Swelling of the neck is a common complaint in the primary care physician’s office. Ultrasound examination is a useful tool for targeted diagnostics. It is particularly helpful in the evaluation of unclear swellings of the neck, as almost all structures are easily accessible.
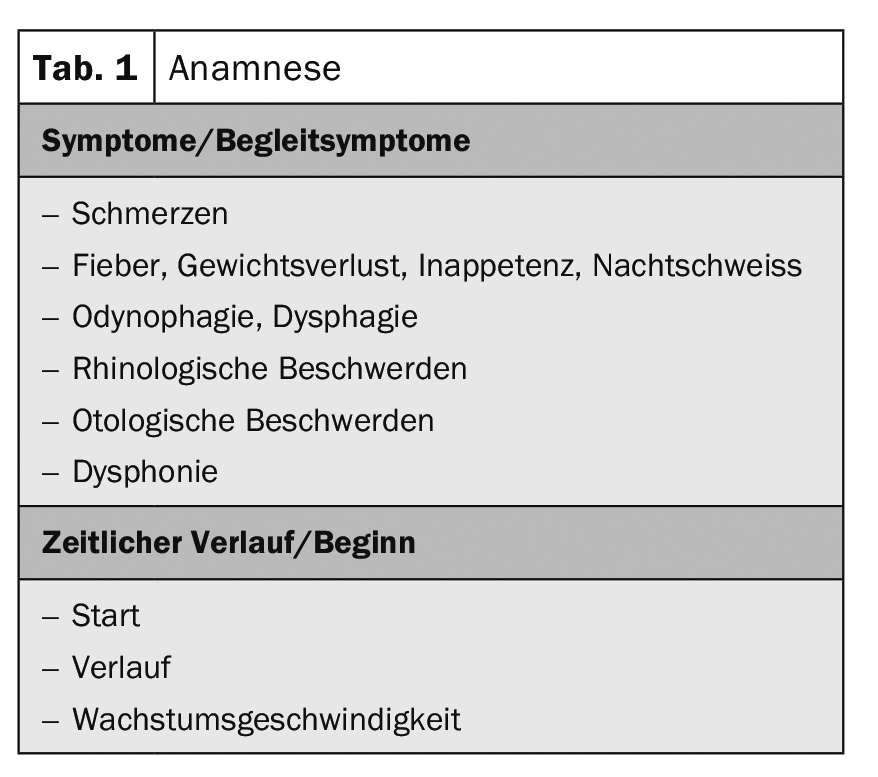
Swelling of the neck is a common complaint in the primary care physician’s office. A working hypothesis can already be established by taking a targeted history. The aim of the anamnesis is to ask about the symptoms and accompanying symptoms in addition to the onset and time course (Tab. 1). The personal history also includes risk factors for swelling of the neck (medications, occupational exposure, contact with animals, stays abroad, noxious substances or secondary diseases). When taking a family history, the most important thing is whether there is a family history of tumors.
The status evaluates localization, displaceability, number of masses, consistency, fistula formation, hyperthermia, and redness of the skin over the swelling. The point is to find a cause, or at least narrow down the possibilities. Especially in the case of infectious or tumorous causes, the status of the entire mucous membranes in the ear, nose and throat area is very important.
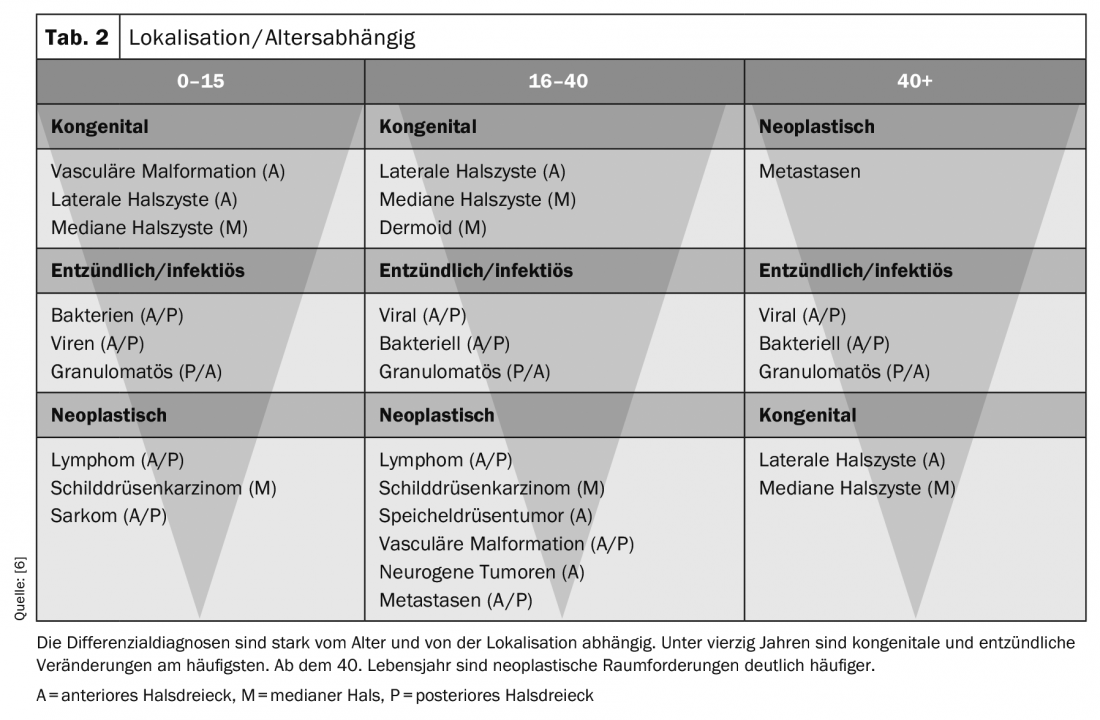
Age and localization have a major influence on narrowing down the differential diagnoses (Tab. 2). A working hypothesis can then be established on the basis of the patient’s history and status, which is to be tested by ultrasound. Since all structures in the neck are very superficial, they can be visualized very well by ultrasound. A linear probe with a frequency range of 8-13 MHz is recommended (a matrix probe if available).
