Not infrequently, the general practitioner is also confronted with dermatological clinical pictures. Which finding is harmless and when should referral to the specialist be made?
Eczema, fungus or parasitic infestation? Benign or malignant skin lesion? Pathologic skin lesions are common in family practice. However, because of the marked diversity of morphologic findings, dermatologic clinical pictures are often confusing to non-dermatologists. The most efficient initial assessment is based on the following:
- Red spot – localized
- Red rash – generalized over a large area
- Black spot – localized
- White spot – generalized or localized
- Warning symptoms
Reddish spot: asymmetric infestation
The most important criterion in skin florescence presenting as a localized red or reddish patch is asymmetry vs. symmetry.
Attention must be paid to asymmetric skin florescences: Any unilateral redness that is more painful than itchy is considered an infection – until proven otherwise. An infection is either bacterial (e.g., impetigo, erysipelas, or Lyme disease), viral (e.g., varicella in the form of zoster), or mycotic (e.g., tinea capitis or tinea barbae). Infectious skin florescences may occur all over the body (Fig. 1 and 2) . Possible additional symptoms are swelling of the lymph nodes, fever and/or general feeling of illness. Consider a dermatologic consult if infection is suspected. Timely recognition and action are elementary.

Reddish spot: Symmetrical infestation
In the case of symmetrical skin florescences, the time factor is secondary: these are unpleasant for the patient, but not dangerous. The two most important criteria here are with vs. without itching, and additionally, for itchy patches, rough vs. smooth.
Rough surface with itching: Eczema is the most common skin condition. They occur in all age groups – including children – and can show up all over the body. Identifying feature of this inflammatory, non-infectious disease: The skin is rough in the affected area, usually itchy and scaly. Regular basic care with a lipid-replenishing product is indispensable for relapse prevention, as is the identification and prevention of trigger substances (Fig. 3).

Exsiccation eczema is the most common form of eczema. It is caused by excessive contact with water: Water is the most common noxious agent – too much water dries out the skin. Reducing water contact to the minimum necessary is the most important therapy. Greasing is of little use if contact with water is not reduced. When washing hands and showering, it’s not so much what is used for it, but that the skin is consistently cared for afterwards.
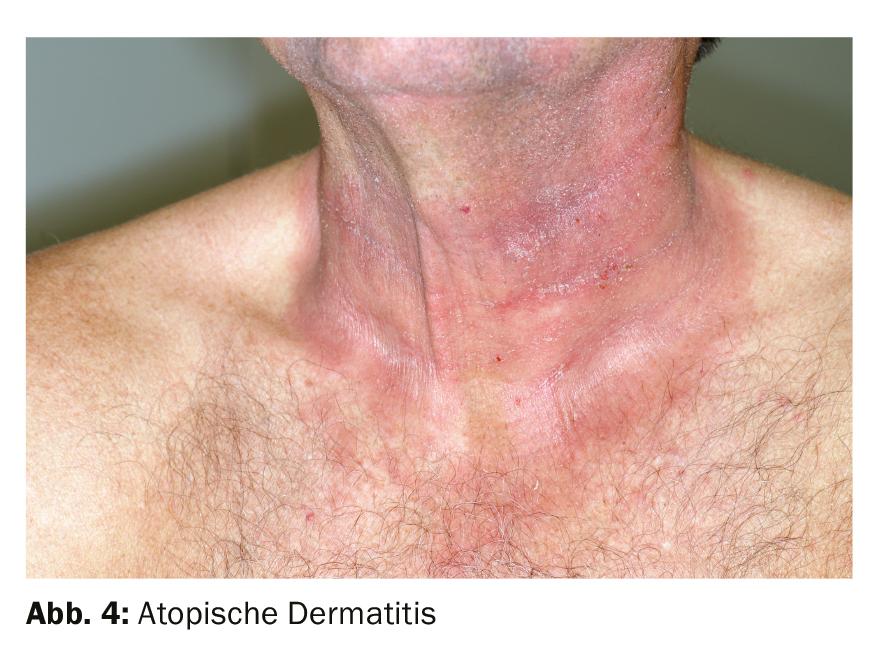
Atopic dermatitis is also widespread. The flare-ups of this chronic disease vary in severity and duration. The eczematous rashes that develop during an episode range from mild skin lesions to large-scale inflammation. The skin is not only red, rough, very itchy and scaly, but sometimes even oozes and crusts. The eczema can move from one part of the body to another. In infants, the scalp, cheeks, arms, legs and trunk are often affected – less frequently the diaper area. In school children and adults, the eczematous rashes are usually found in the bends of the arms and knees, but also on the face, neck and hands. In many patients, the symptoms subside with the end of puberty. However, atopic dermatitis can also first appear in adulthood. For symptom relief, urea-containing skin care products are often counterproductive; especially if used at the wrong time – during an acute flare. Treat itching in the setting of atopic dermatitis primarily with topical steroids; only secondarily with antihistamines. The combination of steroids with Fucicort, for example, is important here. Monotherapy with steroids often leads to relapse (Fig. 4).
Smooth surface with itching: A smooth, itchy area is often urticaria or drug exanthema, although the majority of these two skin florescences present as a generalized red rash.
Rough surface without itching: Chronic inflammatory, non-infectious psoriasis presents with sharply defined, bright red, dry and raised plaques covered by silvery scales. Often affected are elbows, knees and scalp. The most common mistake in the treatment of psoriasis is too weak steroids. Those who treat with steroids need potent steroids (class 3 or 4) or fixed combination preparations (steroid class 3 and vitamin D) for a good effect ( Fig. 5).

