Chronic wounds are a major challenge for primary care providers. The reasons for this are the diverse causes of wounds, the patient’s desire for rapid treatment success and, last but not least, economic pressure, as treatments are often lengthy. Regardless, it is necessary to provide each patient with a comprehensive assessment and therapy, because only then is there a chance that the chronic wound will ultimately heal.
A wound is a substance defect of the tissue. A wound is said to be chronic if healing has not occurred after three months [1]. Sufferers usually suffer from pain, hardly dare to go out of the house, especially in case of weeping or smelling wounds. The physical constitution and the psyche suffer from this. Before determining a treatment plan, the cause of the wound must be determined, otherwise therapy is given into the blue. The family doctor usually already has a lot of key data.
Diagnostics
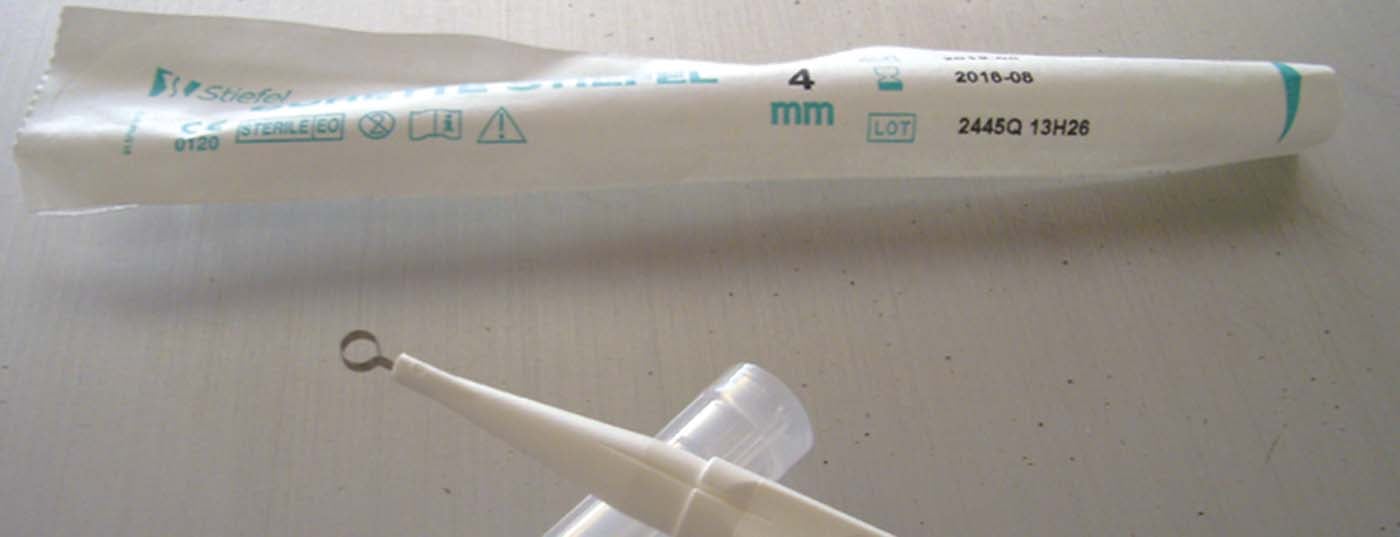
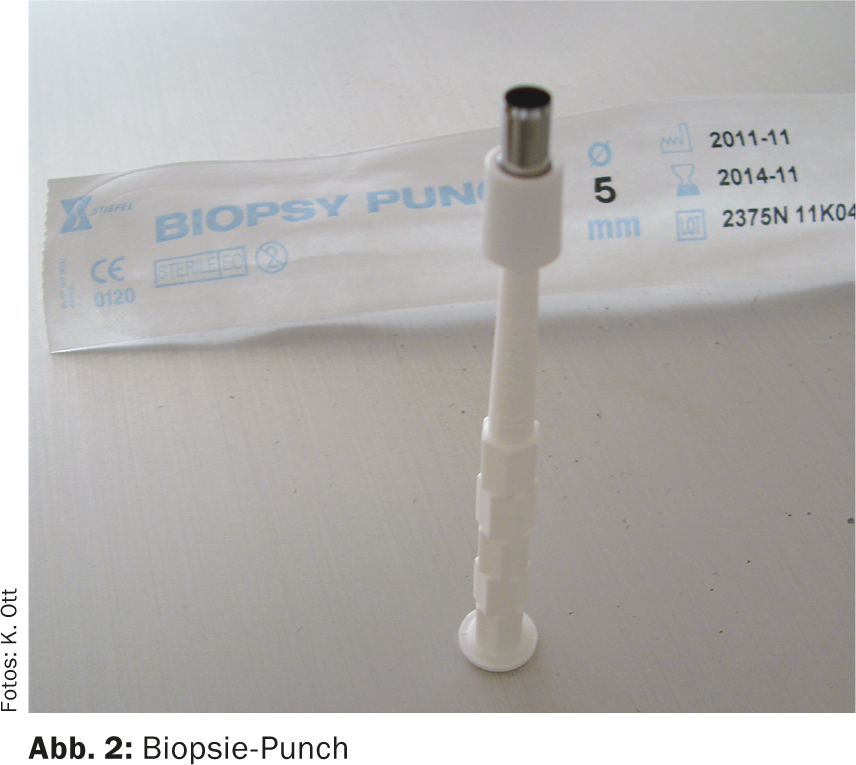