To get a good quality image, we recommend applying the 4-button rule [1]. The aim is to optimize the quality of the image as standardized as possible in a short time. Four settings are made in each case:
- Gain
- Frequency (10-12 MHz)
- Depth (approx. 2.5-3 cm)
- Focus (approx. 1.5-2 cm)
Normally, the ultrasound examination is performed with the patient lying down. The device is operated with the left hand and the probe is guided with the right hand. It is important to have a good attitude. The chair, couch and monitor should be adjusted to the body size by the examiner. It is usually recommended to rest the right arm on the patient. If propping is uncomfortable, the patient can cross his/her arms and the examiner can rest the arm on them.
Depending on the exposure of the neck, a pillow can be placed under the neck. It is worthwhile to always perform the ultrasound examination equally and, above all, systematically, so that all regions of the neck are examined. There is no standard for the sequence. We at the ENT Clinic Bern always start with the examination of the thyroid gland. With the image of the thyroid gland, we also perform the device settings (4-button rule). Afterwards, we first scan the entire neck on the non-pathological side incl. of the parotid gland and then on the pathological side incl. of the parotid gland. The goal is that all regions (lymph node levels) on the neck are controlled.
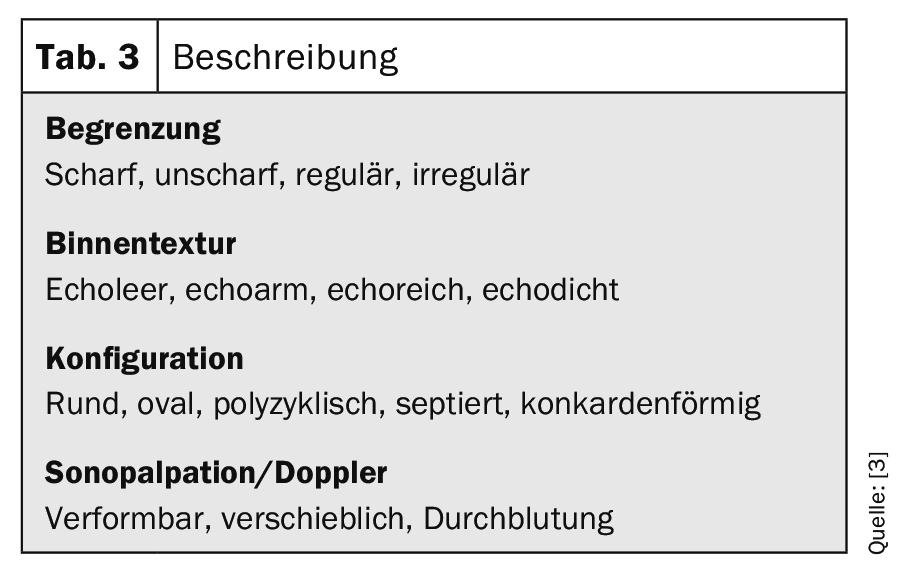
Pathology must always be viewed and assessed in two planes. The boundary, internal structure, configuration, sonopalpation and blood flow are assessed (Table 3). Since the structures and pathologies in the neck region are very superficial, sonopalpation can provide good information on whether the mass is soft (cystic) or hard (solid). Elastography can also be used with the newer devices to assess the hardness from the tissue. If dorsal sound amplification is seen, it is a sign of fluid in the mass. This may be pus, blood, seroma, or even necrosis. Sonographically, no clear differentiation of these fluids can be made. The medical history can be helpful for differentiation.
If the diagnosis is not clear, or to confirm a diagnosis, a fine needle aspiration may be done. This should always be ultrasound-guided, especially for smaller lesions.
There are two ways to perform the puncture:
- In-plane technique: The puncture is made longitudinally to the transducer in the transducer plane. With this method, the complete needle can be displayed incl. the polish.
- Out-of-plane technique: The puncture is perpendicular to the transducer plane. This allows only the tip of the needle to be seen. This method is particularly suitable for deeper-lying space lesions.
Recommendation for performing fine needle aspiration [2].
According to the latest European guidelines, it is recommended to protect the transducer, disinfect the skin and prick it with sterile gel or disinfectant that does not attack the transducer. By means of puncture, fluid can be aspirated or cells can be obtained. The fluid and/or cells can then be examined cytopathologically +/- bacteriologically.
