A comprehensive overview of the physiological changes of the skin in old age and associated typical clinical pictures, as well as on the influence of nutrition and environmental factors on the visual aging process and the risk of skin cancer development.
The aging processes of the skin are physiological, according to Prof. Brand. All natural functions of the skin such as secretion, pigmentation, regulation of immunological processes etc. are affected, in some cases they decrease by 50-60%. This results in fibrosis and atrophy of the skin, a decrease in hair and nail growth, a decrease in vitamin D synthesis, and a decrease in the density of Langerhans cells and thus decreased immune response [1].
Intrinsic aging, caused by internal factors and accelerated by dialysis, diabetes or hormone deprivation during menopause, genetics, as well as extrinsic aging are considered to be the cause of the above-mentioned processes. The latter is influenced by external factors, such as ultra-violet radiation, cigarette consumption or air pollution.
Frequent is frequent
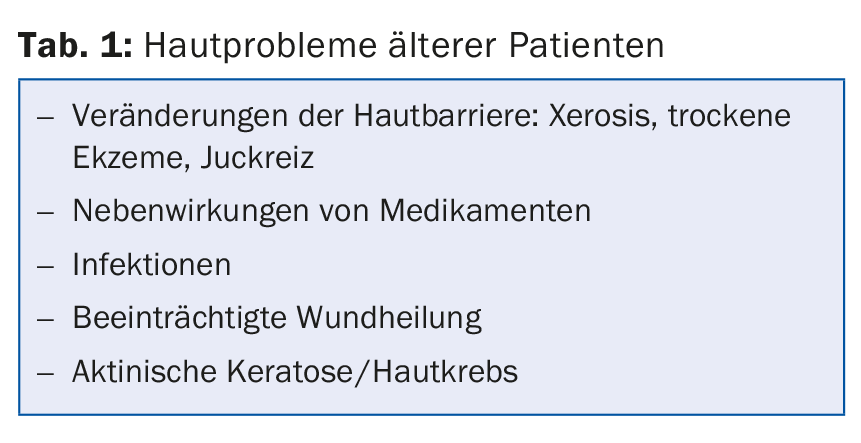
As a result of the described changes in older skin, some dermatological diseases are diagnosed more frequently in this stage of life (Tab. 1).
The altered skin barrier and decrease in seborrheic glands increases the risk of developing dry eczema. This becomes symptomatic mainly by itching and the typical grain of the skin. It is recommended to refrain from excessive washing or to use a pH-neutral soap as well as moisturizing care products. If more severe, topical steroids may be resorted to for a short period of time.
The most common affecting the lower extremities is static dermatitis. It develops due to chronic venous congestion. The result is redness and later eczema. In the case of unusually long-lasting complaints in this area, resistance to therapy, enlargement of the affected area, blistering/weeping in the area of the ulcer and especially in female patients, contact allergy should always be considered as a differential diagnosis, emphasized the speaker.
An exceedingly common phenomenon in dermatology is itching. Again, elderly patients are particularly affected. Depending on the study, prevalence data vary between 11.5 and 41%. This fact can be attributed to three physiological changes in the aging process [2]:
- Decreased epidermal barrier and repair
- natural decrease of immunological response with age
- central and peripheral neurodegenerative disorder
Senile pruritus, however, remains a diagnosis of exclusion. Prof. Brand referred to the clarification of the symptoms prior to this diagnosis with the help of the S2k guideline for the diagnosis and treatment of chronic pruritus [3].
Special features of the medication plan
In addition to local processes in the skin, the metabolism of drugs can change. Polypharmacotherapies and altered pharmacodynamics, as well as pharmacokinetics (with reduced absorption rapidity, decreased renal and hepatic function, etc.) can lead to severe adverse side effects, even at doses at which this would not be expected in the younger patient. 80% of adverse drug reactions (ADRs) that occur in the hospital or lead to hospital admission are dose-related and predictable [4]. In the case of ADRs, it is important to find out precisely whether the patient is taking over-the-counter and/or herbal remedies in addition to the prescribed pharmaceuticals – information that is usually difficult to obtain without asking.
When prescribing new medications or changing the medication schedule, it is important to consider whether the elderly patient is able to take the intended therapy as needed. Psychosocial barriers, comorbidities, compliance, and access to care should be considered. The goal should be to reduce to essential drugs while excluding the “high-risk” class. A regular review of the current therapy plan is also part of the optimal therapy setting.
Wound healing
Wound healing in healthy elderly patients may be delayed. An age of more than 60 years is an independent risk factor [5]. Circumstances that may influence wound healing include immobilization, comorbidities such as diabetes, pAVK, malnutrition, decrease in sex hormones. Factors, in other words, that often affect older people.
