Guidelines specific to this context exist to improve the management of depressive symptoms in primary care. It is not uncommon for general practitioners to be the first or only point of contact for depressed patients. The etiology can be very variable. Diffuse somatic complaints sometimes conceal larvalized depression.
iFightDepression® [1] is a project funded by the EU Commission in which fact sheets on individual aspects of the disease have been developed. Neither the EU [2] nor the WHO [3] provide their own guidelines, but address the issue as part of the health agenda. The US [4] and German guidelines [5] are based on the respective cultural conditions and health care systems, which differ from Swiss conditions.
Guidelines from Mednetbern
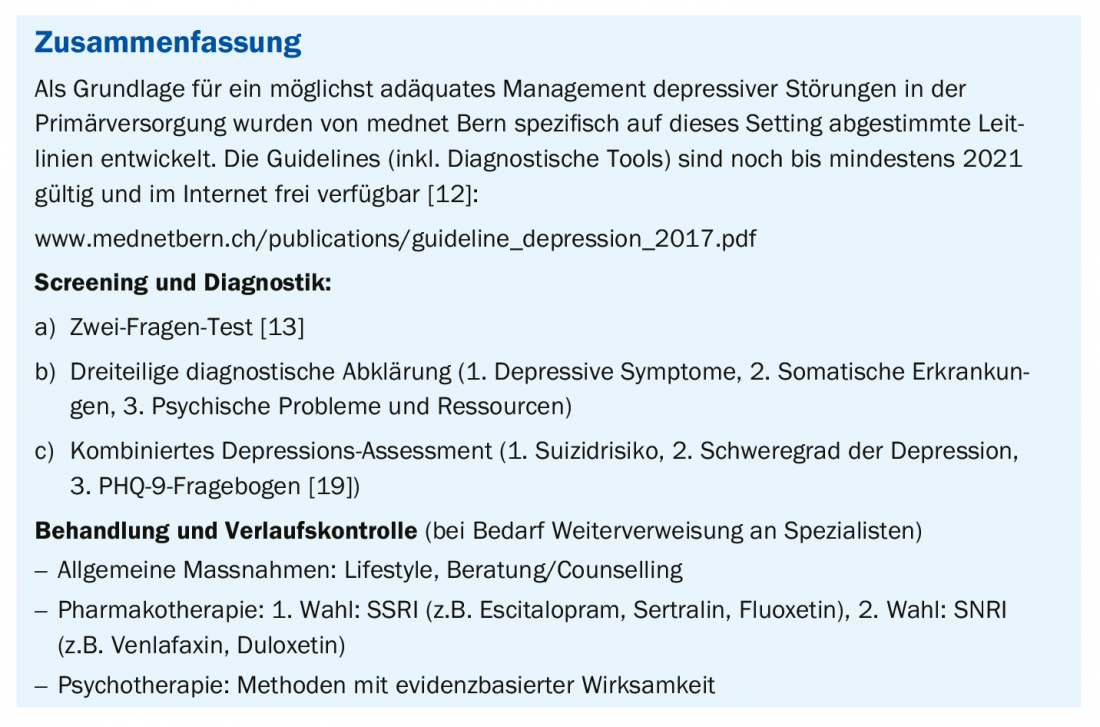
As a supplement to the guidelines on somatic therapy of depression [6,7] and psychotherapy of depression [8], which have been available in Switzerland for some time and were developed under the aegis of the psychiatric societies, the mednetbern network of physicians [9] has developed guidelines specifically tailored to the conditions and needs of the outpatient primary care setting here. The target user group is physicians, and the recommendations apply to adults regardless of age group and gender. This article contains a compact summary of the guidelines valid in the current version until at least 2021.
The authors of the guidelines define depression as follows [9]: “Neurobiological syndrome with severe psychological, mental, physical, and social effects. Leading symptoms: Depressed mood, joylessness, impaired self-esteem, physical well-being, and sleep (lifetime prevalence 15%). Unrecognized and untreated, the disorder can lead to death by suicide and negatively affect the course of many illnesses and the ability to work.”