Solitary with rather smooth surface without itching: A basal cell carcinoma can also appear reddish, often it is additionally interspersed with whitish. This common semimalignant tumor forms reddish-whitish-brownish, shiny nodules with typically very fine red veins at the tumor margin. The rim is usually raised. The coloration often corresponds to that of normal skin. In the early stage, the skin at the affected area initially hardens. In the later course, the affected area often appears centrally sunken and ulcerated. Light-skinned, sun-sensitive individuals are particularly affected, usually in the second half of life. Basal cell carcinoma develops slowly over months to years. It can occur anywhere on the body, but most commonly on sun-exposed areas of the body such as the face, ears, scalp and neck. Basal cell carcinoma needs mandatory dermatologic evaluation. Although it does not usually metastasize, early treatment is very important: if left untreated, the growing tumor destroys surrounding healthy tissue (Fig. 6).

Reddish rash without itching
The most important criterion for skin florescence that appears generalized over a large area as a red or reddish rash is the presence or absence of pruritus. Rashes without itching can be further divided into smooth or solitary rough rashes.
Smooth: A red, generalized rash without itching is parainfectious exanthema (also called paraviral or infectious exanthema). The rash is caused by different viral pathogens. The most common are Epstein-Barr virus (mononucleosis) and measles-mumps-rubella virus. Bacterial pathogens are also possible, for example streptococcus (scarlet fever). The smooth rash appears as large round to oval red spots or papules – first pale red, then dark red. It is practically always additionally accompanied by exanthema of the oral mucosa. Fever and general symptoms are also common. Parainfectious exanthema can occur anywhere on the body. It often shows on the trunk, but the face and extremities can also be affected. In this case, it is a case of wait and see: no therapy is the best therapy for parainfectious exanthema (Fig. 7).

Solitary rough: Actinic keratosis also often does not occur as a single spot, but rather in small groupings or distributed over a large area. The rough, slightly thickened and scaly skin areas are reddish to reddish brown, sometimes crusty yellowish. The affected areas are often more palpable than visible and feel like sandpaper. Actinic keratosis occurs in the majority in the second half of life – especially in fair-skinned, sun-sensitive individuals who have often been exposed to the sun. Typically, it shows up on the “sun terraces of the skin” – especially the bald head, forehead, nose, ears, lips as well as the décolleté, back of the hands or forearms. The epidermal light damage to the skin usually remains permanently visible. It is imperative that you have an actinic keratosis dermatologically evaluated. It is considered a precancer: if left untreated for too long, it can develop into malignant squamous cell carcinoma (Fig. 8).

