Early recognition of the onset of psychosis is of great importance, as early help can prevent negative consequences and even chronification of the illness. Centers specializing in early detection play an important role, but primary care providers can also recognize early symptoms, respond to them in a timely and adequate manner, and thus decisively improve the course and prognosis.
Schizophrenic psychoses are often characterized by an insidious and atypical onset. Diagnosis and treatment often occur late in the full onset of symptoms. However, serious consequences already occur in the still pre-psychotic phase and even before that in the still unspecific so-called “prodromal phase”. Early detection and early intervention in the onset of psychosis help to minimize the negative consequences, including pronounced difficulties in the social and educational or occupational spheres, as well as the risk of severe, chronicizing courses of the disease.
Gradual and atypical onset
Schizophrenic psychosis begins, on average, several years before an initial diagnosis is made. In about 70% of later psychosis patients, a gradual development of psychosis can be observed [1]: In the first years, mainly uncharacteristic prodromes or prodromal symptoms occur, i.e., unspecific changes affecting the nature, feelings, behavior, and performance. This can lead to a loss of energy and interest, concentration problems, sleep disturbances and reduced resilience: Patients feel thin-skinned and more sensitive than before, everything gets “under their skin,” they have difficulty concentrating and are quickly distracted. They also have little energy left to go about their daily lives and their interest wanes, even in those things that used to be fun – they’re “just not the same anymore.” Mostly young people are affected by this, who show a behavior that is “somehow different”: Affected people have increasing difficulties in fulfilling their previous role in the family, in partner relationships and at work – the typical “kink in the life line” occurs.
At this stage, the affected person may notice so-called “basic symptoms”, i.e. subjectively experienced impairments in thinking and speaking and changes in perception. Such prodromal signs often become increasingly specific over time. Mistrust arises and unusual interests, ideas and perceptions appear. In addition, there are increasingly interpersonal problems that can lead to social withdrawal (see case study).
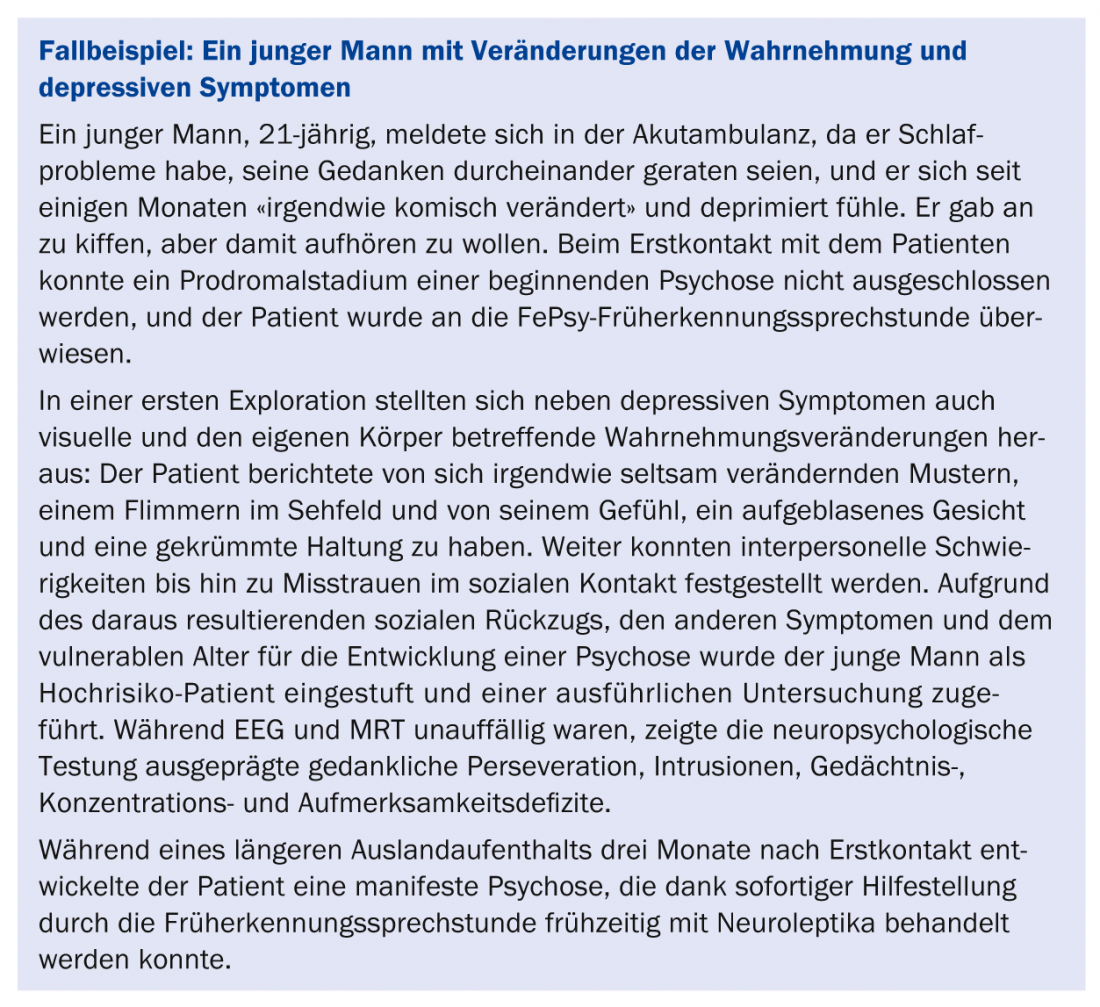