The theoretical rationale of the assessment manual is based, among other things, on the internationally recommended procedure for the management of depressive disorders (ICD-10: F32.- Depressive Episode) [10]. The goal is to help better identify, assess, and treat depression [9]. This includes, but is not limited to, information on medications, ability to work, and fitness to drive. Clear decision criteria have been defined for referral. Validated psychometric questionnaires are included as an aid to rational assessment. The “Guideline Depression” from mednetbern is freely available on the web [11,12]: www.guidelines.fmh.ch; www.mednetbern.ch
Diagnostic algorithm
According to the currently valid classification, the following criteria must be fulfilled for the diagnosis of “depression”: for at least 4 weeks ≥2 main symptoms and a total of ≥4 main and additional symptoms that cannot be attributed to the abuse of psychotropic substances. A depressive episode caused by somatic illness or medication is considered an organic mental disorder (F06.32) [10].
In terms of differential diagnosis, particular attention should be paid to distinguishing it from grief reaction, adjustment disorder, substance dependence disorders, and other mental illnesses. Physical symptoms (for example, weight loss) should always be clarified.
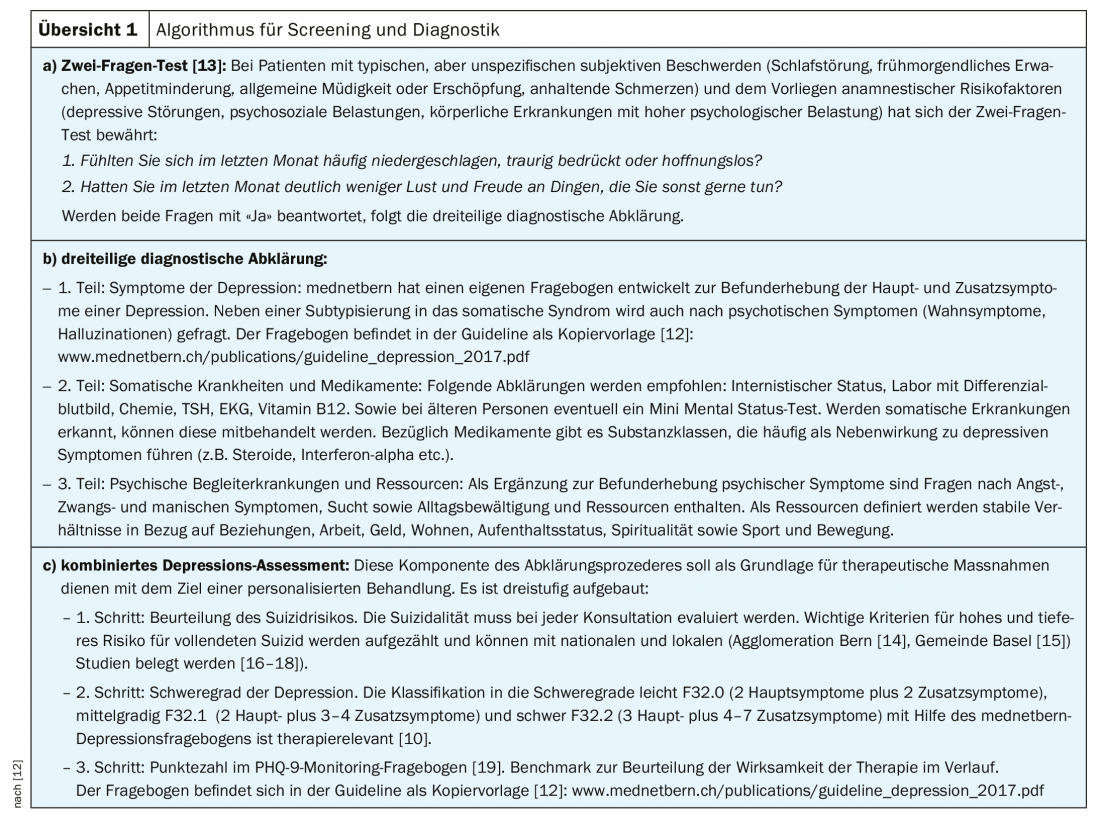
There is a wide range of diagnostic tools which can be used as aids. The mednet Bern guidelines recommend the following procedures: a) Two-question test [13]: b) three-part diagnostic workup, (c) combined depression assessment (review 1).
