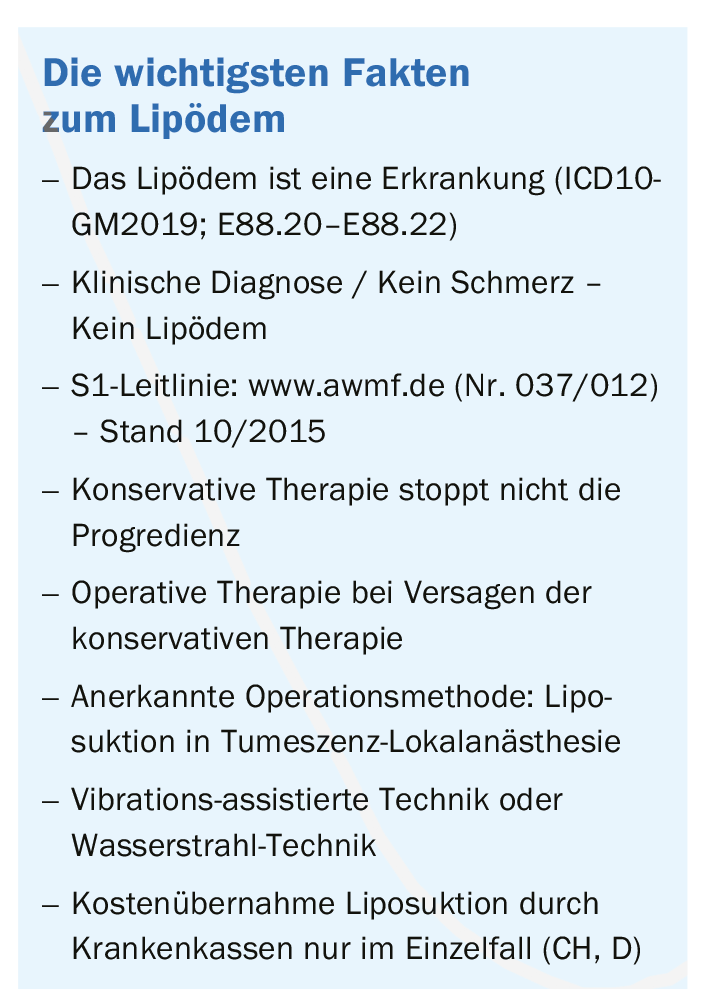
Guideline-based treatment of lipedema is based on four pillars. In case of insufficient effectiveness of conservative treatment, surgical therapy is recommended (liposuction).
The disease is defined by circumscribed, symmetrically localized subcutaneous adipose tissue proliferation of the legs, and less commonly, the arms. Characteristic is the increased sensitivity to touch and pressure pain in the affected body regions. Edema is also typical, as is a tendency to hematoma after minor trauma.
Diagnostic classification
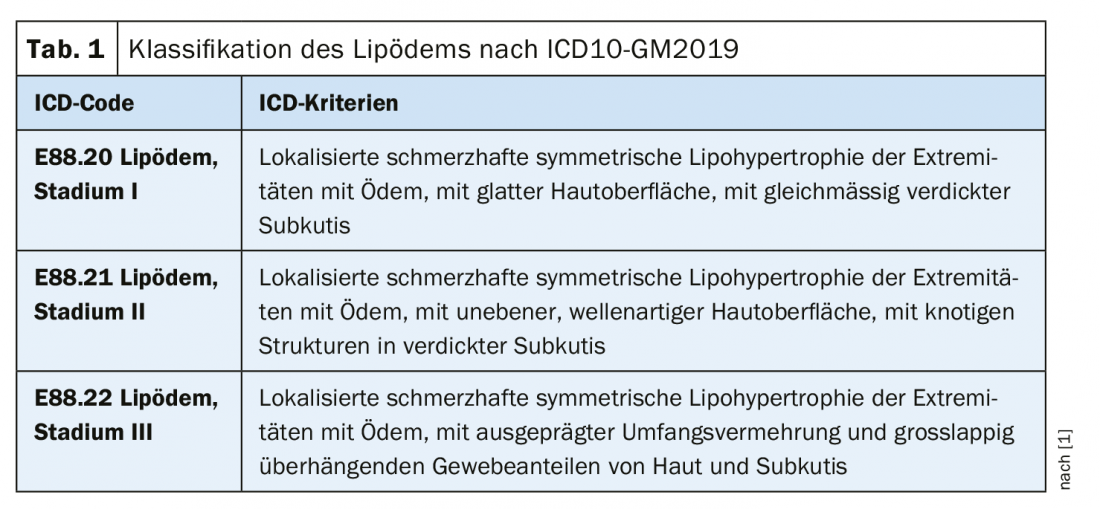
Since 2017, the disease lipedema has been statistically classified internationally. In the ICD10-Catalog-German Modification, the disease lipedema is listed stage-dependent (stage I-III) in the category “Other metabolic disorders” (ICD10-GM2019: E88.20-E88.22) (Table 1) [1].
