If a dural AV fistula is demonstrated, it is important to exclude possible involvement of venous drainage of the cerebral parenchyma, spinal cord, and orbit. This is usually accomplished with the MRI scan, which should include MR angiography. In some cases, however, catheter angiographic examination for clarification cannot be avoided.
Case report: A 47-year-old male patient presented with unilateral protrusio bulbi and conjunctival injection to a foreign clinic, where a diagnosis of carotid sinus cavernosus fistula (CCF) was made by MRI (images not available). An ophthalmologic consultation had been regular, an increased eye pressure had not existed.
The patient was recommended a conservative approach with regular ophthalmologic check-ups. He was told that most CCF would spontaneously close.
Six months after initial diagnosis, there had been improvement in protrusio bulbi. However, another three months later, increased eye pressure was detected. The ophthalmologist therefore advised therapy. At this time, the patient presented to our clinic.
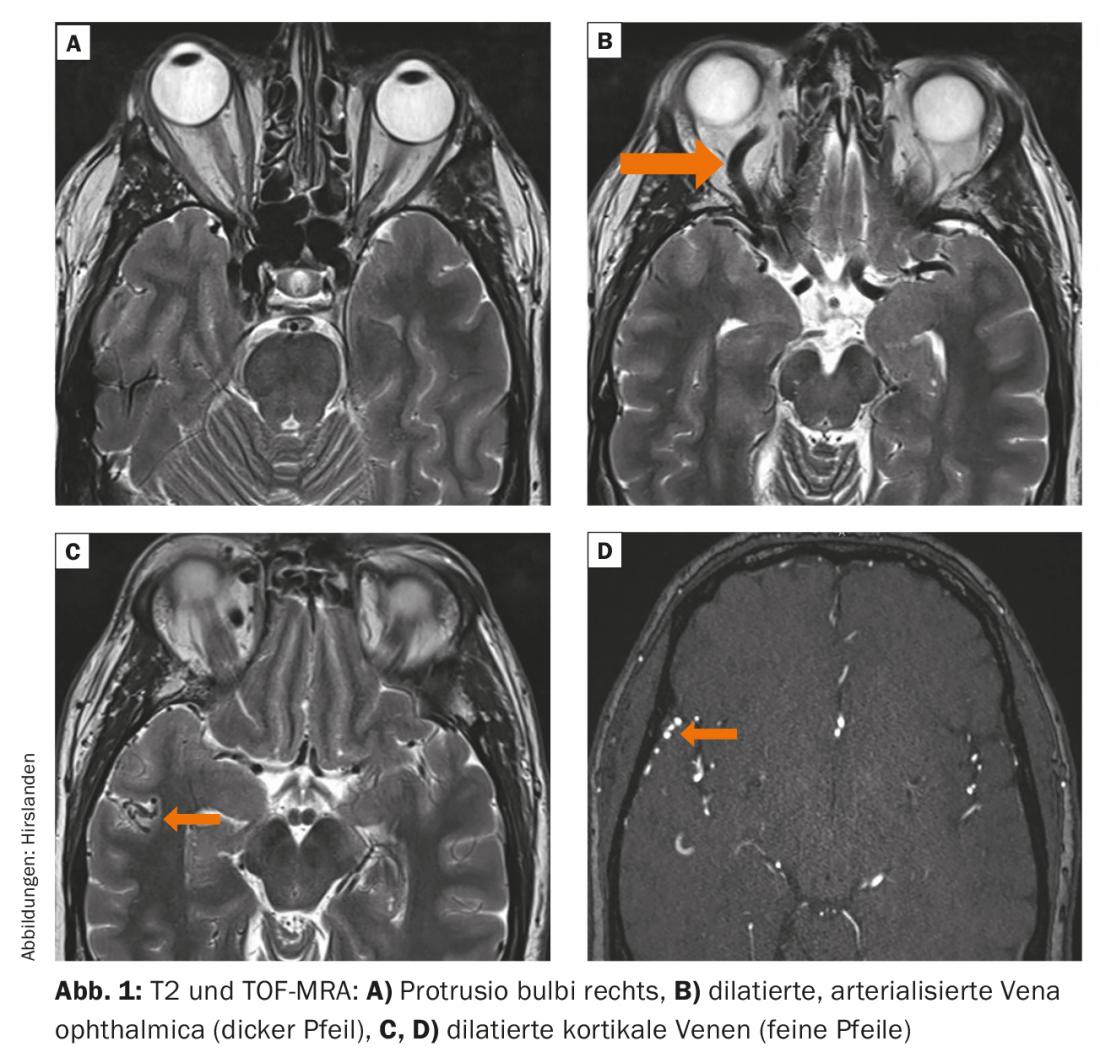
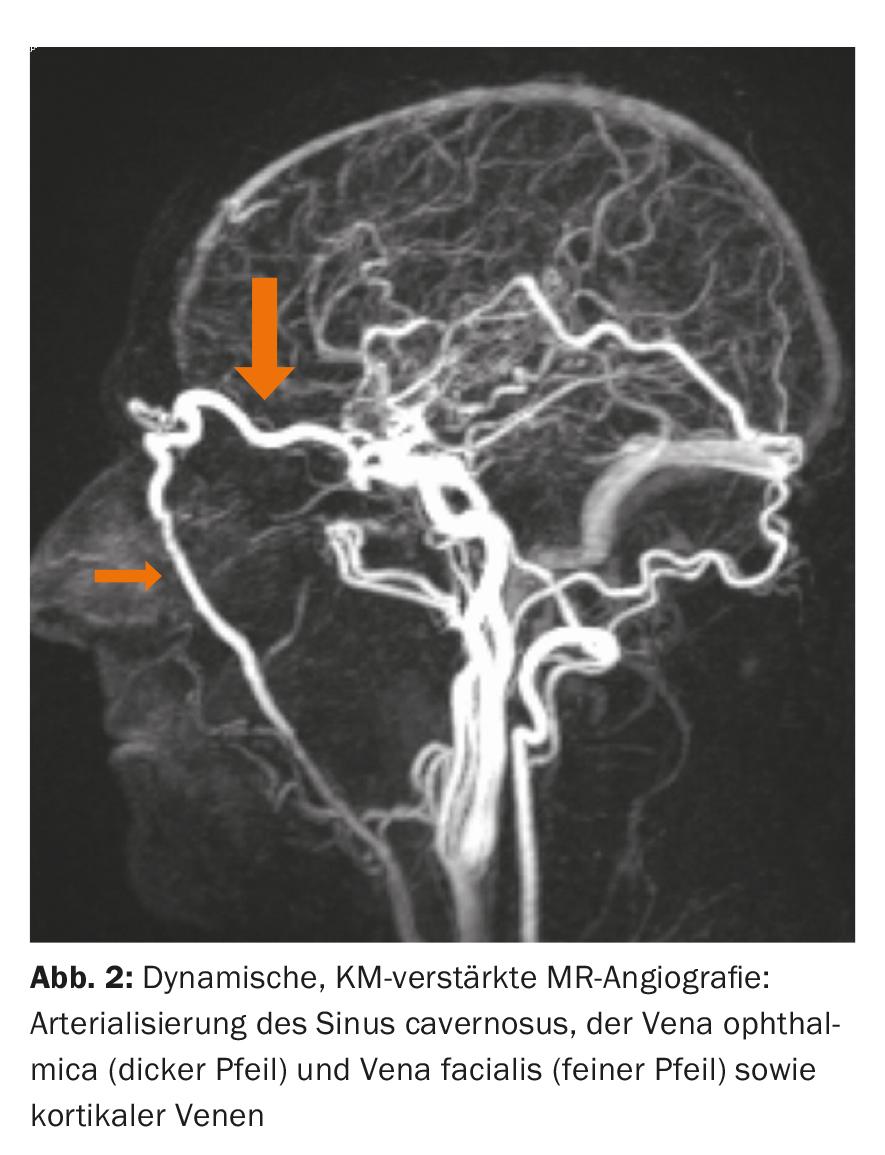
Diagnosis and Therapy: MRI examination demonstrated an AV fistula at the dorsal venous plexus of the clivus. Venous drainage was via the cavernous sinus and further into the ophthalmic vein as well as retrograde via the laterocavernous sinus into intracranial veins. There was exophthalmos, double vision was not complained.