Ulcers often develop on the basis of venous insufficiency, which is already evident on inspection. Duplex sonographic examination further delineates this cause. Other causes are peripheral arterial occlusions (PAVK) (tab. 1). In practice, a perfusion disturbance of the lower extremity can be easily determined by means of the ankle-brachial index. The systolic occlusion pressure at the upper arm and ankle in the region of the anterior and posterior tibial artery is determined with the patient lying down using a hand-held Doppler (Fig. 1). The pressure at the ankle is divided by the pressure of the upper arm. A value of 0.9 or lower already indicates PAVK, even if symptoms are absent. A value of 1.0 is normal. Diabetics may have values greater than 1.3 because of mediasclerosis. For all pathologic values, angiologic evaluation is recommended with regard to potential revascularization [2]. If the process is unclear, a biopsy often leads to a diagnosis. A biopsy punch is suitable for this purpose (Fig. 2); it is advisable to have some hemostatic absorbent cotton (alginate) to hand.
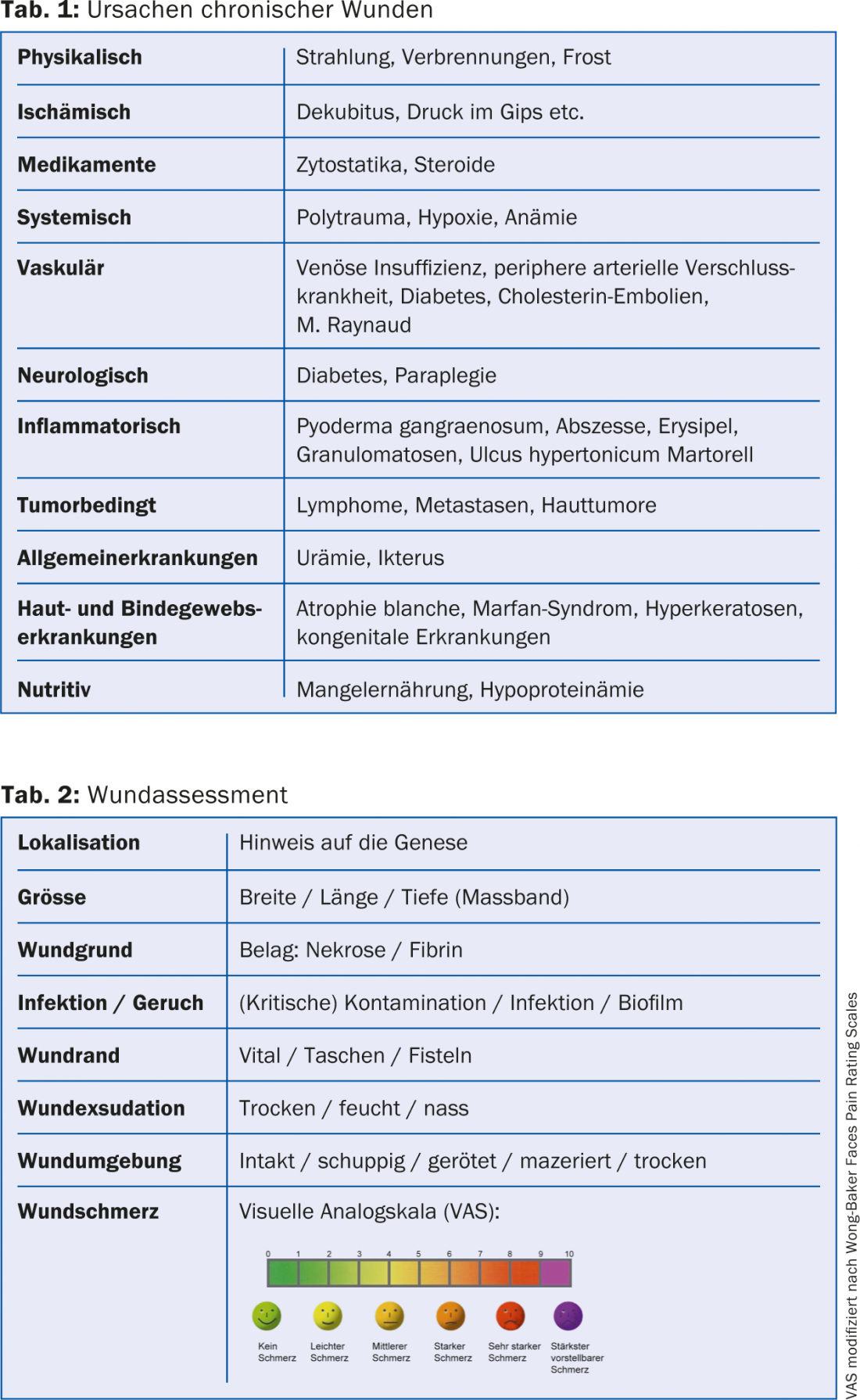
Wound Assessment
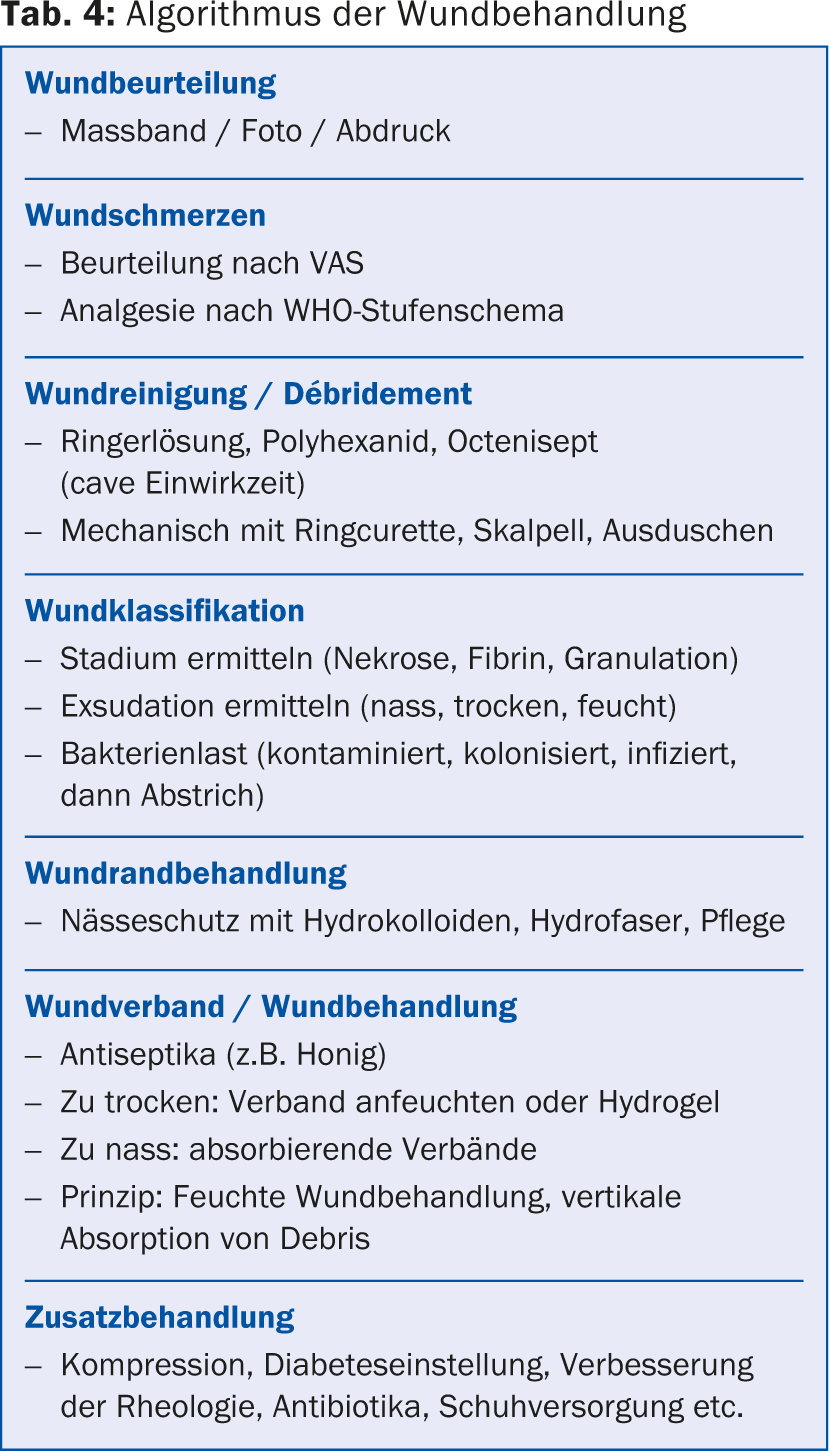
