The prevalence of rheumatoid arthritis (RA) is common and the onset of disease is mostly in early adulthood. That is, as a physician, you have many decades to work with patients, but only a very few weeks to achieve remission. How narrow this time window actually is was discussed at the DGRh congress in Dresden.
Rheumatoid arthritis (RA) is a systemic chronic inflammatory disease. So far, so well known and to be read in every textbook. In other words, rheumatologists are dealing with a disease that affects the entire body. It is chronic because there can be no spontaneous healing in a situation where the immune system has been instructed to destroy the body’s own tissues. “We know that our patients live 10 years shorter than the healthy population if untreated, but treated patients live 3 years longer than the healthy non-treated population,” explained Professor Hendrik Schulze-Koops, M.D., Rheumatology Unit, Medical Clinic and Polyclinic IV, Ludwig Maximilian University Hospital, Munich. “Because we are interfering with inflammatory mechanisms that put an end to life at many aspects in the body. We should be aware of that when we talk about remission.”
As the expert detailed, early adulthood is a phase when the patient is indolent. He does not come to a rheumatologist on his own initiative when the first symptoms appear. Instead, at best, he goes to the family doctor, who gives him a few pills. By the time he actually presents to a specialist, much that can be achieved with drug therapy has already been missed. In this context, Prof. Schulze-Koops emphatically pointed out that RA “is not a joint disease that hurts a little.” Rather, it is associated with significant comorbidity and mortality. And remission should refer to everything, including comorbidities, from cardiovascular disease to depression and osteoporosis, otherwise it’s not true remission.
Of crucial importance, he said, is the fact that it is an autoimmune disease. After all, an immune system is there to eliminate a danger as quickly as possible. The rheumatologist reminded us of the old rule of thumb that we usually suffer from an acute infection for exactly 9 days: 3 days activity, 3 days elimination, 3 days stop. “With RA, how long does it take to get to the doctor: 7 to 9 months.” During this time, the immune system has the opportunity to actively participate in eliminating the target from the patient. And the target is the connective tissue. This is where we need to start if we want to effectively bring more people with RA into remission in the future. Because if you continue to give the immune system a free hand against a microorganism and sometimes wait nine months before finally intervening (instead of the nine days it would take physiologically), then too much land is simply lost.
Pregnant is not a permanent therapy
Lane & Griffith defined RA as early as 1890 as one of the most refractory and intractable diseases that can affect the human body. Prof. Schulze-Koops also recalled a text from 1936 that stated that the easiest way to get a patient with RA into remission was to get pregnant. – “But it’s not like it’s a long-term therapy.” This example, however, shows how frustrating disease progression has been for many physicians to observe over the last century, he said. “Relatively complete” remissions were thus so rare that they were considered a medical curiosity.
Supply reality 2019
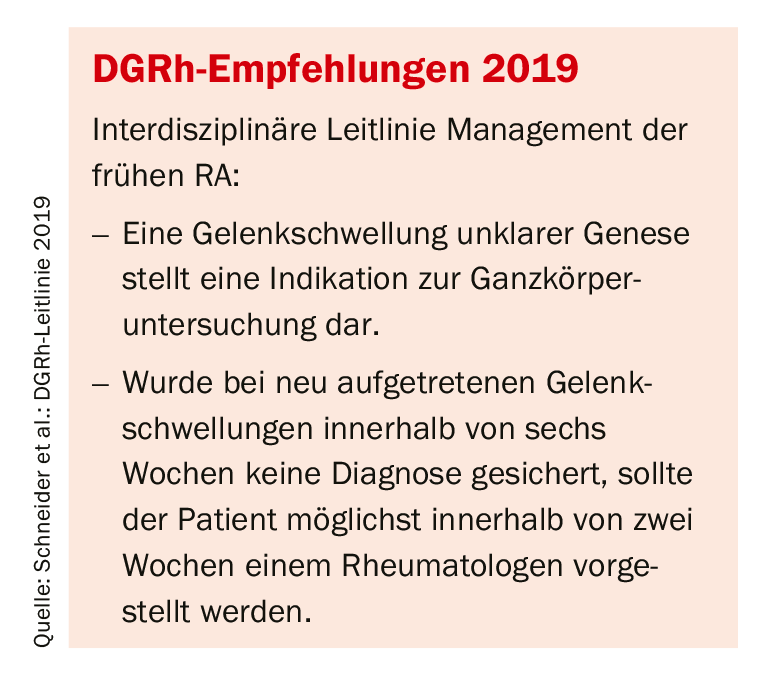
By contrast, the situation in 2019 has unquestionably improved – albeit at a still soberingly low level. Because of earlier detection, there is not as intense a progression as there was 30 or 40 years ago. Nevertheless, the reality of care with new biologics today is 25-30% clinical remission (Fig. 1). “But that can’t be the goal,” the expert put it succinctly.