Reddish rash with itching
The two most important criteria for large-area generalized red skin florescences with pruritus are nodular vs. smooth and, in the case of a smooth rash, additionally stationary vs. migratory.
Nodular: Varicella, caused by varicella zoster virus, presents with episodic flare-ups of small red spots all over the body. The spots quickly turn into papules and vesicles that crust over time. Unlike all other infectious exanthemas, varicella is intensely itchy. In addition, enanthema of the oral mucosa is usually seen. Varicella first begins on the head and oral mucosa, then the trunk and extremities are affected. Palms and soles, on the other hand, are not involved. For varicella, the focus is on drying – not rehydrating – treatment (Fig. 9).

Smooth with a wandering course: Urticaria is one of the most common skin diseases and looks like an allergy at first glance. However, urticaria is very rarely caused by a type I allergy (immediate type or IgE-mediated in less than 1% of cases), but is usually physical or emotional. Urticaria caused by histamine overproduction is superficial dermal. It presents with reddish wheals, always smooth, distributed in spots or over a large area. Often these are rather small-spotted. However, wheals the size of the palm of a hand are also possible. An urticaria flare-up often develops very quickly: within a few minutes, the skin is covered with intensely itchy wheals. These are local or spread over the whole body. In the course they migrate over the body and usually disappear after 24 hours at the latest without leaving any traces. However, a relapse can also last several days or even weeks. It is important in the diagnosis of urticaria to distinguish it from drug exanthema. This often requires a biopsy. Urticaria should be treated with antihistamines, often in higher doses (up to five times a day). Fixed preventive use of antihistamines is important (Fig. 10).

Urticaria in combination with angioedema is an emergency that requires rapid dermatological evaluation: In addition to the symptoms of urticaria, angioedema is characterized by severe subcutaneous swelling of the hands, feet, nose, lips, eyes or penis. In this case, avoid urticaria-promoting drugs unless they are vital indicated or irreplaceable. These include ACE inhibitors, AT2 antagonist, aspirin, and non-steroidal anti-inflammatory drugs. Likewise, refrain from using codeine-containing antitussives.
Smooth with stationary course: Drug exanthema manifests itself in patchy redness (Fig. 11) . In cases of severe intolerance, these are usually extensive. The affected skin areas are overheated and itchy. Drug exanthema is an allergic reaction of the skin to a locally applied or ingested drug (such as an antibiotic). It typically manifests in the trunk area, but can also occur elsewhere on the body. This skin reaction occurs in all ages, including children. Drug exanthema is more common in older people because they usually take more medications, increasing the likelihood of intolerance. Drug exanthema appears smooth at first but may become rough as it progresses. Differentiation from eczema is difficult. Unlike eczema, drug exanthema does not appear scaly. The most important distinguishing feature is time: drug exanthema occurs suddenly, usually within hours, days, or overnight. Discontinue the locally applied or ingested medication immediately. Pain, erythroderma and additional blistering of the skin, mucous membrane or conjunctiva or palmoplantar rashes on the palms or soles of the feet are signs of a life-threatening reaction!