Light damage
Photodamage with age is common. It is difficult to assess if and when the early stage of actinic keratosis transitions to squamous cell carcinoma. The literature data here vary between 0.075 and approx. 16%. So treatment is usually indicated, the speaker said.
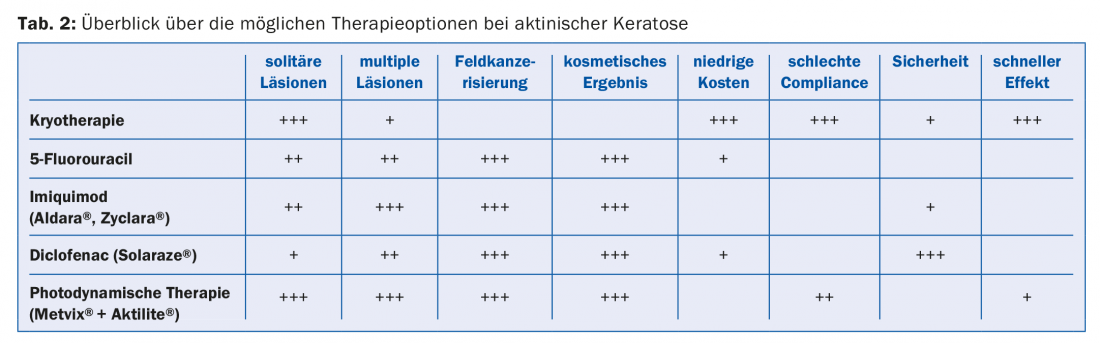
In hyperkeratotic lesions, keratoslysis should be performed. If the foci appear heavily infiltrated, a biopsy should be performed to differentiate between spinalioma and actinic keratosis. Therapy (see Table 2 for actinic keratosis) should be adjusted according to current guidelines.
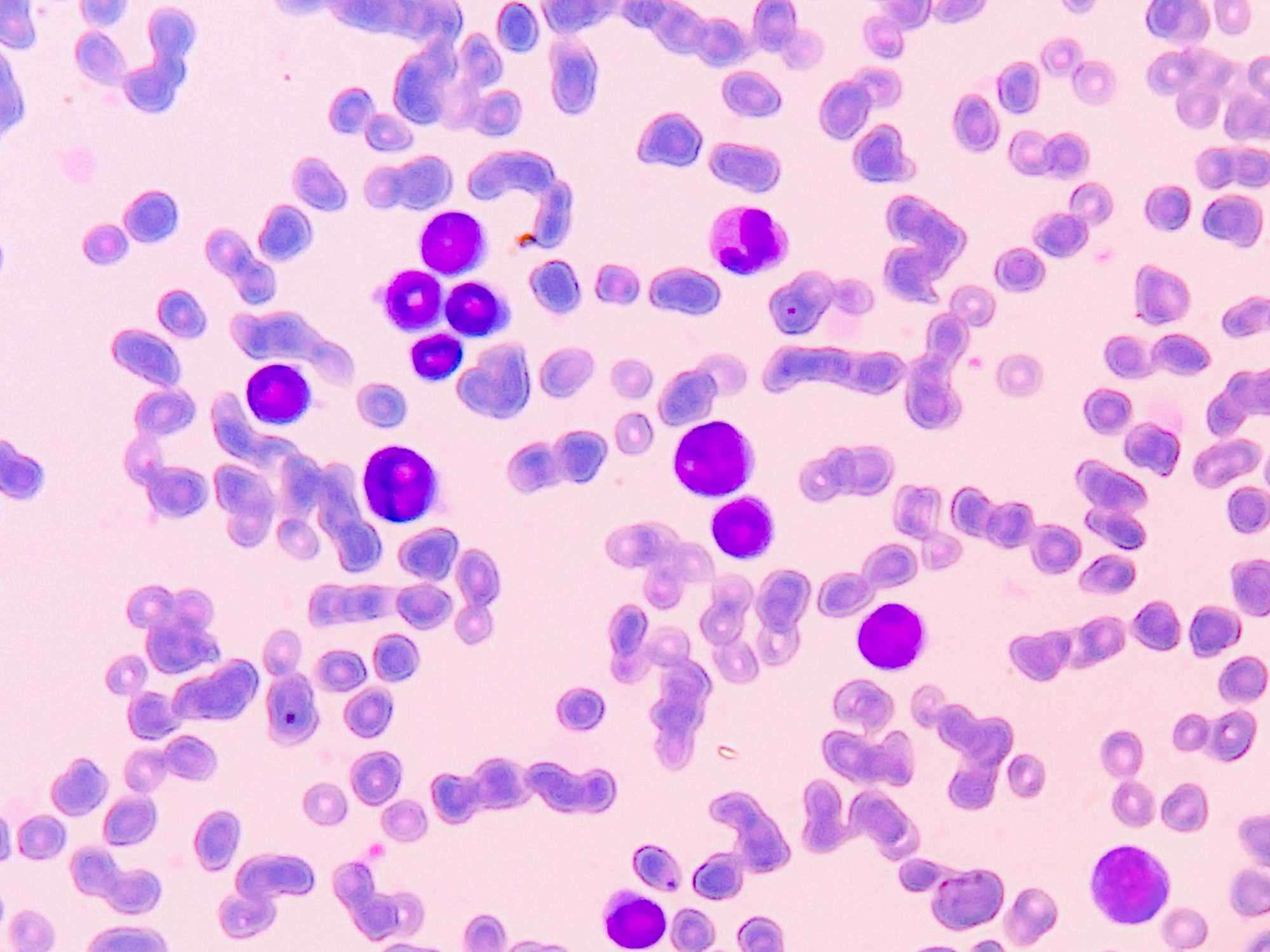
Skin cancer
The age-specific incidence of melanoma increases with age. The situation is similar for balsal cell carcinoma and spinalioma. Advanced age should not be an obstacle to therapy. In the further course, these diseases can otherwise lead to costly care problems, among other things. If the lesions are difficult to operate on, radiotherapy or possibly cryotherapy is a possible alternative.