As the disease progresses, the symptoms may become more severe. Subthreshold psychotic symptoms occur, so-called attenuated (pre)psychotic symptoms. Such symptoms are preforms of ego disorders, delusions or hallucinations. Patients feel “like they are in a movie” or their own body feels somehow foreign. Some patients feel watched and followed. Here, however, the delusional conviction is missing, so that the criterion of delusion in the sense of an unalterable conviction is not (yet) fulfilled at this stage. Some patients perceive colors and sounds more intensely or report otherwise strangely altered sensory perceptions. However, the criterion of a hallucination in the sense of a perception without a real basis is not (yet) fulfilled. Isolated brief and transient hallucinations such as hearing one’s own name may occur.
During this “pre-psychotic phase,” transient psychotic symptoms may also occur, so-called brief, transient, intermittent psychotic symptoms. Ego disorders, delusions and hallucinations are here only of short, transient duration (minutes to max. one week with spontaneous remission). If the symptoms intensify even further, the first psychotic decompensation with persistent acute symptoms such as thought disorders, delusions or hallucinations may then occur (Fig. 1) [2].
Consequences of incipient psychosis
Serious consequences can occur even in the still undiagnosed early phase of a psychotic illness. Depressive moods, lack of energy and drive, as well as impaired thinking, attention and concentration often lead to a decline in performance at school, in studies or at work, even in the early stages of psychosis. Characteristic is the often disturbed information reception and processing and an increased irritability. Together with a mistrust due to illness, this leads to a general social withdrawal.
What does early detection do?
Studies have shown that the nonspecific prodromal phase lasts an average of two to five years [3]. Even when psychotic symptoms are already present, it takes an average of one to three years for psychosis to be diagnosed and treated. Early detection allows for timely assessment of psychosis risk status or diagnosis of full-blown psychosis, as well as differential diagnostic evaluation.
Early detection in early detection centers: Early detection centers such as the early detection of psychosis (FePsy) consultation at the University Psychiatric Clinics (UPK) Basel offer comprehensive, individual, outpatient assessment and counseling to people seeking help [4]. It is assessed whether the symptoms reported by the patients may be the first signs of incipient psychosis or even already meet the criteria for psychotic decompensation. This also takes into account whether there is a genetic risk, i.e. whether a close relative of the patient is affected by a psychotic illness.
For clinical interviewing, specially developed clinical diagnostic procedures are used in the FePsy consultation, such as the “Basel Screening Instrument for Psychosis” (BSIP) [5] and the “Basel Interview for Psychosis” (BIP) [6].