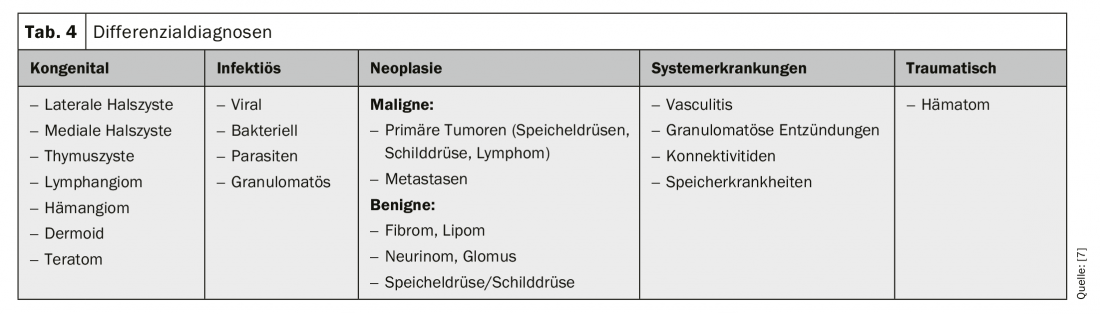
Pathologies according to etiology (Tab. 4): By means of history and status, it is usually possible to divide the possible pathologies into large groups of differential diagnoses. This helps in the evaluation of the ultrasound images.
Pathologies according to localization (Fig. 1) : Especially in tumor diagnostics, it is important that the localization of a mass is as precise as possible. The neck is divided into six anatomically limited levels.
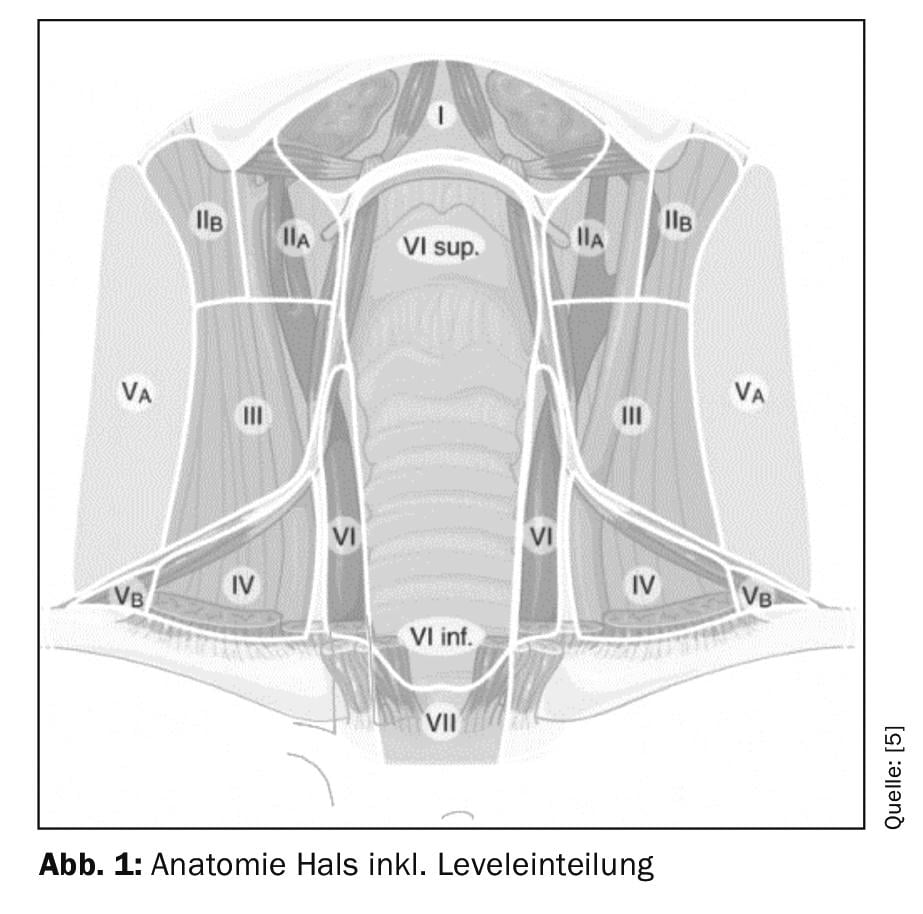
The submental region (level Ia) is formed by the venter anterior of the digastric muscle, the os hyoideum, and the median neck plane. The submandibular region is formed by the venter anterior of the digastric muscle, the venter posterior of the digastric muscle, and the inferior border of the mandible (Level Ib). The Eq. submandibularis is also located in this region.
The lateral portion of the neck is divided by the sternocleidomastoid muscle into an anterior portion (Level II-IV) and a posterior portion (Level V). The anterior portion is divided into level IV (caudal to the omohyoideus muscle), level III (cranial to the omohyoideus muscle and caudal to the carotid bifurcation), and level II (cranial to the carotid bifurcation and caudal to the digastric venter poserior muscle). The median neck (level VI) includes all pretracheal and paratracheal lymph nodes as well as the perithyroid lymph nodes. The lateral border is formed by the aa. Carotis communis formed.