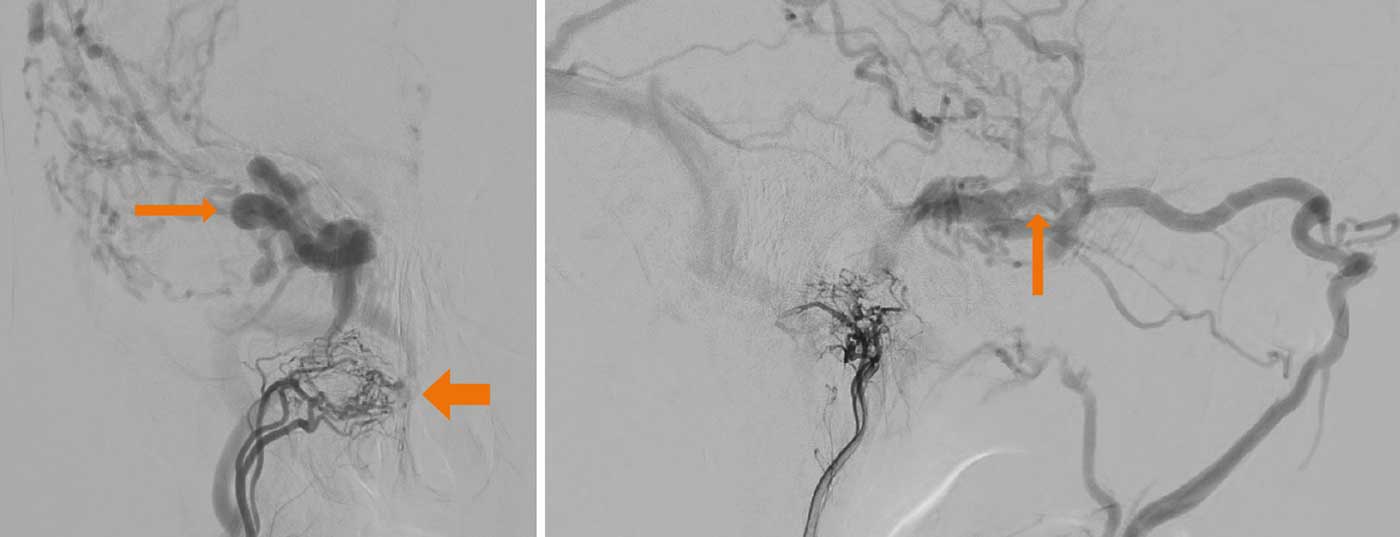
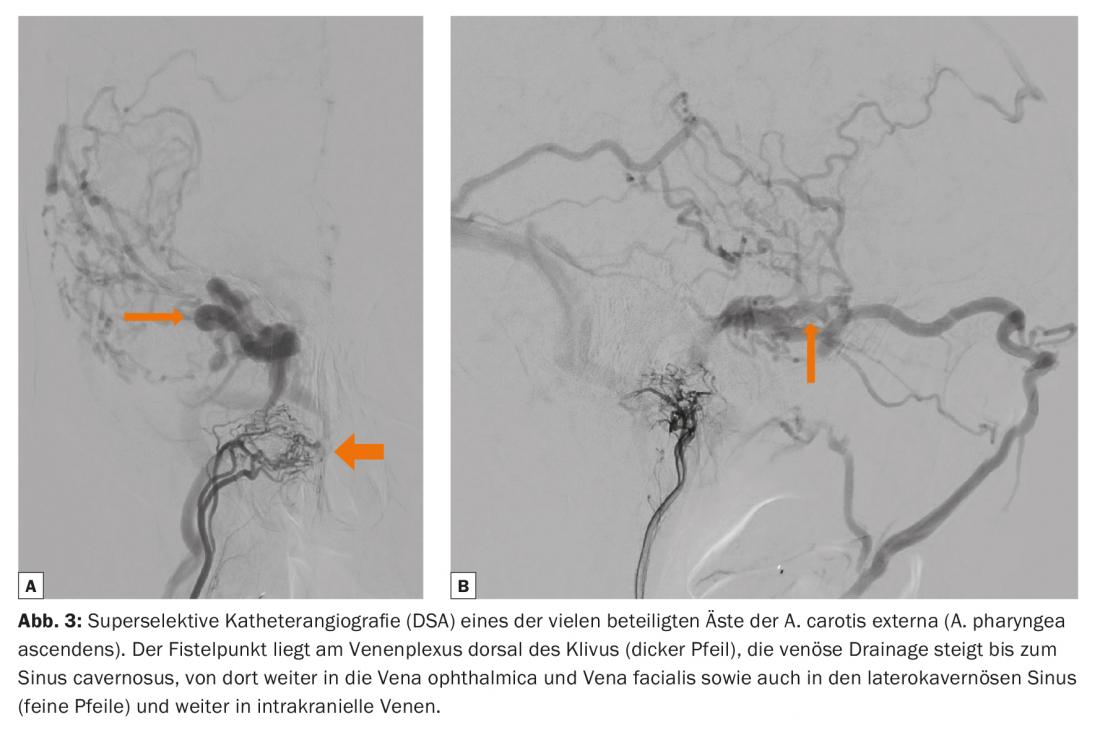
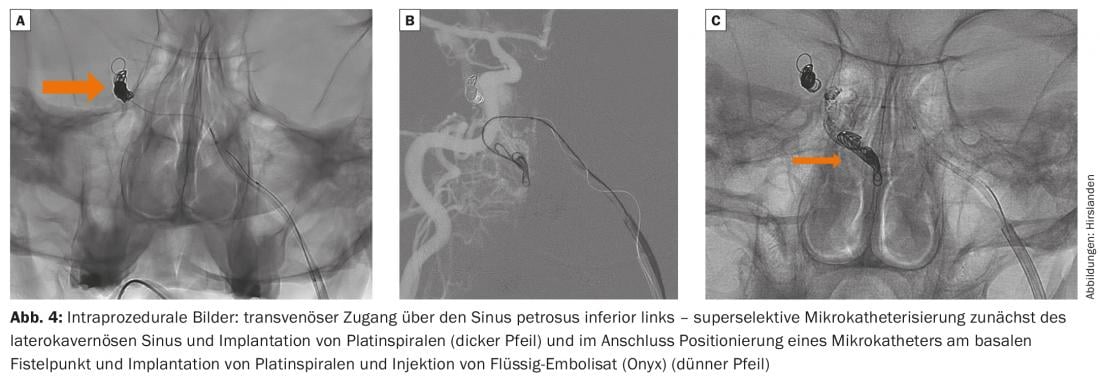
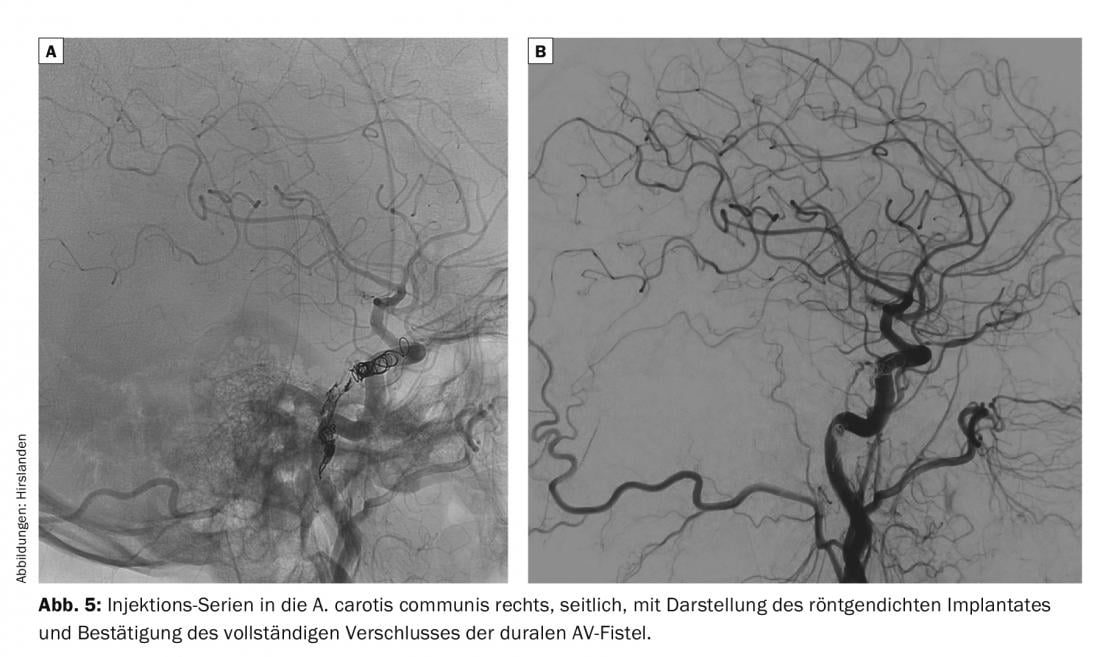
Catheter angiographic workup and endovascular transvenous closure of the AV fistula were performed. Here, under general anesthesia and via femoral punctures, access via the inferior petrosal sinus on the left was chosen to reach the lateralocavernous sinus on the right via the intercavernosal sinus and to fill it with platinum coils to first stop drainage toward the intracranial veins. Another microcatheter via the same access route allowed retrograde probing of the venous plexus along the clivus and access to the fistula zone. This was closed after insertion of platinum coils with liquid embolizate (Onyx).
The protrusio bulbi rapidly regressed. Three months after therapy, the MRI scan shows regular findings with complete closure of the AV fistula with no evidence of recurrence. Vein caliber and eye pressure have normalized.