By means of further clarifications (thorough psychiatric-psychological examination including neuropsychological testing, EEG, magnetic resonance imaging of the brain, laboratory tests), the risk status of the patient can be assessed more reliably or the diagnosis made can be confirmed and possible causes determined. In addition, these diagnostic procedures can be used to differentially rule out other disorders with similar symptomatology, such as ADHD, depression, or temporal lobe epilepsy. On the basis of the findings resulting from the examinations, an individual therapy plan is drawn up for each patient, and appropriate measures are initiated – if desired, in cooperation with the referring physician.
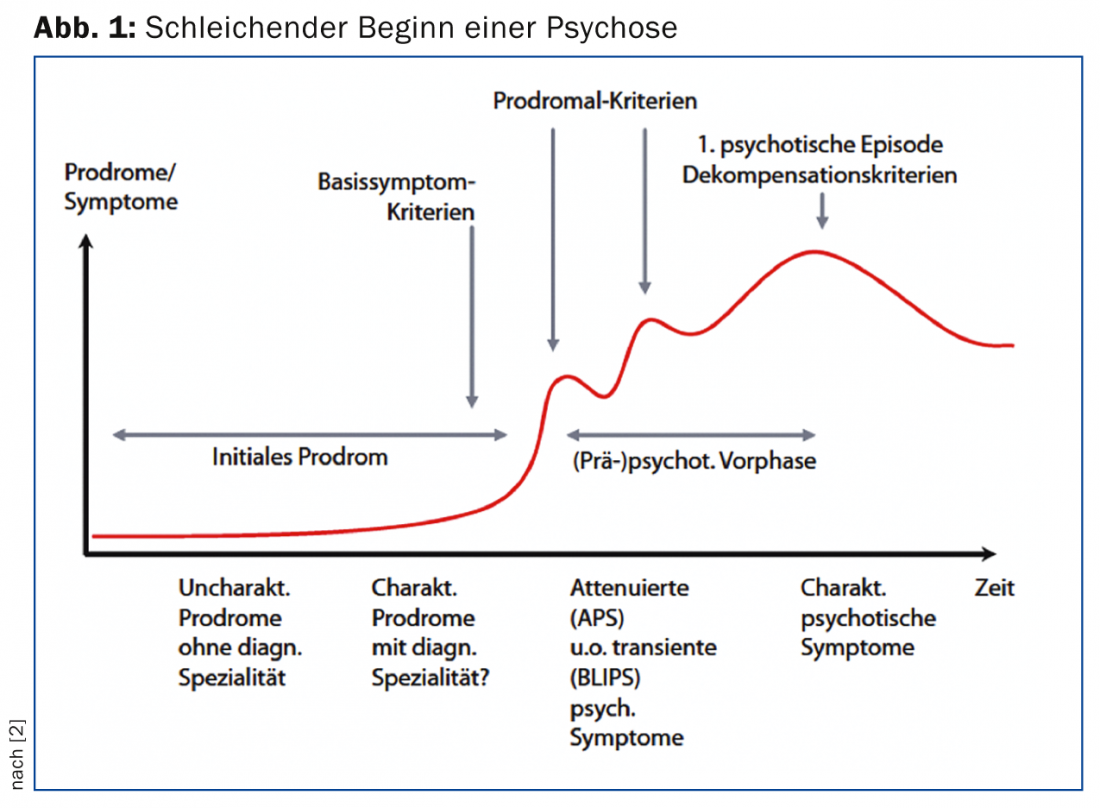
Early detection by the primary care provider: The “Risk checklist for psychosis” was developed specifically for primary care providers as part of the Basel FePsy consultation (Fig. 2) [7].