Pathologies in the median neck
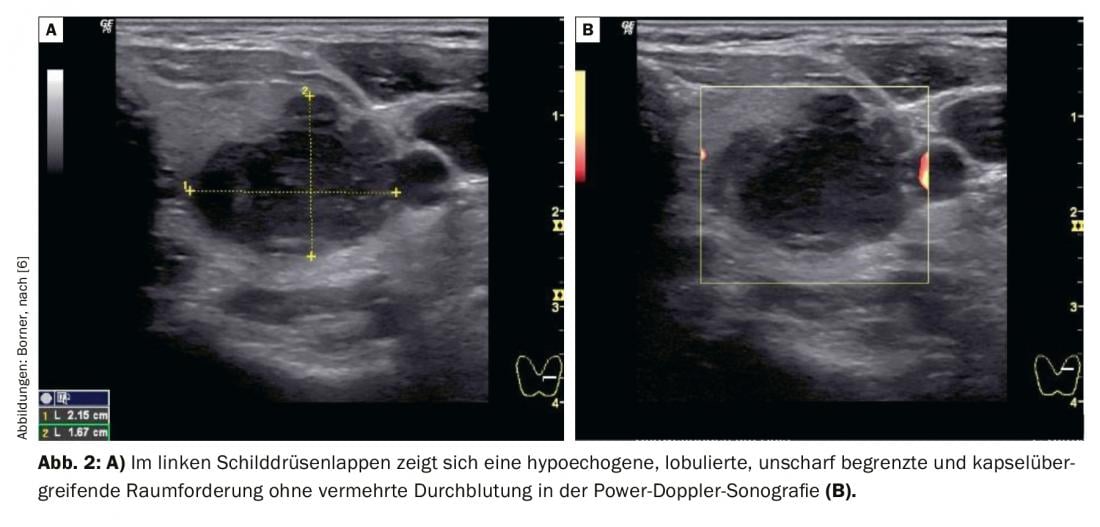
Pathologies in the median neck region are often congenital in origin (median neck cyst, thymic cyst, dermoid, teratoma), especially in young patients. After the age of 40, neoplasms are significantly more frequent (metastases or benign/malignant primary tumors). It is rare for a congenital mass to be symptomatic for the first time after the age of 40. Very often thyroid nodules are found sonographically as incidental findings. Thyroid nodules may be symptomatic above a certain size when they press or become visible on the trachea, esophagus, larynx, or externally. The prevalence of thyroid nodules is about the same as the patient’s age. Since thyroid nodules are very common incidental findings, it is important to know how to deal with them. It is important that each node is described and assessed. There are different guidelines on how thyroid nodules should be evaluated and how to proceed from there (ATA, TIRADS). At Inselspital, we follow the 2015 American Guidelines (ATA) (Table 5) [3]. The 2015 ATA guidelines fully integrated ultrasonography into the treatment decision. Each node is assessed individually and assigned a risk category. There are five risk categories. If the node is hypoechogenic, it already belongs to one of the two highest risk categories. If another malignancy sign is also present, such as indistinct boundary, microcalcification, taller than wide, or extrathyroidal spread, the nodule belongs to the highest risk category with a malignancy risk of >70-90%. Depending on the size of the lump and the risk class, a decision is made as to whether a puncture is necessary or whether the lump can be checked using ultrasound (Tab. 5).
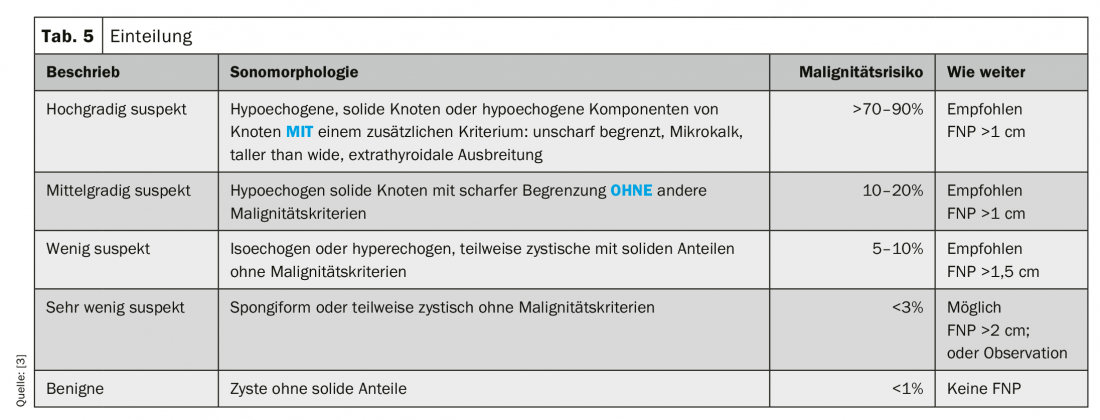
Figure 2 of the left thyroid gland shows a hypoechogenic, indistinctly circumscribed mass measuring 2.15×1.67 cm, which is lobulated and shows no increased blood flow. In the marginal area it goes out over the capsule of the thyroid gland. According to current ATA guidelines, this lesion is highly suspicious for thyroid malignancy because it is hypoechogenic and has additional malignancy criteria (indistinct boundary, extrathyroidal spread). In this case, according to the guidelines, a fine needle aspiration of 1 cm or more is recommended. Fine needle aspiration revealed undifferentiated thyroid carcinoma in this case.