The disease affects almost exclusively women and occurs during periods of hormonal changes, such as puberty, during pregnancy, or more rarely during menopause. It is estimated that about 5% of Swiss women suffer from lipedema. Unfortunately, valid epidemiological data from larger studies are not available. Familial clustering is observed in about 60% of cases. Individual case reports of affected men are associated with hormone therapies or disorders (e.g., hypogonadism) or liver cirrhosis. The etiology of the disease is as yet unknown. The pathomechanisms and especially the specific role of hormones or hormone receptors remain unclear and are subject to research efforts.
Previously commonly used synonyms for the condition: lipomatosis dolorosa, lipohypertrophia dolorosa, lipohyperplasia dolorosa, adiposity dolorosa, lipalgia, adiposalgia, painful lipedema syndrome, painful columnar leg.
The diagnosis of lipedema is made exclusively on the basis of clinical criteria. Anamnesis, inspection and palpation lead to the typical characteristics here:
- Female patient
- Onset of disease during puberty, pregnancy or menopause
- Disproportionate, symmetrical fat tissue proliferation on the extremities
- Caliber jump proximal joints – hands and feet – are not affected
- Painfulness on palpation
- Feeling of heaviness and tension, edema
- Hematoma tendency
The increase in adipose tissue is due to hyperplasia and hypertrophy of fat cells in the area of the affected extremities.Due to a capillary permeability disorder, excessive fluid enters the interstitium. The lymphatic system initially reacts to this with increased lymphatic transport. Due to a resulting high-volume transport insufficiency, the subcutaneous fat and connective tissue can no longer be sufficiently drained, and edema develops. The delayed and decreased veno-arterial reflex also promotes orthostatic edema. Over the course of many years, secondary lymphedema, fibrosis of the subcutaneous fatty tissue, sclerosis and papillomatosis of the dermis may develop. Increased capillary fragility is causative for the increased hematoma tendency.
Differential diagnostics
First and foremost, lipohypertrophy, obesity and lymphedema must be considered as differential diagnoses (Tab. 2) . This differentiation of lipedema is also based on clinical features: Fat proliferation, disproportion, edema, pressure pain, and hematoma tendency. All five characteristics are exclusively fulfilled in lipedema. The guiding criterion in lipedema is pain. Without pain symptoms, lipedema is not present. In lipohypertrophy, with the aesthetically disturbing breeches symptomatology, edema and tenderness are absent, and a hematoma tendency may be present. Obesity usually does not show disproportion, edema is possible, pressure pain and hematoma tendency are not present. The diagnosis of lymphedema runs through the edema, disproportion is present, fat proliferation is possible; usually there is asymmetry. Pressure pain and hematoma tendency are not present in lymphedema.
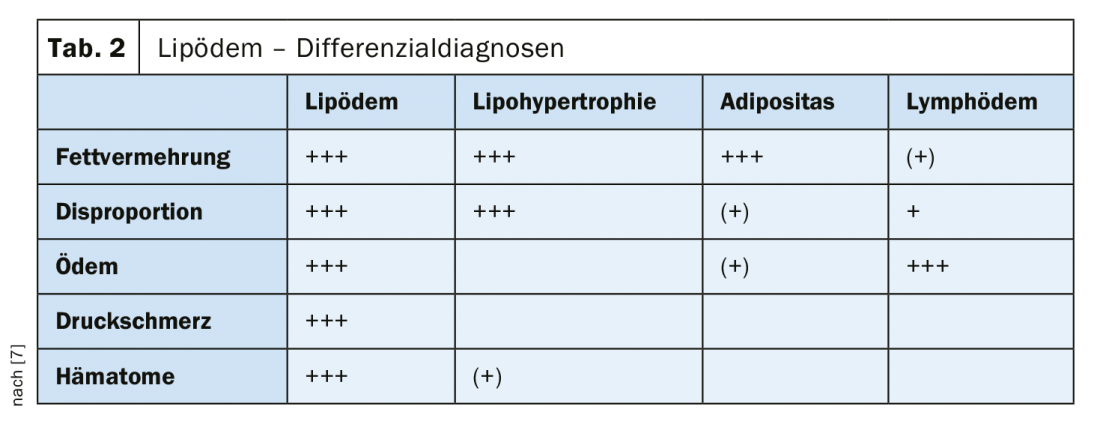
Other differential diagnoses include phlebedema (edema and skin sign of chronic venous insufficiency), myxedema in thyroid dysfunction (doughy edema), and combined disorders: Lipedema with secondary lymphedema, lipedema with concomitant obesity, obesity with secondary edema (adiposity edema), obesity with fibromyalgia.