Infections
Due to the reduced barrier function of the skin, infections occur more frequently in old age. The classic example of bacterial inflammation is erysipelas. Due to a redistribution of fat towards a trunk accentuation, there is also an increased risk of infections in the intertriginous area, here mainly by Candida. Therapeutically, in this case, it takes a paste, not a cream, to dry out the area, Prof. Brand emphasizes.
In addition to infections of the skin, fungal infestation of the nails may increase with age . Depending on the individual situation, a decision should be made here as to whether treatment makes sense and exactly what means can be used to implement it.
Especially in the ophthalmologic field, herpes zoster (with its postherpetic neuralgias) is a major problem in the elderly patient. Meanwhile, a vaccination specifically for zoster is available. There are recommendations to vaccinate from the age of 60 years or from 50 years for patients at risk.
As young as you feel?
The aging processes of the skin are physiological. Nevertheless, the question remains whether it is possible to visibly influence the external appearance of the largest human organ from the outside. In addition to personal preferences, there are countless opinions on the best course of action depending on the desired goal, for example, in terms of a goal-oriented diet.
In 2008, a study showed a benefit from increased intake of vitamin C and linoleic acid, as well as lower consumption of fats and carbohydrates for improved appearance of aging skin [6]. Environmental factors can also be influenced. For men, cigarette consumption, sunlight exposure, and a low BMI have a negative effect on visual facial aging; for women, a low BMI and a low social status also show a significantly unfavorable effect. A positive association with a younger look had a low depression scale score and married people [7].
In addition to the influence of environmental factors on optical aging, their effect on the development of malignancies was also investigated. Thus, an association between nicotine use and the development of spinalioma was found, and the relative risk was 2.3 (p=0.0001) [8]. Coffee consumption led to a reduction in melanoma risk in a meta-analysis. This showed a dose-dependent effect – an increase in coffee consumption of one cup per day was associated with a three percent decrease in melanoma risk [9].
Source: Swiss Derma Day and STI reviews and updates, 10. and January 11, 2018, Lucerne
Literature:
- Cerimele D, Celleno L, Serri F: Physiological changes in aging skin. Br J Dermatol 1990; 122(5): 13-20.
- Wang, K.CH: Pruritus in Older Patients. Advances in Geriatric Dermatology 2015; 31-39.
- Sonja Ständer, et al: S2k-Leitlinie 013/048: Diagnostik und Therapie des chronischen Pruritus, Stand 31.05.2016. (www.awmf.org/leitlinien/detail/ll/013-048.html).
- Brahma DK, et al: Adverse drug reactions in the elderly. J Pharmacol Pharmacother 2013; 4(2): 91-94.
- Sgonc R, Gruber J: Age-related aspects of cutaneous wound healing: a mini-review. Gerontology. 2013; 59(2): 159-164.
- Cosgrove MC, et al: Dietary nutrient intakes and skin-aging appearance among middle-aged American women. Am J Clin Nutr 2007; 86(4): 1225-1231.
- Rexbye H, et al: Influence of environmental factors on facial aging. Ageing 2006; 35(2): 110-115.
- De Hertog SA, et al: Relation between smoking and skin cancer. J Clin Oncol 2001; 19(1): 231-238.
- Micek A, et al: Caffeinated and decaffeinated coffee consumption and melanoma risk: a dose-response meta-analysis of prospective cohort studies. Int J Food Sci Nutr 2017 Sep 11: 1-10.
HAUSARZT PRAXIS 2018; 13(2): 31-33
DERMATOLOGIE PRAXIS 2018; 28(1): 41-43