Pathologies in the lateral neck region
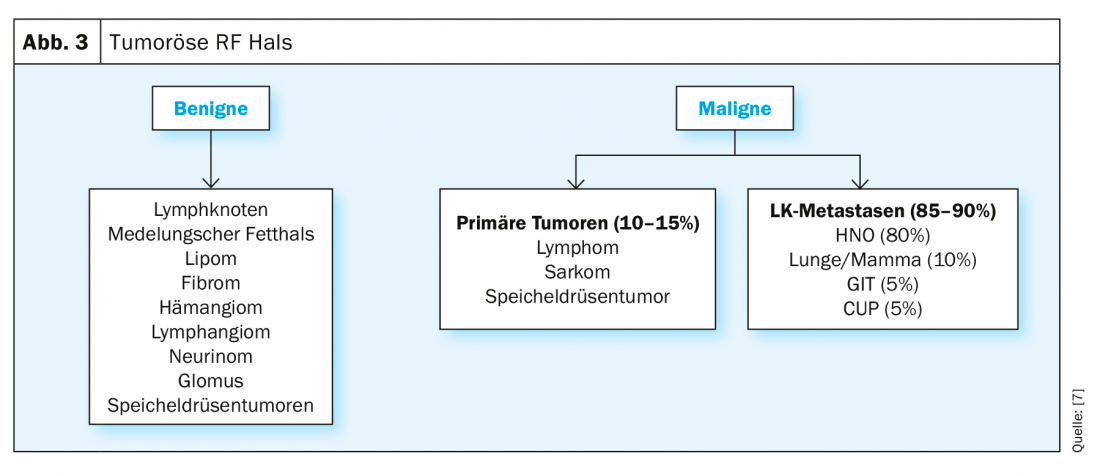
By means of anamnesis and status one inquires about the dynamics and a possible cause for the swelling. Inflammatory causes of swelling (reactive lymph nodes) are most commonly found. Benign tumors (lipomas, fibromas, neurinomas, glomus tumors, salivary gland tumors) and in patients over 40 years of age, metastases and primary malignant tumors are possible (Fig. 3). Among malignant space-occupying tumors, metastases are significantly more common than primary malignancies. Metastases in the neck area have the primary tumor in the ENT area in 80%. Therefore, it is very important to perform a complete mucosal status in any unclear neck mass.
Case presentation
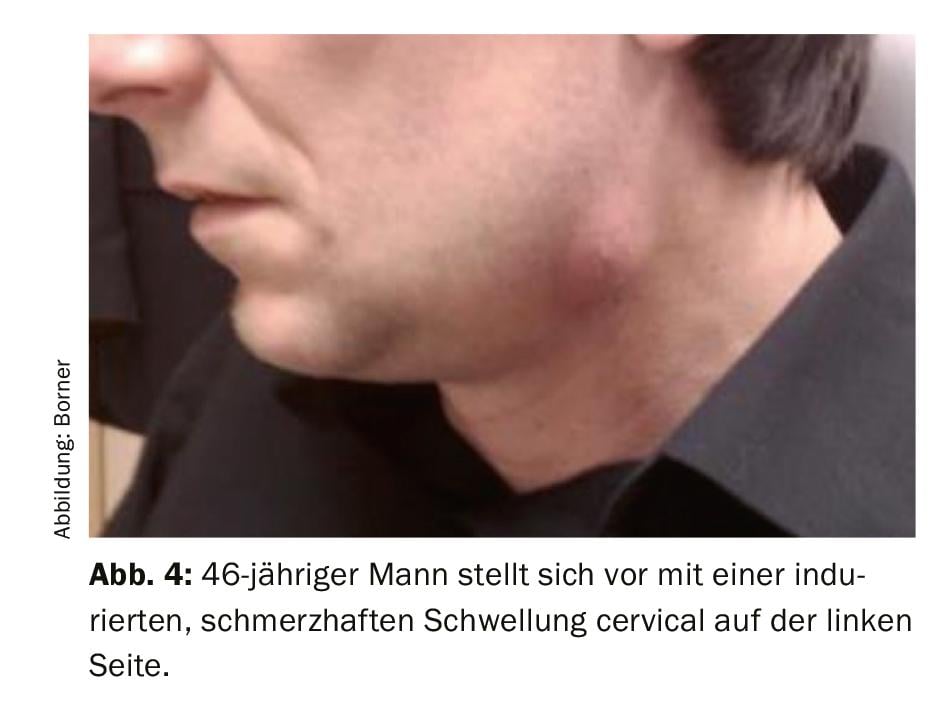