Treatment recommendations
Based on the results of the assessment, therapy can be implemented with the goal of achieving recovery or remission, reducing mortality, especially from suicide, and preventing relapse and recurrence [9]. Every patient can receive general measures/counseling (counselling) through the primary care physician. Further therapeutic measures are psychotherapy and pharmacotherapy. For mild and moderate depressive episodes, patient preference should determine which measure should be used first. In mild depressive episodes, antidepressants should be used for initial treatment only after particularly critical consideration of the risk-benefit ratio. In severe depressive episodes, the combination of psychotherapy and pharmacotherapy is mandatory.
General Measures (Counselling): Participatory decision making promotes understanding and commitment/adherence.
Lifestyle: sleep hygiene, regular diet and physical exercise (at least 2-3× per week 30-45 min endurance training) should be recommended. Harmful effects of alcohol and drugs must be emphasized.
Counseling/Counselling: education, psychoeducational-supportive discussions, qualified guided self-help, problem-solving approaches.
Pharmacotherapy: the indication for a particular drug should be made by the individual side effect and risk profile.
- 1st choice: SSRIs (Selective Serotonin Reuptake Inhibitors): Escitalopram, sertraline, fluoxetine.
- 2nd choice: SNRI (Selective Norepinephrine Reuptake Inhibitors): Venlafaxine, duloxetine. Important: in major depressive episode (F32.2) [10], venlafaxine is drug of 1st choice
- 3. special cases: according to guidelines (page 3) [12], e.g. depending on the situation mirtazapine for sleep disorders, duloxetine or amitriptyline for chronic pain.
- 4. strategies for lack of efficacy: change of antidepressant, dose increase, combinations of antidepressant with psychotherapy, augmentation (combination of an antidepressant with mirtazapine, atypical neuroleptics, thyroid hormone, lithium).
Psychotherapy: Patients for whom psychotherapy is indicated can be referred to specialists: Cognitive behavioral therapy, conversational psychotherapy, or psychodynamic/analytic psychotherapy are evidence-based effective methods for treating depression [20,21].
Treatment algorithm: therapeutic measures should be tailored to the severity of the depressive episode and should be continued over clearly defined periods of time even after improvement or remission. As a first step, the implementation of general measures/counseling (counselling) is recommended for all patients. If the depression is mild, it is possible to wait for a period of 14 days before initiating pharmacotherapeutic or psychotherapeutic measures (“watchful waiting”). For mild or moderate depression, the use of an antidepressant or psychotherapy is advised. Medication and psychotherapy in combination are recommended for major depressive episodes.
Follow-up: Response to treatment should be evaluated at 14-day intervals. If the reduction in depressive symptoms in the PHQ-9 monitoring questionnaire [19] is less than 50%, compliance should be questioned, therapy modified, or the patient referred.
Referral: Emergency, to psychiatric emergency service or psychiatric clinic: In case of danger to self or others, severe depression, depression with psychotic symptoms. Regular, to office-based psychiatrist: for moderate to severe depression, concomitant psychiatric disorders (e.g., substance abuse), treatment resistance.
Literature:
- European Alliance against Depression: iFightDepression®, http://ifightdepression.com/de/
- European Commission: Measures against depression, http://ec.europa.eu/health/ph_determinants/life_style/mental/docs/depression_de.pdf
- WHO Media Centre: Depression. www.who.int/mediacentre/factsheets/fs369/en/
- Gelenberg AJ, et al: Practice guideline for the treatment of patients with major depressive disorder, third edition. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf
- DGPPN: S3 Guideline and National Health Care Guideline (NVL) Unipolar Depression. www.dgppn.de/leitlinien-publikationen/leitlinien.html
- Holsboer-Trachsler E, et al: The somatic treatment of unipolar depressive disorders 1st part. Swiss Med Forum 2010; 10(46): 802-809.
- Holsboer-Trachsler E, et al: The somatic treatment of unipolar depressive disorders 2nd part. Switzerland Med Forum. 2010;10(47):818-22.
- Küchenhoff J: Psychotherapy of depression. Treatment recommendations for psychotherapy of depression. www.psychiatrie.ch/sgpp/
- Giania A, et al: Guidelines for primary care providers: Depression. Guideline from mednetbern. Prim Hosp Care (en) 2018; 18(05): 78-81.
- ICD-10, www.icd-code.de
HAUSARZT PRAXIS 2020; 15(2): 19-20











