At the EULAR congress in Paris, systemic lupus erythematosus was also addressed. Points of discussion were the study situation on antimalarials, the optimized use of glucocorticoids, concomitant measures such as vaccinations and the therapy of specific manifestations.
(ag) According to Jaime Calvo-Alén, MD, Cantabbria, in 2010, a systematic review [1] examined 95 different randomized and observational studies for evidence of antimalarials (AM) such as chloroquine or hydroxychloroquine in systemic lupus erythematosus (SLE). The following conclusions could be drawn: Antimalarial drugs show a
- High level of evidence regarding reduction of mortality, clinical activity, and number of flares
- moderate evidence regarding reduction of organ damage and thrombosis as well as protection against bone mass loss
- little evidence regarding reduction of osteonecrosis or benefit in serum lipid levels.
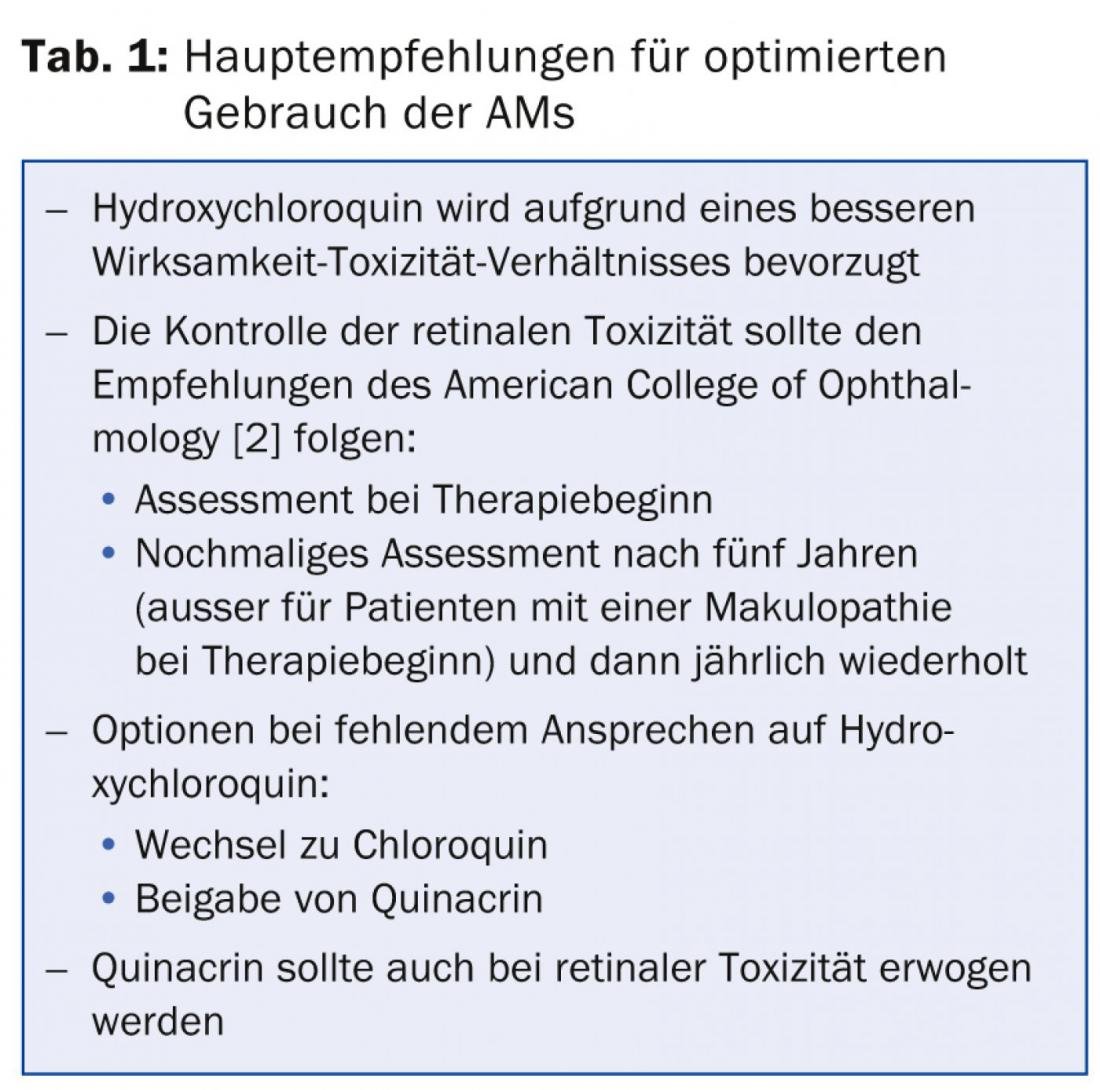
Hydroxychloroquine has a better safety profile than chloroquine, but with both, toxicities are rare, mild, and usually reversible. Hydroxychloroquine, in particular, also appears to be effective during pregnancy without harming the baby. The main recommendations for the optimized use of AMs are summarized in Table 1 .