A 46-year-old man presents with an indurated, painful swelling cervical on the left side (Fig. 4) for 2 weeks. Previously, he never had similar complaints. Anamnestically, no clear cause could be elicited (no focus of infection, no B-symptoms, no stay abroad, no pets, no noxae, no other diseases). Except for the painful indurated swelling, the status shows only a carious tooth status. The other ENT status was unremarkable.
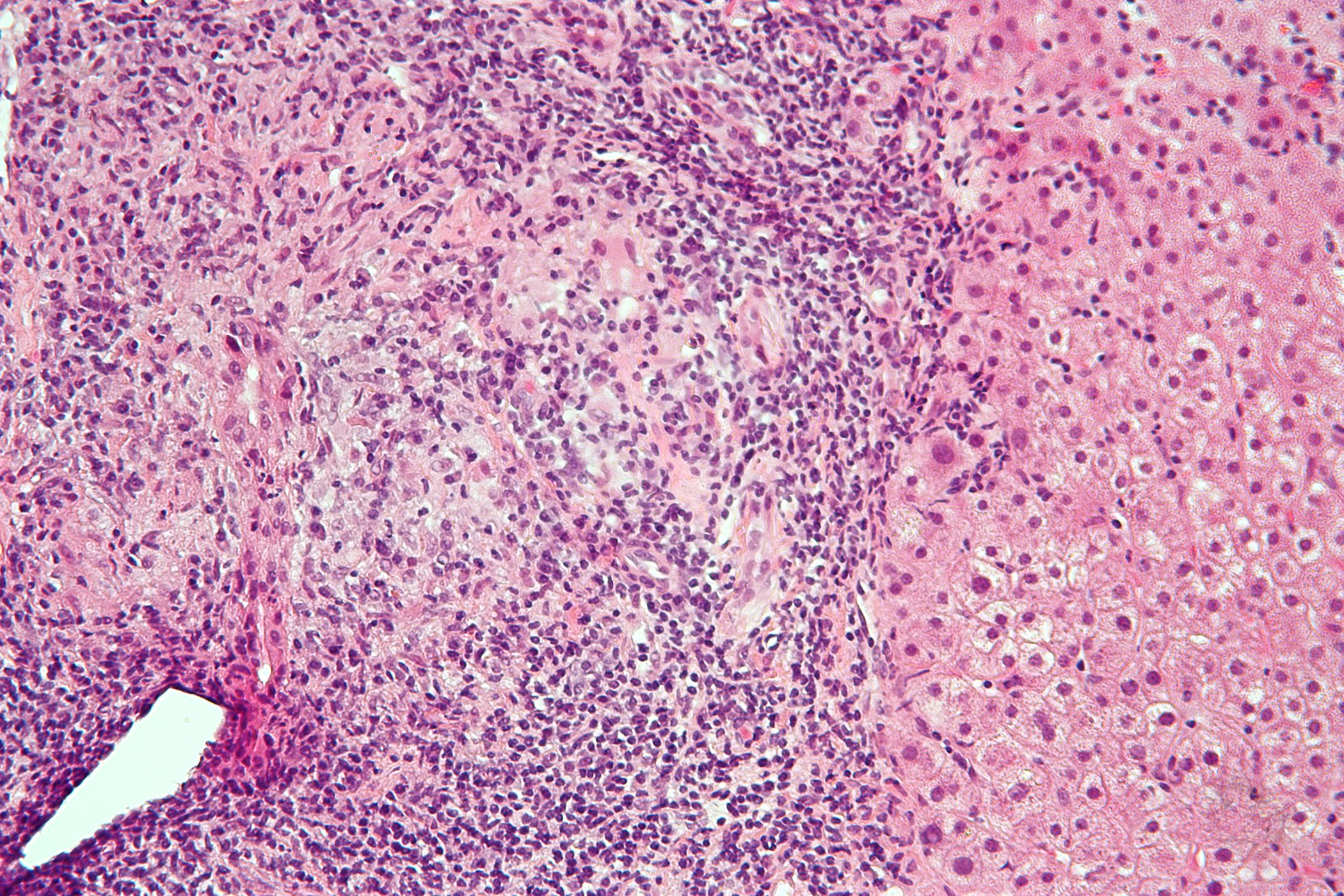
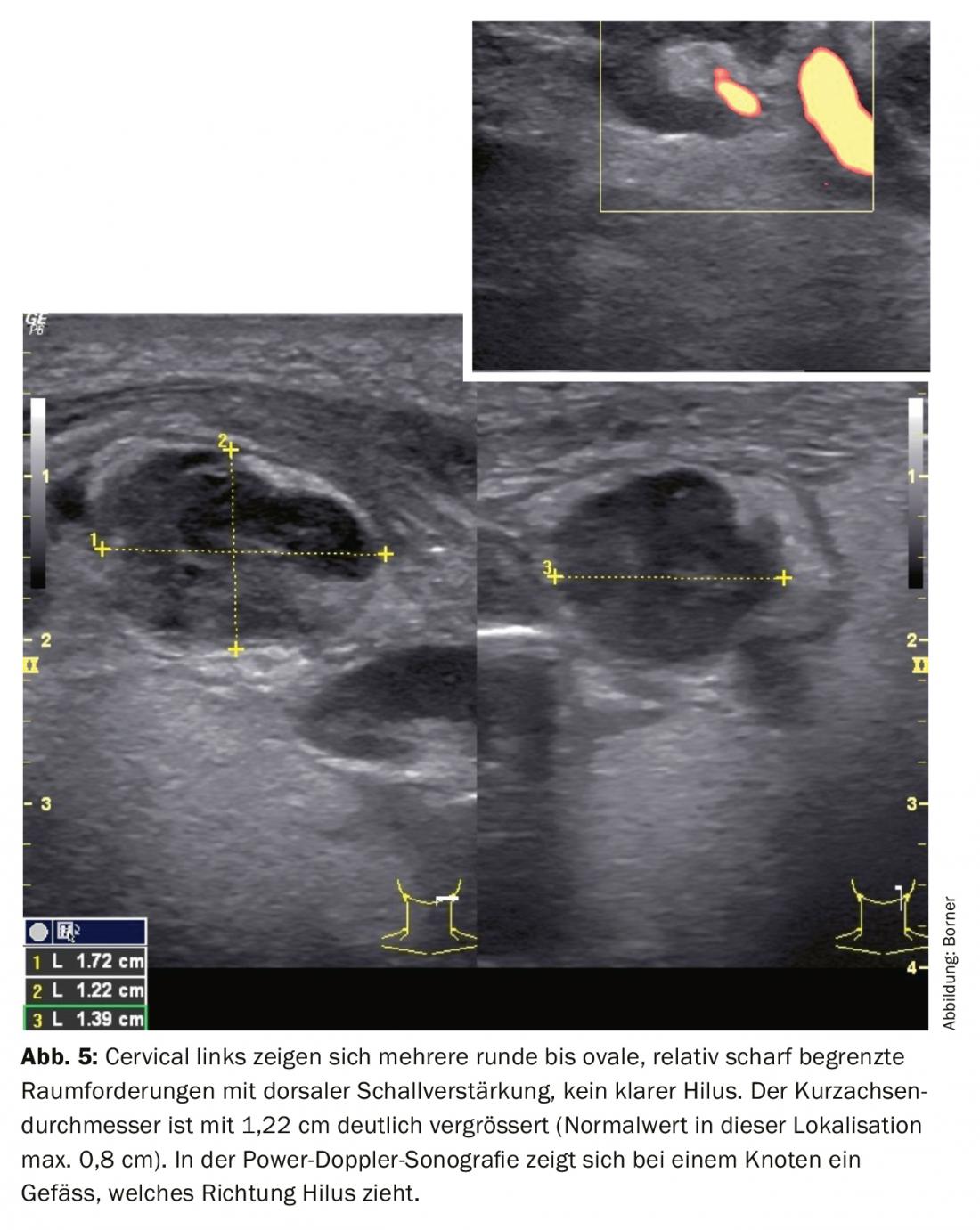
Ultrasound shows multiple relatively sharply demarcated, hypoechogenic, round to oval, inhomogeneous RF with dorsal sound enhancement. The short axis diameter of 1.22 cm is significantly increased (normal value in this localization maximum 0.8 cm). No increased central or peripheral blood flow (Fig. 5).