Progress monitoring
The following parameters are suitable for monitoring the progression of lipedema: Body weight, body mass index (BMI), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), and circumference and volume measurements of the extremities (perometry). An elevated BMI can be misleading in lipedema; the WHR is usually clarifying in this case. These parameters are also helpful in cases with difficult differential diagnosis, e.g. differentiation of lipedema from obesity.
Morphologic examinations and functional studies of the lymphatic system are not diagnostic in lipedema and therefore are not required in routine clinical practice. Even the frequently used high-resolution sonography does not show any specific criteria in the diagnosis of lipedema.
The disease lipedema is chronic-progressive, individually very different and unpredictable. The classification is based on localization on the one hand and on morphology on the other (stage I-III, Fig. 1). A distinction is made between the whole leg, thigh and lower leg types in the lower extremities and the upper arm, whole arm and forearm types in the upper extremities. In each case, the order mentioned reflects the frequency of occurrence in a decreasing trend.
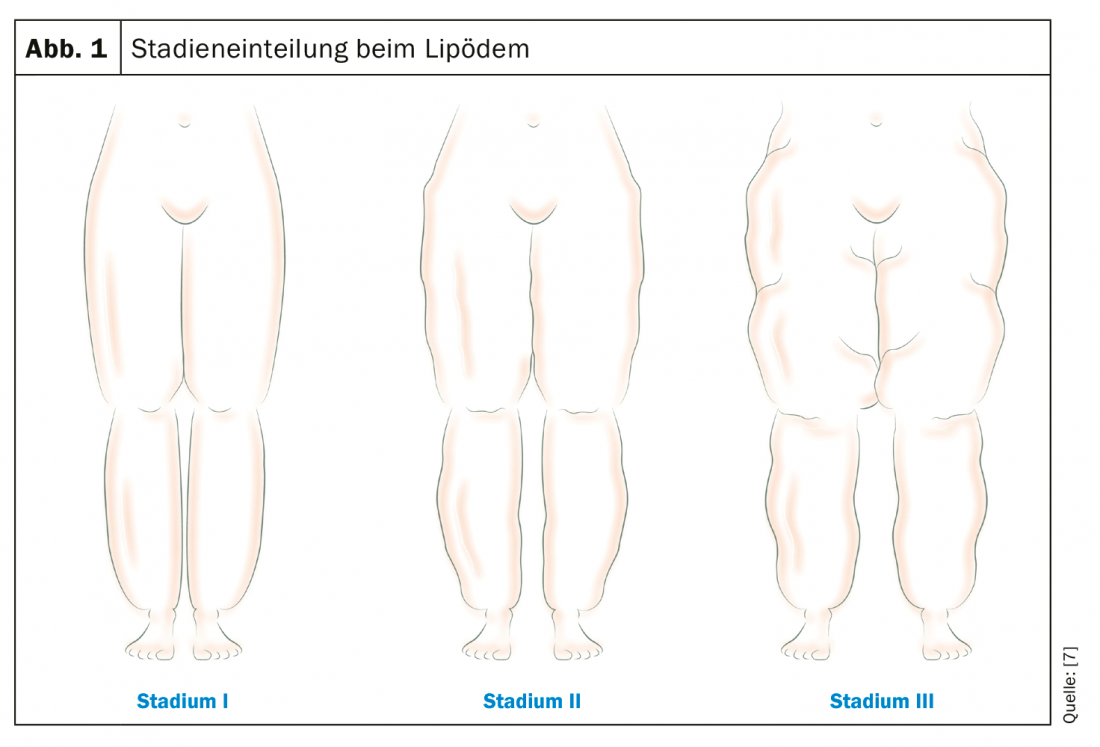
The stage can be defined by the following morphological characteristics:
- Stage I: Smooth skin surface with uniformly thickened, homogeneously imposing subcutis
- Stage II: Uneven, predominantly wavy skin surface, nodular structures in thickened subcutis
- Stage III: Pronounced circumferential proliferation with overhanging tissue portions (dewlap formation)
A smooth transition from stage I to stage II or stage III is possible depending on the course of the disease. However, the intensity of symptoms in lipedema does not correlate with the level of the stage. Pain may be much more pronounced in stage I than in advanced stages II or III. Photo documentation can therefore very often not do justice to the symptoms and the suffering of the patients; unfortunately, in many cases the aesthetic component is in the foreground.