Black or dark spot
If there is a black or dark localized spot, the suspicion of melanoma is obvious. The most important assessment aids here are the “ugly duckling sign” and the ABCD rule. Use the “ugly duckling” rule to get an overview. First, look at the patient from a distance. If the black or dark spot is clearly distinguishable as an “ugly duckling” in basic shape and basic color from the other black and dark spots on the body, a dermatoscopic examination is quickly needed. It is also possible to examine the image using the four criteria of the ABCD rule: A: Asymmetric, B: Blurred, C: Multicolor, D: Dynamic. If at least one of the four criteria applies to the spot, there is an urgent suspicion of melanoma. A suspected melanoma cannot be confirmed by eye. Only a biopsy brings certainty.
| Tip Our reference book “Derma Survival Guide – how to survive in dermatology” provides more certainty in diagnosis and triage: It supports you with guiding questions, diagrams and photos very practically in the rapid assessment of skin changes. Order at www.derma-check.ch |
Melanoma arising from melanocytes is the most dangerous form of all skin tumors. It presents as a skin change asymmetrical in shape and color in an existing or newly appeared dark spot. Commonly seen as a dark to black spot that may be flat, domed, or nodular (Fig. 12) . Melanoma can occur anywhere on the body. Melanoma occurs in all age groups – including children. Light-skinned people are much more likely to be affected than dark-skinned people. In principle, melanomas are very common. However, thanks to early detection, they are easily treatable. Timely diagnosis prevents fatal courses: the chance of recovery is 99% with early intervention and drops to 14% in later stages. Clarify every newly appearing or already existing, changing black or dark spot obligatorily dermatoscopically – better once too much than too little! The workup should be done quickly so that the melanoma can be removed before it metastasizes, if possible.

The birthmark, a benign growth of melanocytes, appears as a symmetrical black or dark spot. It has regularly bordered edges, is homogeneously of the same color and has the same size over a longer period of time (Fig. 13).

The frequently occurring seborrheic keratosis may also appear as a black or dark spot and therefore be mistaken for melanoma (Fig. 14) . However, this typical feature of aging skin is a benign growth, unlike melanoma. Seborrheic keratosis presents in an early stage with flat, dull patches or plaques, and later as sharply demarcated, roundish to oval, fissured, raised growths. From black to gray to dark and light brown, various shades are possible. The lump is a few millimeters to several centimeters in size, occurs singly or multiple times. The number increases as the age of the affected person increases. The chest, back and neck are particularly affected, but also the face or the extensor sides of the hands and forearms. The palms of the hands and soles of the feet are not affected. In the case of dark seborrheic keratosis, a rapid dermatological differential diagnosis to malignant melanoma is mandatory.
White spot
Most important differentiation criterion for flat, localized or generalized white patches is body trunk vs. extremities.
Pityriasis versicolor , a harmless superficial fungal disease occurring on the trunk of the body, presents with hyperpigmented, scaly, round to oval patches. These may be reddish, pinkish, yellowish or brownish in color – in pityriasis versicolor alba the patches are hypo- or depigmented. The spots are found on the trunk of the body, especially in areas with high sebum production. With pityriasis versicolor, relapses readily occur. To reduce this risk, regular skin care is important (Fig. 15).

