Even if children survive a malignancy, they are still at risk. Late effects resulting from therapy should not be taken lightly.
The survival rate of children and adolescents who develop cancer has been increased to over 80% in recent years. Nevertheless, their life expectancy is reduced because late effects resulting from cancer therapy cannot be ruled out. Up to 70% of all patients suffer from such health impairments 30 years after the end of treatment. These can affect different organs and potentially be life-threatening again, such as another cancer or severe heart failure.
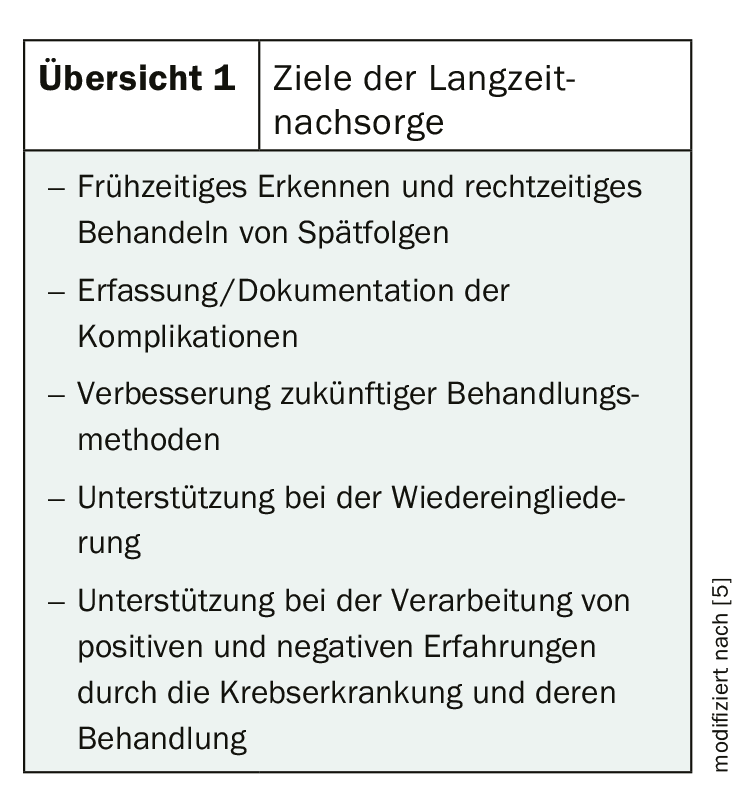
The risk of complications is influenced by individual factors such as previous diseases, age, gender and genetic predisposition. But of course the type of oncological therapy also plays a major role. Experts advocate an individualized follow-up plan, as many diseases can be treated well in the early stages. However, since the affected individuals then no longer fall under the purview of pediatric oncologists, an interdisciplinary approach is required.
The most common complications at a glance
The most common late effects can be found in the endocrine area. Endocrinopathies occur because radiotherapy can lead to dysfunction of endocrine organs. Thyroid disorders, hypothalamic-pituitary system disorders, or gonadal dysfunctions occur in more than one in two. The latter can be found mainly after chemotherapies. Radiation therapies are usually more likely to result in thyroid dysfunction or neoplasia.
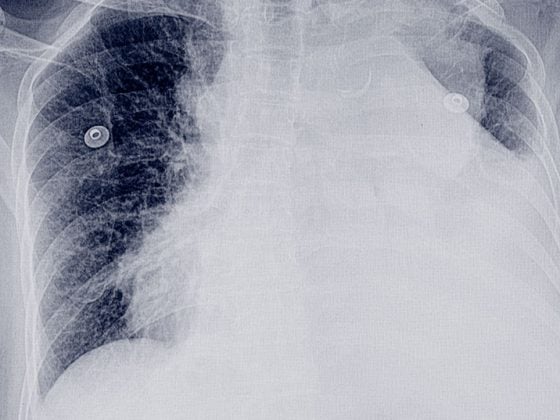
Serious and potentially life-threatening consequences include cardiac disease in particular. Cardiomyopathies, valvular changes, arrhythmias or coronary heart disease can be treated well initially, but often the right time is missed and the disease progresses. The likelihood of cardiac complications increases, especially with anthracycline-containing chemotherapy and thoracic radiotherapy. Affected individuals are seven to eight times more likely to experience early cardiac-related mortality.
Both radiation and chemotherapy can increase the risk of malignant neoplasms. Therefore, many long-term survivors of childhood or adolescent cancer are later affected again by hemato-oncologic disease. In the first 15 years after the end of therapy, hematologic diseases occur most frequently, after which mammary and thyroid carcinomas are more common.
However, other complications, such as decreased pulmonary function, neurological or neurocognitive late effects, or problems in the gastrointestinal tract, kidneys, or musculoskeletal system can also affect the patient. By optimizing the treatment options, an attempt is made to reduce the risk of late effects. However, they cannot yet be completely ruled out.
Further reading:
- www.awmf.org/uploads/tx_szleitlinien/025-003l_S1_Nachsorge_von_krebskranken_Kindern_Jugendlichen_06-2013-abgelaufen.pdf (last accessed on 2019-09-14)
- Kaatsch P, Spix C. German Childhood Cancer Registry – Annual Report 2017 (1980-2016).
- Bhakta N, et al: Lancet 2017; 390:2569-2582.
- Morton LM, et al: J Natl Cancer inst 2017; 109.
- www.kinderkrebsinfo.de/patienten/nachsorge/spaetfolgen___langzeitnachsorge/einfuehrung/index_ger.html (last accessed on 2019-09-14)
InFo ONCOLOGY & HEMATOLOGY 2019; 7(4): 22.