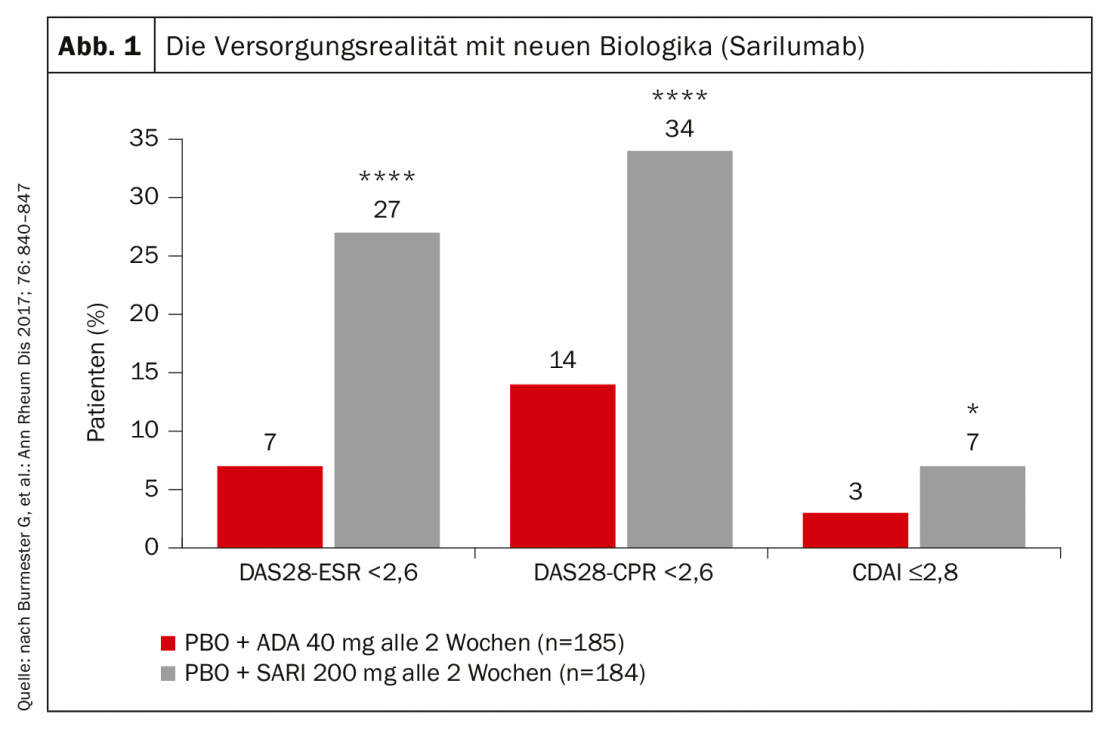
In the course of RA, the sites that are later radiologically conspicuous are created in the first year and are detectable. A patient with RA, completely x-rayed, has almost no erosion in the first 12 months. Between the first and second year, 70% of the erosion seen later can be predicted radiologically. The following year 100%. “In other words: If I wait 2 years with my patient until he is treated, all is lost,” says Prof. Schulze-Koops. “There is no radiologic remission that occurs on the ground of filling erosive changes” (Fig. 2).