Background: Dural AV fistulas are now considered to be the result of pathological neovascularization of a venous thrombus and arise on venous segments that have an arterialized wall, accordingly along the dura. Thrombosis may well occur in association with trauma. The patient described was a rugby player, so a traumatic genesis of this unusually localized AV fistula would be entirely possible. However, especially if the cause is unclear, a coagulation analysis should be performed with the question of thrombophilia.
Spontaneous closure of dural AV fistulas has been described in the literature but is very rare. In these cases, the fistula volume is usually small and additional factors, such as manual pressure on the ocular bulb with flow slowing in the ophthalmic vein, trigger occlusion. The interim improvement of protrusio in our patient could be explained by the fact that venous drainage has changed. Initially, venous outflow probably occurred only via the cavernous sinus into the ophthalmic vein. It is reasonable to assume that laterocavernous sinus involvement reduced flow through the orbit because intracranial veins were now also involved in outflow – thus, clinical improvement does not automatically speak for a reduction in AV fistula. In any case, it means that imaging should be done to make sure that the fistula has not turned into a fistula with drainage into cortical veins, potentially causing brain damage from increased venous pressure or even intracranial hemorrhage. There is a risk of hemorrhage whenever cortical veins are involved in drainage, even more so if they are dilated.
Conclusion: If a dural AV fistula is detected, it is important to exclude a possible involvement of the venous drainage of the cerebral parenchyma, the spinal cord and the orbit, respectively. to prove. This is usually accomplished with the MRI scan, which should include MR angiography. In some cases, however, catheter angiographic examination for clarification cannot be avoided.
Therapy is indicated if symptoms exist or the drainage pathway involves cortical intracranial veins or involves venous drainage of the orbit. Endovascular therapy usually allows complete closure of the AV shunt and is therefore the treatment option of first choice.
Further reading:
- Wanke I, Rüfenacht D: The Dural AV Fistula (DAVF), the Most Frequent Acquired Vascular Malformation of the Central Nervous System (CNS). Clin Neuroradiol 2015 Oct; 25 Suppl 2: 325-32.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(3): 35-37.