The characterization of the wound determines the local treatment, pain therapy and planning of dressing changes (Tab. 2). Can the patient change the dressing himself, does he need Spitex or is it necessary to call in the patient regularly (Fig. 3)? Economic aspects are just as important as maintaining quality of life and targeted treatment. Initial wound documentation using a digital camera is recommended. The image files can usually be attached to the medical record electronically. They serve the physician to control the course of treatment, but are also increasingly demanded by health insurance companies in order to possibly justify a longer and more cost-intensive therapy.

Wound treatment
So which is the simplest and most efficient dressing? The criteria of hydroactive wound therapy, also called modern wound treatment, should be observed. “Modern” is not very accurate, however, because the ancient Egyptians already knew this treatment principle. In traditional dry wound treatment, the wound is sealed by a scab. This simple principle is very effective, but fails in complex and chronic wounds. Not all possible dressing materials are available in a family practice. It is advisable to have some materials in stock for modern wound therapy. These can be billed via TARMED.
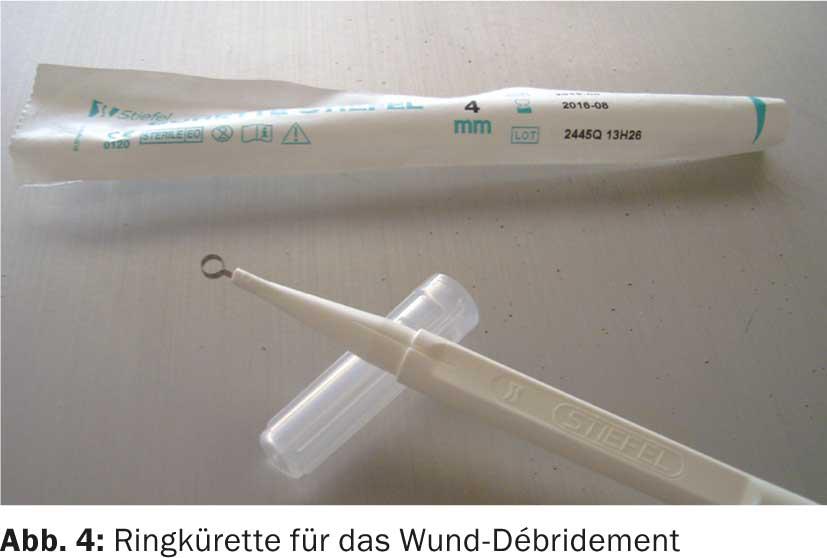
A principle of all wound dressings is vertical absorption. All bacteria and cellular debris are retained in the dressings, and secretions are absorbed. Cotton gauze causes alternation between absorption into the dressing and sloughing off onto the wound and must be changed daily. This is only useful if the patient can perform the dressing changes themselves. If the wounds are too dry, the dressings can be moistened, e.g. with Ringer’s solution or a hydrogel; for wet wounds, the application is dry with appropriate absorbent cover dressings. Advantages of hydroactive dressings are longer intervals between dressing changes, rapid pain reduction and a physiological environment. Local debridement is important beforehand to remove fibrin and necrosis. Debridement can be performed with scissors, scalpel or ring curette (Fig. 4) . With 2% lidocaine gel, usually sufficient analgesia can be achieved within ten minutes.