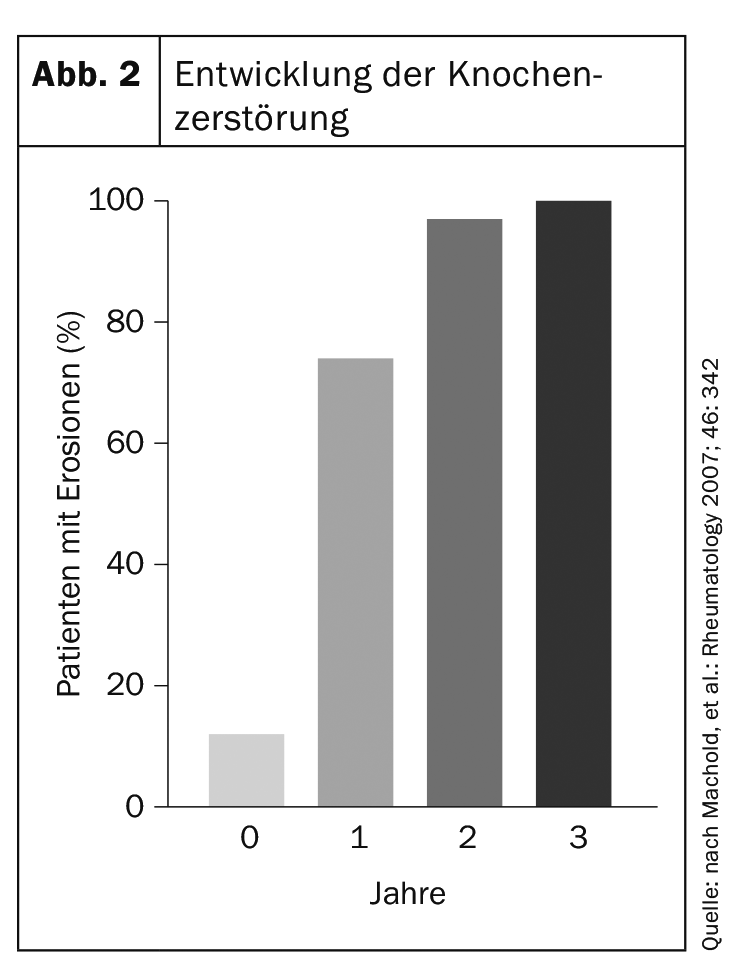
The course of the disease depends on the first weeks. A Swedish paper as early as 1995 randomized a group of patients to 8 months of placebo followed by DMARDs or to DMARDs from the start (Fig. 3). The radiological course shows that within the first 8 months the gap widens – and then widens even further, although the therapy is identical from that point on. “The later we get, the more functional deficits we have and the faster the momentum of destruction that we can’t recapture,” the rheumatologist concluded.
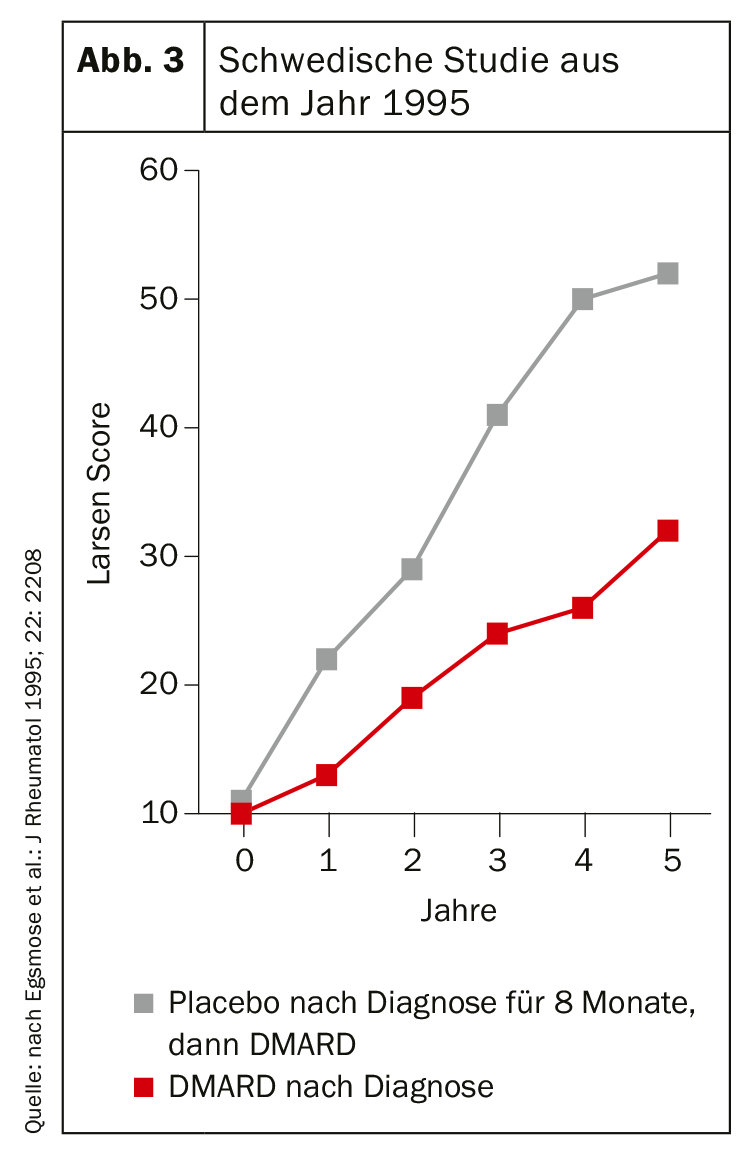
A few weeks are crucial
The duration of illness of outpatients at first contact with a rheumatologist averaged 2 years in 1994. In 2015, it was 7 months. That alone is unquestionably progress. However: the 2018 S2e guideline on RA therapy with disease-modifying drugs states that DMARD therapy should be started as soon as RA is diagnosed, and that the earliest possible start for newly diagnosed RA should be “optimally within 12 weeks of symptom onset”-not at 7 months.