To narrow down the differential diagnoses, we systematically ask ourselves the following three questions in each case:
1. could it be a lymph node?
2. if it is a lymph node, is it pathologically altered?
3. if it is pathologically altered, what is the pathology?
a. Hyperplastic
b. Inflammatory
c. Neoplastic
Specifically, this would mean for the lesion on Figure 5:
1. it could be a lymph node.
2. it is pathologically altered.
3. based on the ananmnesis and dorsal sound enhancement, it could be an abscessed lymph node.
To confirm the diagnosis, an FNP was performed, which showed pus. The pus was examined and showed infection with Actinomyces. We started antibiotic therapy with co-amoxicillin i.v. After 3 days there was no improvement, so we had to perform an abscess drainage externally. The postoperative course was very gratifying.
Ultrasonographic evaluation of lymph nodes is difficult because there are several criteria that cannot be considered individually but only in context [4]. The assessment includes:
- Lymph node size; especially the short axis diameter.
- the homogeneity
- the limit
- the blood circulation
- the assessment of the hilus and the cortex
- the shape
It should be specifically mentioned that round lymph nodes can also be normal in the neck region (in level I, IIA and in the parotid gland). When assessing the size, the simplest method is to determine the short axis diameter.
- The short-axis diameter may be a maximum of 8 mm in Level IB and II
- In all other regions, it may be a maximum of 5 mm.
This rule greatly simplifies the assessment, since no index needs to be calculated. It also simplifies the follow-up of altered lymph nodes.
Pathologies of the salivary glands
Humans have six major salivary glands (gl. parotis, gl. submandibularis, gl. sublingualis), each of which is paired, and 600-800 minor salivary glands located in the mucous membranes. Sonomorphologically, the large salivary glands are homogeneous and hyperechogenic. The small salivary glands as well as the ductal system cannot be visualized in normal cases. Since the major salivary glands are paired, it is worthwhile to compare the salivary glands, especially if pathology is present. There are circumscribed lesions (tumors) and diffuse changes (e.g., inflammation, systemic disease).
In pathologies of the salivary glands, the question of food dependence is central. All pathologies (salivary stones, stenosis, tumors) that affect or constrict the ductal system lead to food-related complaints.
Acute diffuse changes are often viral (e.g., mumps) or bacterial infection. Sonomorphologically, these cannot be distinguished. Viral inflammation more often affects multiple glands and bacterial inflammation more often affects only one gland. By means of ultrasound, however, an abscess can be ruled out.
In diffuse chronic changes, primary and secondary Sjögren’s disease are the most common causes. These lead to a scarring remodeling of the complete tissue. Sonomorphologically, the tissue is hypoechogenically altered. Depending on the stage, it has cystic changes, which can have different sizes. It may also have scarring changes, which present hyperechogenically. Usually several glands are affected. If the ductal system is affected, the patient will have additional food-related symptoms. In this case, the duct system can usually also be represented sonomorphologically.
The circumscribed changes are almost always neoplasms. In the parotid gland, 80% of circumscribed masses are benign; in the gl. submandibularis 50%, and in minor salivary glands only 20% of the space-occupying lesions are benign.
Rule: As a basic principle, the smaller the gland, the greater the probability that a circumscribed mass is malignant.
As a special pathology, salivary stones may occur in the salivary glands. Salivary stones occur in 1% of the population. Salivary stones are most common in the gl. submandibularis. However, they are very rarely symptomatic.