Therapy guidelines
Treatment of the disease is aimed at symptom relief or symptom freedom (pain, edema, and disproportion) and prevention of complications. In advanced stages, the risk of complications increases (maceration, bacterial and mycotic skin infection, lymphedema, erysipelas, leg and foot deformities with valgus-gonarthrosis, gait disturbances with functional effects).
There is no known causal therapy for lipedema. The symptomatically effective measures are combined individually and adapted to the symptoms.
Since October 2015, the completely revised, updated version of the German S1 guideline Lipedema (AWMF register number: 037-012) is available [2]. The guideline-compliant therapy of the disease consists of a total of four pillars:
- Conservative therapy: This includes complex physical decongestive therapy (CPD), with an initial decongestive phase by means of bandaging (1-2 weeks) and an immediately subsequent maintenance phase with manual lymphatic drainage treatments (MLD) 1-2 times a week in combination with consistent, daily compression therapy (flat-knitted corsetry class II), exercise therapy and skin care. Apparent intermittent compression (AIK) is available as a supportive measure for decongestion and edema reduction, but cannot replace MLD and compression.
- Surgical therapy: This is clearly defined as fat tissue reduction by means of liposuction under tumescent local anesthesia (vibration-assisted technique [VAL] or waterjet technique [WAL]) using blunt microcannulas that are gentle on the tissue, and if necessary the subsequent removal of excess skin and tissue flaps by means of plastic surgery measures.
- Dietary change: An accompanying dietary change is often useful even in normal-weight patients, but in any case for body weight reduction in cases of concomitant overweight or obesity. Blood glucose and insulin spikes should be avoided, and sufficient breaks between meals should be observed (isoglycemic diet). There is no universal, lipedema-specific dietary recommendation.
- Exercise intensification: Increasing physical activity is recommended. Exercises in the water (swimming, aqua-jogging, aqua-aerobics, aqua-cycling, etc.) are particularly effective. In water, joints are relieved of body weight, lymphatic flow is stimulated by water pressure, and more energy is expended by exercising against the resistance of the water. Furthermore, sports exercises with movement on the trampoline are favorable.
In individual cases, psychotherapeutic support can be very useful. Many patients feel stigmatized by the disease with its disproportionate appearance, its conservative therapy, the daily wearing of compression garments and the time-consuming regular lymphatic drainage. In addition, it is not uncommon for doctors and family to advise weight reduction and more exercise for years, but the clinical picture remained undetected. Patients felt guilty and helpless, seeing themselves unable to tackle their apparent obesity. Whereby it is also not a question of motivation. The fact that eating disorders or real overweight are added to this is very well explainable.
Drug therapy or diuretic therapy to eliminate fluid retention in the legs is not indicated in lipedema, with or without secondary lymphedema. Drug-induced fluid withdrawal in the interstitium leads to increased protein content in the tissue and thus secondarily to increased edema.
The treatment goal of conservative therapy for lipedema is edema reduction, pain relief, and reduction of hematoma tendency. As a rule, conservative therapy accompanies the patient for the rest of her life and sometimes massively restricts the quality of life.
Wearing the firm, custom-made, flat-knitted compression class II corsetry (with a seam at the back) – often made in two parts: e.g. capri pants and knee sock or cycling pants and thigh sock to facilitate donning – is particularly necessary in the hot season, but then especially difficult to tolerate.