Also pay attention to the biofilm. These are communities of microorganisms consisting of a mucilaginous matrix of extracellular polymeric substances. These organisms are resistant to external influences and break down again through communication proteins. The biofilm can be “cracked” by means of mechanical debridement in combination with antiseptics.
Antiseptics
Suitable antiseptics include octenidine (Octenisept®), except for fistulas. Polyhexanide (Prontosan®) contains surfactants that break up the biofilm, is hardly toxic and has a low protein defect, but the exposure time is relatively long (ten minutes). However, octenidine and Prontosan® do not have a virucidal effect. Studies indicate that superoxidized water is both antibacterial and breaks up biofilm and is virucidal (Microdacyn®). Betadine® is not suitable for chronic wounds due to toxicity to the wound bed.
Associations
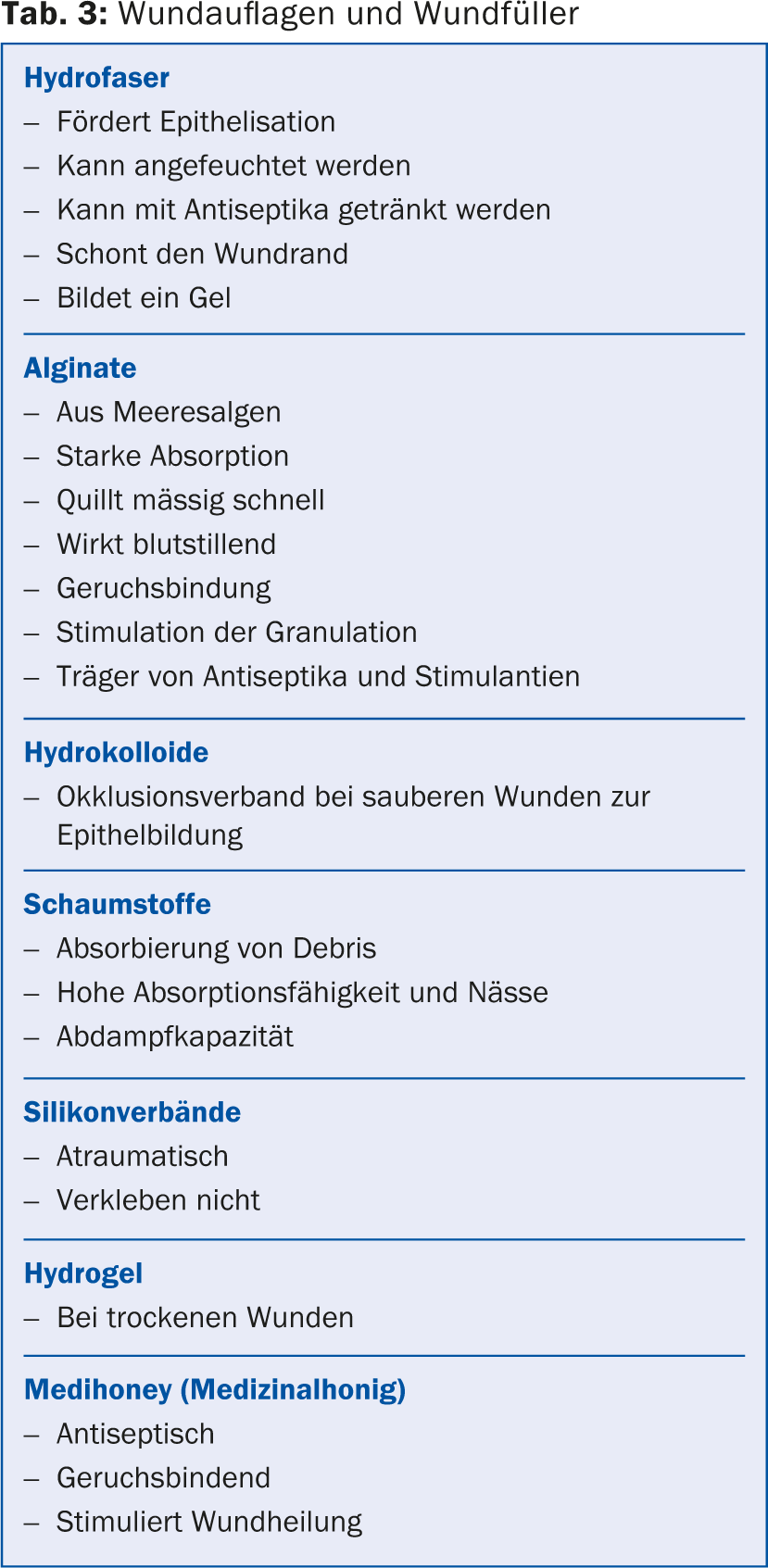
For wound covering resp. wound filling, there are numerous products available, and it is easy to feel overwhelmed by the large range offered by the industry (Tab. 3). The dressing should
- keep the wound moist,
- have a suction capacity appropriate to the degree of exudation,
- be odor-binding,
- stabilize the pH in the acidic range to regulate bacterial colonization and counteract destructive proteases,
- Make room for fibroblasts and macrophages,
- Absorb cell debris.
Adjuvant therapy
Venous insufficiency: Venous insufficiency always requires compression therapy unless PAVK is also present. Compression can be established using short-stretch bandages or appropriate compression stocking systems with washable understocking.
PAVK: In arterial occlusive disease, rheology must be restored, which is usually possible with radiological interventional measures. Otherwise, any local wound therapy is futile.
