To diagnose diabetes, there are several methods with certain advantages and disadvantages. Given that today one in two adults with diabetes remains undiagnosed, screening is strongly recommended for individuals 40 years of age and older. One criterion for the screening method in practice is ease of use. In one of his presentations at the Diabetes Update in Zurich, Prof. Roger Lehmann compared the different methods and showed which statements are possible with them. HbA1c is now also newly approved for diagnostics.
HbA1c refers to glycosylated hemoglobin. The proportion of HbA1c in total hemoglobin provides information about the average blood glucose level over the last twelve weeks. With an average lifetime of erythrocytes (and thus their hemoglobin) of about 100 days, the normal HbA1c value is less than 5.5% of total hemoglobin. “The measurement of HbA1c is extremely meaningful, not only for monitoring progress, but also for the diagnosis of diabetes,” said Prof. Roger Lehmann, senior physician at the Department of Endocrinology, Diabetology and Clinical Nutrition at the University Hospital Zurich and one of the keynote speakers at Diabetes Update. Also, the blood glucose criteria for diagnosis are simpler for HbA1c than for plasma glucose [1].
Advantages of HbA1c measurements
With the HbA1c the development of diabetes within five years can be predicted as follows: with an HbA1c of 5.5-6%, the chances are 9-25% that a diabetes diagnosis will be made, the HbA is1c 6.0-6.5%, the chances are 25-50%, i.e. they are 20 times higher than for a HbA1c of 5.0% [2]. In one study, the relationship between the occurrence of retinopathy and the HbA1c value was investigated [3]: The result shows a significant increase from a value of 6.5%, where 6.5% corresponds to the threshold for the diagnosis of diabetes. This result further shows that the better the blood glucose control, the lower the risk of secondary diseases for diabetes patients.
Prof. Lehmann also explained how high the influence of the blood glucose control of the last three months on the HbA1c is: In the first month it is 50%, in the second month 25% and in the third and fourth month also 25%. “In this way, an improvement in blood glucose control can also be recorded after just one month, for example, in the event of a change in therapy.” Prof. Lehmann sees a major advantage of HbA1c in the improved mapping of chronic glycemia. Compared with fasting plasma glucose and OGGT, the other advantages are:
- This is a standardized measurement method.
- Biological variability (2%) is lower than fasting plasma glucose (12-15%).
- Better correlation and predication of secondary complications.
- It is preanalytically more stable and independent of time of day or stress.
- It is the main parameter for therapy adjustment.
Certain limitations should be noted, however; HbA1c is not suitable for diagnosis in the following conditions:
- Hemoglobinopathies (HbS, HbC, HbF, HbE),
- increased erythrocyte turnover (hemolytic anemia, blood transfusion, subclinical hemolysis in HIV)
- severe hepatic and renal insufficiency
- Gestational diabetes or diabetes associated with cystic fibrosis
- Interference with iron deficiency results in falsely high HbA1c, intake of high doses.
- Vitamin C and E provides a falsely low value, in general HbA1c is about 0.4% higher in patients over 70 years old.