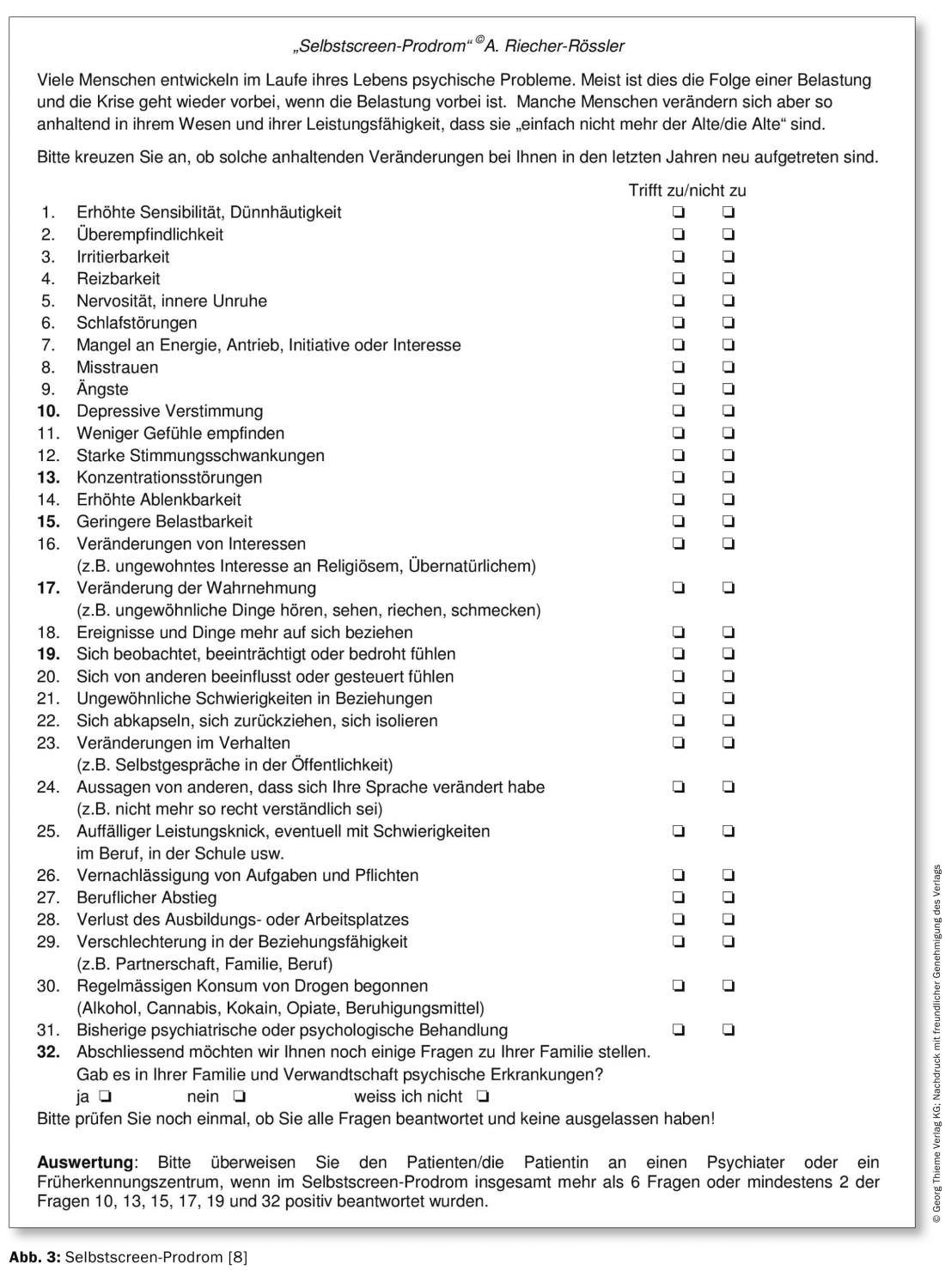
This questionnaire allows a simple and quick assessment in the family practice whether there is a risk of psychosis and a referral to a screening consultation is indicated. There is also a corresponding self-assessment tool, the “self-screen syndrome” (Fig. 3) [8]. These questionnaires help to prevent the symptomatology in adolescents from being mistakenly dismissed as an “adolescent crisis” or – even in adults – from being superficially diagnosed only as depression.