The most important criterion for white patches on the extremities is sharply or indistinctly defined. In harmless vitiligo, the patchy loss of the original skin color shows up in sharply defined white patches. Vitiligo usually appears before the age of 20. The spread of the spots is extremely variable: it can remain with a few areas or a generalized spread can occur over large parts of the entire body. The spots do not show any symptoms – neither itching, nor scaling. Vitiligo often begins on sun-exposed areas such as the hands, face (especially eyelids, mouth area) or back of the feet. The genital area is also frequently affected. Very good protection from UV radiation is especially needed for vitiligo.
A white, fuzzy, dry patch is from a healed eczema, a healed eczematous area of atopic dermatitis, or a healed injury. Such stains disappear by themselves after some time without treatment.
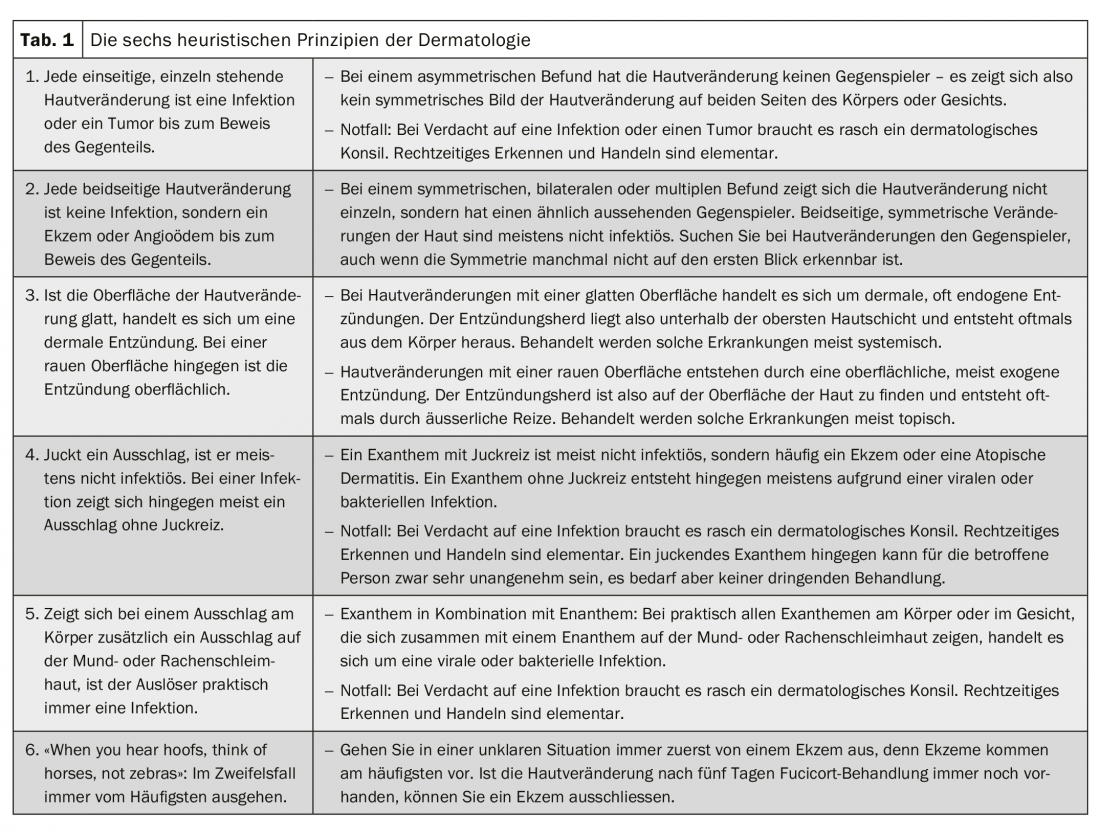
Heuristics help
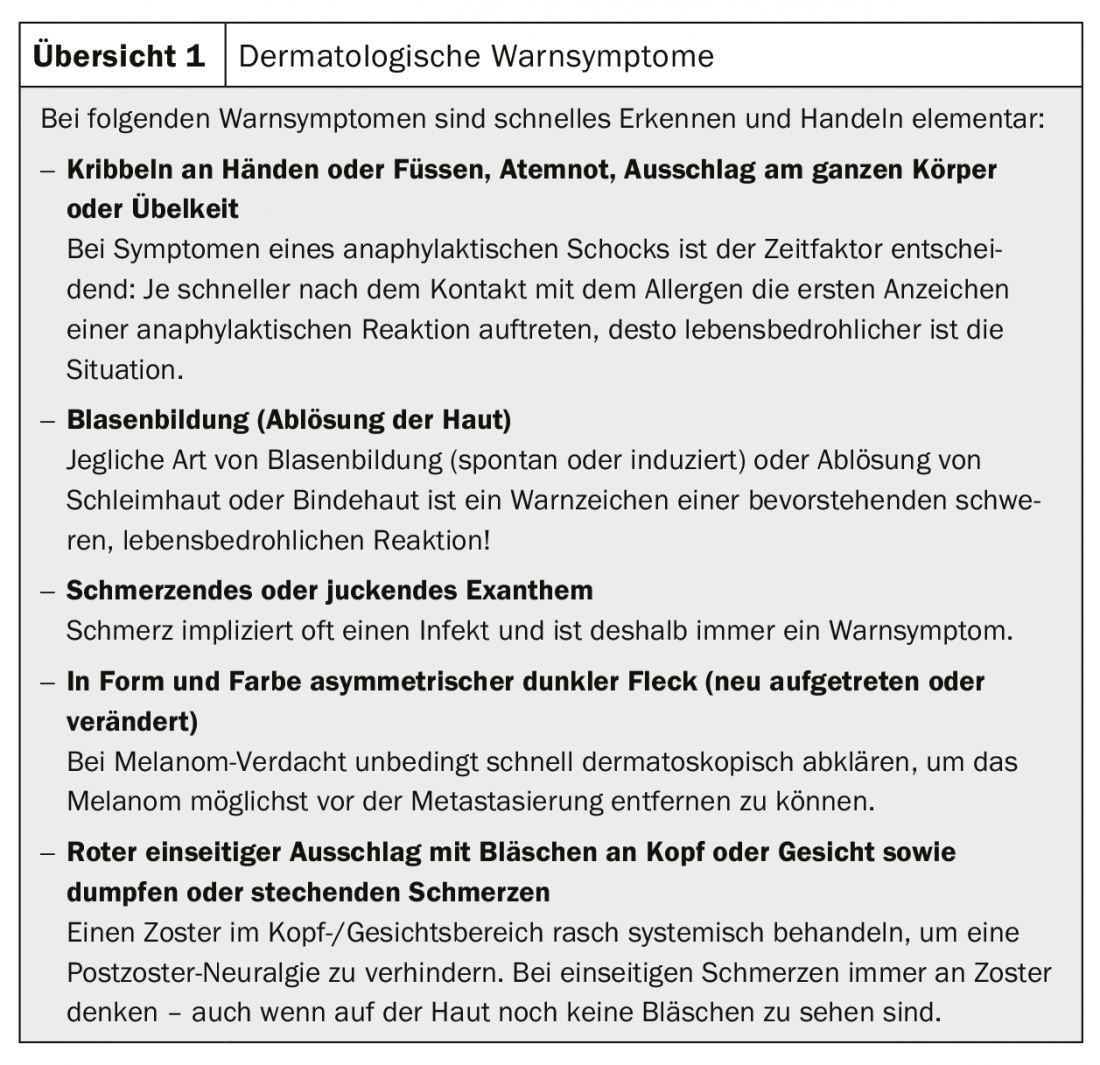
In everyday practice, decision algorithms are needed for rapid and safe triage of skin florescences. The most important question here: Is the skin change potentially dangerous? With the help of the six heuristic principles, you can quickly distinguish between dangerous and harmless. Heuristics, which have been practiced since ancient times, are nothing more than a shortcut to thinking when solving your question. It allows you to arrive at a workable statement despite having little time. Table 1 explains the six heuristic principles of dermatology; in everyday practice, the first, fourth, and fifth heuristic principles are crucial: If there is an urgent suspicion of an infection or tumor, a rapid dermatological consultation is indicated. Overview 1 provides information on warning symptoms.
Take-Home Messages
- Any unilateral, solitary skin lesion is an infection or tumor until proven otherwise.
- Any bilateral skin lesion is not an infection but eczema or angioedema until proven otherwise.
- If the surface of the skin change is smooth, it is a dermal inflammation. With a rough surface, on the other hand, the inflammation is superficial.
- If a rash is itchy, it is usually not infectious. In the case of an infection, on the other hand, a rash usually appears without itching.
- If a rash on the body is accompanied by a rash on the mucous membranes of the mouth or throat, the trigger is practically always an infection.
- When in doubt, always start from the most frequent.
HAUSARZT PRAXIS 2019; 14(5): 19-28