The progression of the disease can be stopped exclusively by means of a surgical measure, liposuction under tumescent local anesthesia. It is an established and low-risk, tissue-sparing surgical method with the help of which the excess fat cells can be removed in a targeted and permanent way up to 85%. The procedure results in pronounced improvements in spontaneous pain, pressure pain, edema, hematoma tendency, range of motion, body shape in up to 90% of cases, thus increasing quality of life and self-esteem in patients. In some cases, conservative therapy can then be dispensed with completely.
Health policy situation
According to the assessment of the Joint Federal Committee (G-BA), the scientific studies on the surgical treatment of lipedema are currently insufficient for liposuction to be recognized as a benefit by the statutory health insurance funds in Germany. By decision of the G-BA of 18.01.2018, a trial guideline liposuction was issued to review the benefit of liposuction in Germany within the framework of a multicenter study yet to be initiated [3].
The petition of the Lipedema Switzerland Association submitted to the National Council in the Federal Parliament in June 2017 with the request to adjust the benefits catalog of the compulsory health care insurance (OKP) with regard to the treatment measures for lipedema led to a review of the situation.
The Commission for Social Security and Health recommends to the National Council in its report of 15.11.2018 not to follow the petition, as it considers the request to be fulfilled [4]: “In the opinion of the Commission, an adjustment of the benefits catalog of the mandatory health care insurance is not necessary, as the costs of the mentioned services are already covered today. A prerequisite for the assumption of costs at the expense of the OKP is a confirmed diagnosis of lipedema with clear differentiation from an extremity-emphasized obesity without lipedema. Lipedema falls into the category of rare diseases due to the small number of cases. Problems in the assumption of costs by the insurers are not due to missing positions in the Krankenpflege-Leistungsverordnung (KLV; SR 832.112.31), but rather to insufficient knowledge about the disease among some of the physicians. The Commission therefore suggests to the Lipedema Switzerland Association to seek contact with the Swiss Society of Medical Officers and Insurance Physicians (SGV) so that the topic is taken up in the context of the SGV’s further training and in the manual of medical officers and thus the level of knowledge about this rare disease is expanded.” The National Council rejected the petition with date of 14.12.2018 [5].
In the manual of the Swiss Society of Medical Consultants and Insurance Physicians SGV, the topic of lipedema was already discussed in detail in January 2018 in the specialist chapter “Angiology” [6]. It is a fact that currently applications to Swiss health insurance companies for reimbursement of liposuction treatment, even in patients with a specialist diagnosis of lipedema (e.g. by an angiologist or dermatologist) and insufficiently effective conservative treatment measures in the course of treatment, are only assessed positively in rare individual cases. The rejection of coverage for liposuction is very often justified in a standardized manner by the lack of proof of the 3 criteria: Effectiveness, expediency and economic efficiency (WZW criteria) according to Art. 32 KVG.
It is interesting to note the overall very different assessment of the reimbursement situation by policymakers and the health care system. The patient is the one who suffers.
Literature:
- DIMDI (German Institute for Medical Documentation and Information): ICD-10-GM Version 2019. www.dimdi.de/static/de/klassifikationen/icd/icd-10-gm/kode-suche/htmlgm2019/
- AWMF (Association of the Scientific Medical Societies): Guidelines: Lipedema. Registration number 037-012, www.awmf.org/leitlinien/detail/ll/037-012.html
- G-BA (Federal Joint Committee): Decision. Trial guideline: liposuction for lipedema. Decision date: 18.01.2018. www.g-ba.de/beschluesse/3202/
- NR (National Council): Petition Association Lipedema Switzerland. Adjustment of the benefits catalog of the compulsory basic insurance for lipedema. Social Security and Medicare Commission Report, November 15, 2018. www.parlament.ch/centers/kb/Documents/2017/Kommissionsbericht_SGK-N_17.2010_2018-11-15.pdf
- NR (National Council): Petition Lipedema Association Switzerland. Adjustment of the catalog of benefits of the compulsory basic insurance for lipedema. Rejection, 14.12.2018. www.parlament.ch/de/ratsbetrieb/amtliches-bulletin/amtliches-bulletin-die-verhandlungen?SubjectId=45074
- SGV (Swiss Society of Medical Officers and Insurance Physicians): Manual Angiology – Lipedema; January 2018 www.vertrauensaerzte.ch/manual/4/angiologie/lipoedem/
- Hirslanden Klink St. Anna AG, Lipedema Center Central Switzerland, Meggen
DERMATOLOGIE PRAXIS 2019; 29(2): 39-40