Diabetes mellitus: The situation is more complex for diabetics. Due to the factors neuropathy, disturbed blood circulation and immune insufficiency, a special dynamic exists. Nevertheless, major amputations are rarely necessary, but the healing time of wounds is much longer. An HbA1c below 7.5% is enormously important for healing. The lack of sensitivity usually results in lesions on the sole of the foot. For prophylaxis, apart from regular inspection of the feet, good shoe care is necessary (shoes with wide toe box and soft bedding). In the case of malum perforans, pressure relief must be provided, e.g. with full-contact plaster, orthosis or VACO®diaped.
Infection: In case of infection, systemic antibiotic therapy is always required after smear collection. The use of local antibiotics is not recommended, as they lead to an imbalance of the prevailing mixed ulcer flora and to resistance.
Malnutrition: Many patients exhibit malnutrition. Without proteins resp. their components, the amino acids, no connective tissue can be regenerated. Vitamin C is important for the stabilization of collagen, especially in the context of revascularization. Since it is not stored in the body and there is an increased need for it, it must be substituted. Zinc is one of the most important trace elements in protein synthesis. Plasma zinc levels should be analyzed prior to treatment. Three times the normal daily intake is recommended for substitution (Table 4) [4].
Literature:
- Streit M, et al: Definiton of wounds: Acute and chronic wounds. ZfW 2008; 3: 159-166.
- Birrer M: The determination of the Ankle Brachial Index: a reliable diagnostic tool for the assessment of cardiovascular risk. Switzerland Med Forum 2007; 7: 254-258.
- McKenna M, Wolfson S, Kuller L: The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis 1991; 87: 119-128.
- Lippert Hans, ed.: Wundatlas: Kompendium der komplexen Wundbehandlung 2006/2: 36.
Further reading:
- Ott K, et al: Wound Manual Luzerner Kantonsspital Wolhusen / Sursee. 3rd revised edition 2011.
- Voggenreiter G, et al: Wundtherapie: Wunden professionell beurteilen und erfolgreich behandeln. Thieme Verlag 2004: 27-34.
HAUSARZT PRAXIS 2014; 9(10): 24-28