Early Intervention
According to the latest findings, stage-specific treatment is offered as part of early intervention programs. A distinction must be made between the treatment of patients with a first full-blown psychotic episode and interventions for patients at risk in a potential prodromal phase.
Early intervention in high-risk patients: Interventions in people at increased risk for developing psychosis should be very cautious and should not (yet) include antipsychotic medication with neuroleptics [9]. The establishment of a sustainable therapeutic relationship, assistance with acute psychological problems (e.g. measures to reduce stress and support from social workers) and, above all, very good psychoeducation and, if necessary, cognitive-behavioral case management should be in the foreground. Any medication should be symptom-oriented, for example antidepressants for depressive moods or sleep disorders.
Early intervention in first-episode psychotic patients: Early use of neuroleptics is indicated in cases of clearly diagnosed psychotic decompensation. Accompanying supportive discussions, psychoeducation, neuropsychological training programs and, if possible, cognitive behavioral therapy specifically for first-time sufferers should be used. Here, too, a stable therapeutic relationship with the patient and his relatives is of central importance, not least to ensure medication compliance and reduce the risk of relapse.
Conclusions
Schizophrenic psychoses are potentially severe mental illnesses, but they are now relatively manageable if detected early and treated adequately. Under these conditions, many sufferers can return to a “normal” life and fulfill their various social roles. A longer therapeutic accompaniment is of great importance for such a successful re-entry into life.
This article is based on Riecher-Rössler (2014) [10].
Prof. Dr. med. Anita Riecher-Rössler
MSc Fabienne Soguel-dit-Piquard
Literature:
- Klosterkötter J, et al: Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry 2001; 58: 158-164.
- Borgwardt S, et al: Early detection and early treatment of psychosis: preventing serious consequences of illness. INFO Neurology & Psychiatry 2010; 8: 6-10.
- Riecher-Rössler A, et al: Early detection and treatment of schizophrenia: how early? Acta Psychiatr Scand 2006; 113 (Suppl 429): 73-80.
- Riecher-Rössler A, et al: Prediction of psychosis by stepwise multilevel assessment – The Basel Fepsy Project. Fortschr Neurol Psychiatr 2013; 81(5): 265-275.
- Riecher-Rössler A, et al: The Basel Screening Instrument for Psychosis (BSIP): development, structure, reliability and validity. Fortschr Neurol Psychiatr 2008; 76(4): 207-216.
- Riecher-Rössler A, et al: The Basel Interview for Psychosis: structure, reliability and validity. Schizophr Res 2014; 153 (Suppl 1): S128.
- Aston J, Gschwandtner U, Riecher-Rössler A: Screening for early detection of schizophrenic psychosis in family practice. Switzerland Med Forum 2002; 41: 971-974.
- Kammermann J, Stieglietz RD, Riecher-Rössler A: “Self-screen syndrome” – A self-assessment tool for early detection of mental illness and psychosis. Fortschr Neurol Psychiatr 2009; 77: 278-284.
- Fusar-Poli P, et al: The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry 2013; 70(1): 107-120.
- Riecher-Rössler A: Early detection and early intervention in incipient psychosis. NeuroTransmitter [im Druck].
CONCLUSION FOR PRACTICE
- Psychoses often show an insidious onset with non-specific symptoms.
- Serious consequences occur even at early stages.
- Early detection helps prevent psychotic decompensation or chronicity of the disorder.
- Risk checklists help with early detection.
- Early intervention allows people to find their way back to a normal life.
A RETENIR
- Les psychoses présentent souvent un début insidieux avec des symptômes non spécifiques.
- Les conséquences néfastes apparaissent dès la phase initiale.
- Le diagnostic précoce contribue à la prévention d’une décompensation psychotique ou d’une chronicisation de la maladie.
- Les check-lists des risques aident au diagnostic précoce.
- Une intervention précoce permet de retrouver une vie normale.
HAUSARZT PRAXIS 2014; 9(11): 47-52