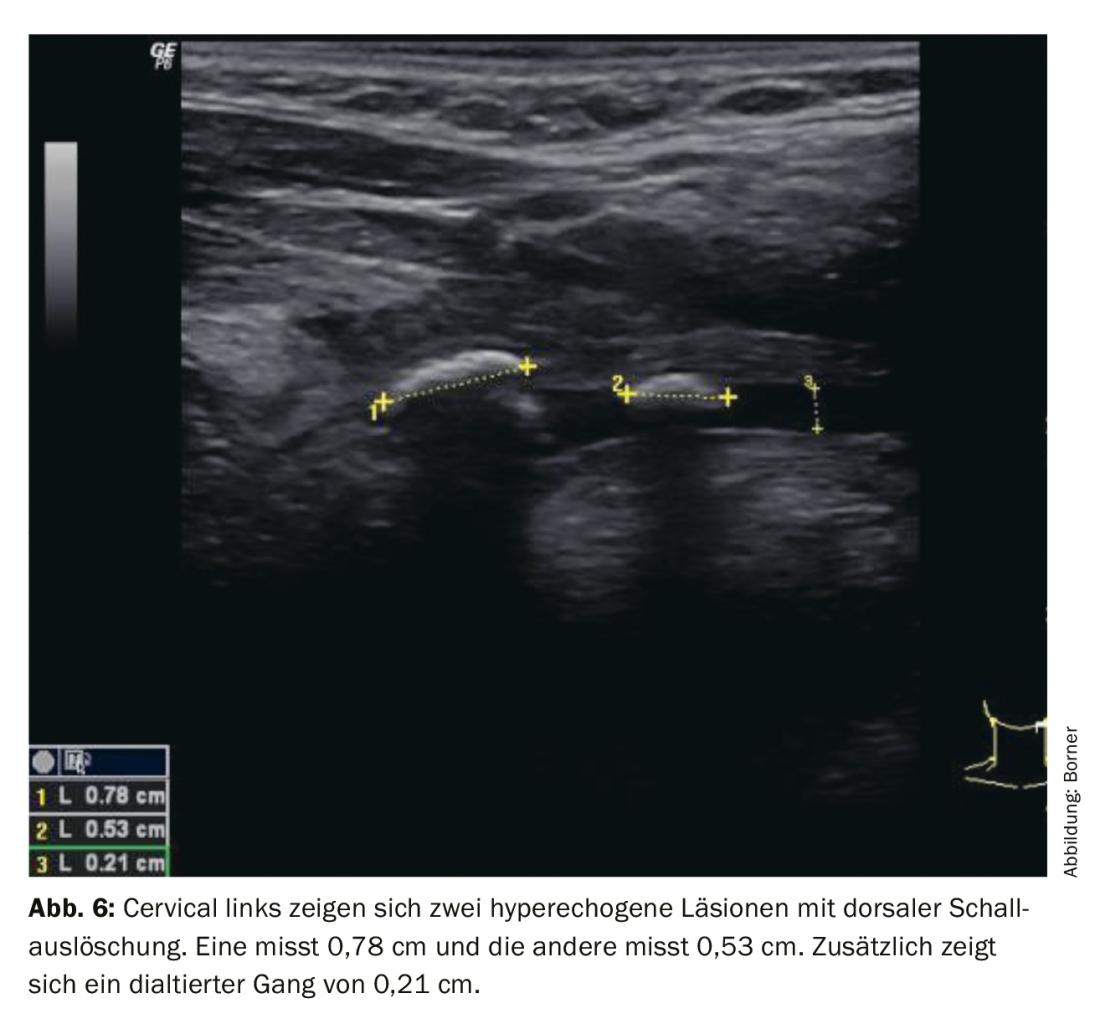
Salivary stones in the Gl. submandibularis are very often located in the area of the hilus of the gland. Ultrasonographically, there are direct signs (hyperechogenic surface) and indirect signs (dorsal sound extinction and dilated ductal system). For better visualization, it may help if the patient takes saliva-producing substances (candy, vitamin C) before or during the examination. This allows better visualization of the dilated duct system (Fig. 6). It is also important not to apply too much pressure with the probe. The salivary ducts are very fine and can be compressed by even a little pressure until they are no longer visible. We recommend using a lot of gel to create a gel layer between the transducer and the skin. This guarantees that not too much pressure is applied.
Pathologies in the floor of the mouth
Spacial lesions in the floor of the mouth often affect tongue mobility during speech and eating at a very early stage. A detailed clinical examination of the floor of the mouth, tongue and teeth is important. In particular, bimanual examination can be helpful. Ultrasonographically, it is important to distinguish whether the lesion is below or above the mylohyoid muscle.
The differential diagnoses for space-occupying lesions in the floor of the mouth are highly age-dependent. In younger patients, it may be a ranula, dermoid, teratoma, vascular malformation, or median neck cyst. Rarely, it may also be ectopic thyroid tissue. In elderly patients, tumorous change must be excluded. Ranula can occur at any age. A ranula is a clinical diagnosis. Ultrasound can be used to assess the extent.
If the cause of the swelling is unclear clinically and sonographically, a fine-needle aspiration must be performed to confirm the diagnosis.
Take-Home Messages
- Ultrasound examination is very helpful in the evaluation of unclear swellings of the neck, since almost all structures are easily accessible. The examination is inexpensive, without radiation exposure and can be performed quickly.
- It is important to adjust the workplace and the device well so that the basic conditions exist to sound accurately and with pleasure.
- Under the age of 40, inflammatory changes and congenital changes are the most common causes of swelling.
- After the age of 40, primary malignancies and especially metastases are significantly more frequent.
- Thyroid nodules are a common incidental finding. The nodes must be assessed and documented individually. Depending on the risk of malignancy and size, they are punctured or controlled.
Literature:
- Iro H, Bozzato A, Zenk J: Altas of head and neck ultrasound; Thiema.
- Müller T, et al: DEGUM Recommendations on Infection Prevention in Ultrasound and Endoscopic Ultrasound. Ultrasound in Med 2018; 39: 284-303.
- Amercian Thyroid Association Management Guidelines for adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer 2015.
- Rettenbacher T: Sonography of peripheral lymph nodes part 1: normal findings and B-scan criteria, Ultrasound in Med 2010; 31: 344-362.
- Leenhardt L, et al: European Thyroid Association Guidelines for Cervical Ultrasound Scan and Ultrasound-Guided Techniques in the Postoperative Management of Patients with Tyhroid Cancer. Eur Thyroid J 2013; 2: 147-159.
- Evaluation of Neck Masses in Adults; American Family Physician. 2015 May 15; 91(10): 698-706.
- Raza Pasha R, Golub JS: Book; Otolaryngology Head and Neck Surgery, Clinical Reference Guide,4th edition.
HAUSARZT PRAXIS 2020; 15(1): 16-21