Conversion to be simplified
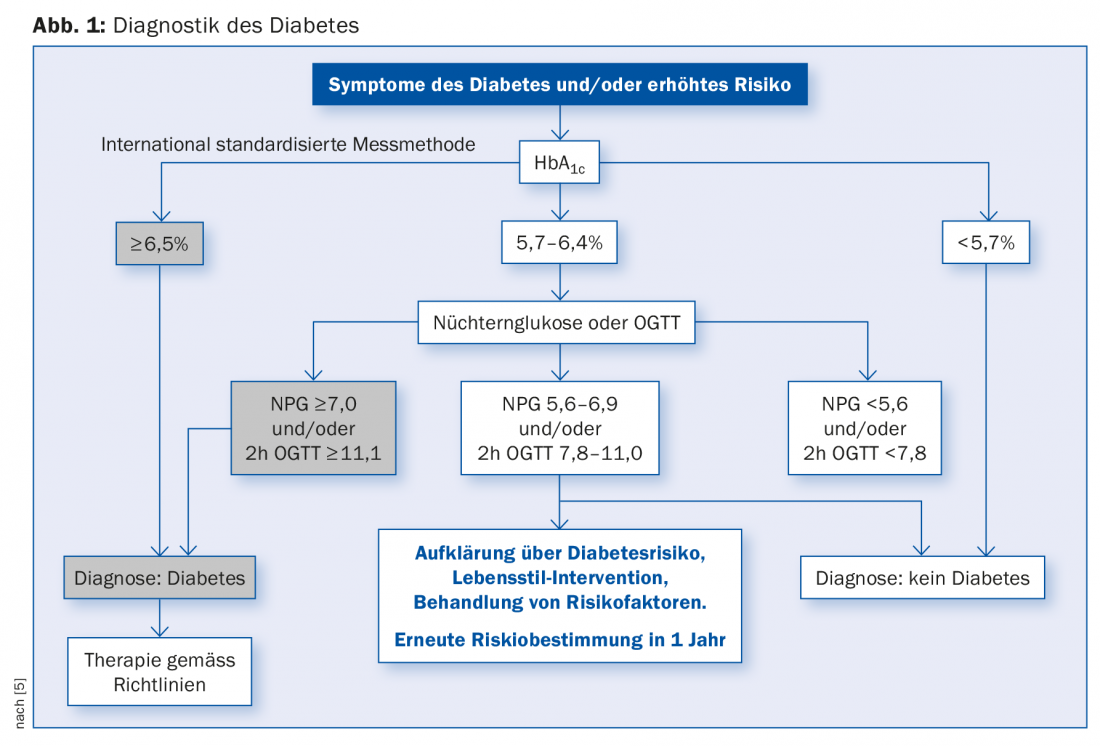
The conversion of HbA1c to average plasma glucose is not linear; moreover, there are two standards: DDCT, which is expressed as a percentage, and the newer IFCC, which is measured in mmol/mol. To obtain the average plasma glucose from HbA1c, calculate as follows: An HbA1c of 6% corresponds to a blood glucose of 7 mmol/l. Per percent HbA1c, add 1.6 mM [4]. This means that an HbA1c of 7.0% corresponds to an average blood glucose of 8.6 mM. Prof. Lehmann points out that in the future these conversions will be simplified to make them easier to understand for physicians and patients. Prof. Lehmann refers here to the scheme of the internationally standardized measurement method [5], see figure 1.
A comparison of tests for prognosis on the cumulative incidence of diabetes over five to six years shows that predictions using HbA1c are similar to those using fasting plasma glucose or the OGTT with 75 g glucose [6]. The Whitehall II study examined the progression of diabetes [7], in 6538 individuals without diabetes aged 35 to 55 years. In the process, 505 cases of diabetes were detected. Measurements of glucose and insulin yielded the following results: NPG increases two years before diabetes diagnosis, postprandial glucose six years before. For insulin secretion, the study showed that it increases four years before diagnosis and decreases two years before diagnosis, while insulin sensitivity decreases more five years before diagnosis.
Source: Forum for Continuing Medical Education, Diabetes Update Refresher, presentation “Diagnosis of Diabetes Mellitus,” November 24, 2016.
Literature:
- Diabetes Care 2011; 34: 11-61
- Diabetes Care 2009; 32, online June 5
- Diabetes Care 2010; 33: 1655-73
- Diabetes Care 2008; 31: 1473-78
- Kerner W: Definition, classification and diagnosis, Diabetology 2010; 5: 109-112.
- ADA Position Statement: Diabetes Care 2003, Suppl. 1, 26: 562-69
- Tobacco Inc, et al: Lancet 2009; 373: 2215-21.
HAUSARZT PRAXIS 2017; 12(1): 38-39











