More Effective Than Open Fusion: A Meta-Analysis. Yonsei Med J 2018; 59(4): 524-538.
- Schinnerer KA, Katz LD, Grauer JN: MR findings of exaggerated fluid in facet joints predicts instability. J Spinal Disord Tech 2008; 21(7): 468-472.
- Standaert CJ, Herring SA, Halpern B, King O: Spondylolysis. Phys Med Rehabil Clin N Am 2000; 11(4): 785-803.
- Thiel HJ: Cross-sectional diagnosis of the spine (1.8). Degenerative changes: Spondylolisthesis. MTA Dialog 2010; 11(5): 386-388.
- Thiel HJ: Spondylolysis. MTA Dialog 2019; 20 (8): 18-21.
- Uhlenbrock D (ed.): MRI of the spine and spinal canal. Stuttgart, New York: Georg Thieme Verlag 2001: 213-214.
- Ulmer JL, et al: MR imaging of lumbar spondylosis: the importance of ancillary observations. AJR 1997; 169(1): 233-239.
HAUSARZT PRAXIS 2020; 15(5): 43-44