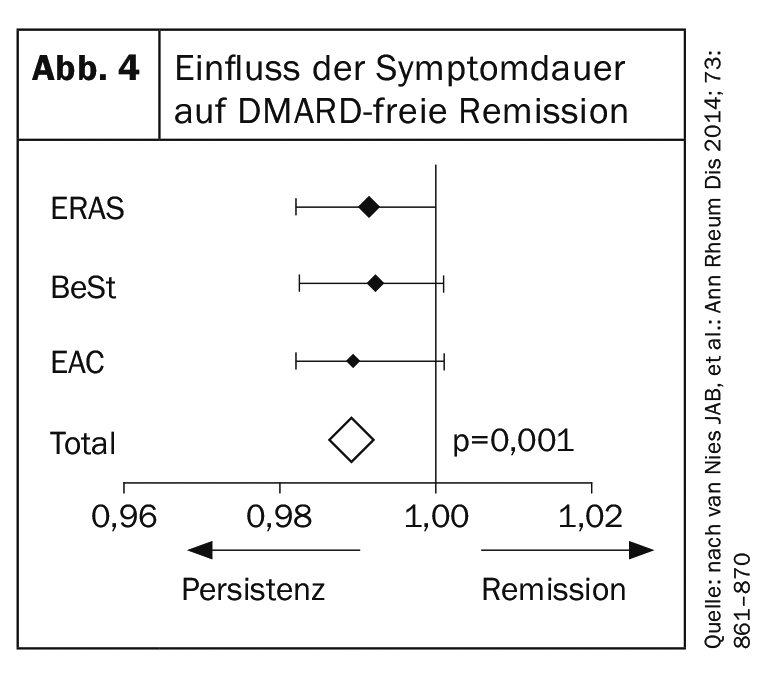
Why are these few weeks so important? – Prof. Schulze-Koops demonstrated it using data from a meta-analysis composed of the original remission induction studies of biologics (Fig. 4) . Here it was shown how high the probability is to ever bring a patient into remission. The time line represents one week. Consequently, each week of treatment delay reduces the probability of ever putting a patient into remission by 1%. “And now think: 7 months until a patient with RA is referred to a rheumatologist in Germany times 4 weeks (0.7×12×4) makes 34% – we lose one-third of the opportunity to put the patient into remission because of the way we introduce them to therapy.”
The fact that most patients only present when the immunological disease has already reached a level that makes it impossible to ever get RA under control again is, according to the expert, the central issue that rheumatologists will have to address in the future. Therefore, he concluded his appeal to colleagues to open arthritis consultations even earlier and instead prefer to postpone a patient with a chronic disease in order to get closer to the goal of remission.
Summary
- RA is common, runs a chronic course, causes severe destruction of bones and joints, and is associated with a number of life-threatening extramusculoskeletal manifestations.
- Early initiation of adequate immunosuppressive therapy can alter the course of RA and reliably prevent its characteristic complications.
- Each week (!) of treatment delay reduces the probability of ever achieving remission by 1%.
- RA is common, results in destruction of cartilage and bone, and is associated with significant comorbidity. It is a disease of the activated immune system and NOT a musculoskeletal pain disorder.
Source: Industry Symposium “Let’s talk about JAKs”, Organizer: AbbVie.
InFo PAIN & GERIATRY 2019; 1(1): 24-25 (published 11/24/19, ahead of print).
HAUSARZT PRAXIS 2019, 14(12): 20-22