Sunscreen and glucocorticoids
“Effective sun protection is an important measure, especially for patients with cutaneous involvement. It includes applying sunscreen 30 min before sun exposure and every two hours thereafter. Ideally, the full spectrum of UV-A and UV-B rays should be covered: UV-A rays are more common but less harmful than UV-B rays. A sun protection factor of 50 or higher should be used,” Dr. Calvo-Alén explained. If the ratio between the “sun protection factor” (SPF, as an indicator of UV-B protection) and the so-called “persistent pigment darkening” index (PPD, as an indicator of UV-A protection) is below three, this indicates a good balance between UV-A and UV-B protection. Also helpful are hats, good clothing or tinted windshields.
“Glucocorticoids brought great advances in the treatment of SLE. They are very effective and essential in some manifestations,” the expert said. “My recommendation is to start with the minimum effective dose. In addition, gradual tapering protocols are useful. There are several studies on the efficacy of dose reductions in lupus manifestations [3,4]. Concomitant administration of other agents such as immunosuppressants (methotrexate) or biologics (belimumab) may reduce the need for glucocorticoids. Regarding side effects: Preventive measures in the area of infections should be taken and risk factors for cardiovascular disease should be controlled as much as possible. Moreover, one must try to prevent osteoporotic symptoms with appropriate precautions.”
Accompanying measures
Measures that can be used in conjunction with the above therapies are vaccinations (anti-pneumococcal, HPV, influenza, but not live microorganism vaccinations) and vitamin D assessment (and supplementation if necessary). Low vitamin D levels are associated with cardiovascular risk factors and increased disease activity in SLE patients [5]; furthermore, vitamin D naturally has a positive effect on bone.
Rituximab and calcineurin inhibitors in lupus nephritis.
Head-to-head comparisons of the use of rituximab and calcineurin inhibitors in refractory lupus nephritis do not exist; both appear to be good options in this setting. However, it is certain that calcineurin inhibitors have a direct additional anti-proteinuric effect and a toxic effect on renal function. Possible indications for this therapy are:
- Basal hypogammaglobulinemia
- Refractory lupus nephritis (class V)
- Severe proteinuria.
Rituximab, on the other hand, is considered for patients with renal insufficiency.
In cases of inflammatory involvement of the central nervous system, high-dose glucocorticoids and immunosuppressants such as cyclophosphamide or mycophenolate mofetil are standard [6].
What is the conclusion?
“In summary, AMs remain cornerstones of lupus treatment. Steroid use should be optimized. Vaccination recommendations should be followed urgently. In refractory cutaneous lupus, belimumab should be the first biologic option. After failure of standard therapy, rituximab is the best option in CNS involvement. Preventive measures for cardiovascular disease are part of lupus therapy in any case,” Dr. Calvo-Alén concluded his presentation.
Source: “Systemic lupus erythematosus,” presentation at EULAR Congress, June 11-14, 2014, Paris.
Literature:
- Ruiz-Irastorza G, et al: Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review. Ann Rheum Dis 2010 Jan; 69(1): 20-28.
- Marmor MF, et al: Revised recommendations on screening for chloroquine and hydroxychloroquine retinopathy. Ophthalmology 2011 Feb; 118(2): 415-422.
- Ruiz-Irastorza G, et al: Prednisone in lupus nephritis: how much is enough? Autoimmune Rev 2014 Feb; 13(2): 206-214.
- Houssiau FA, et al: Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 2002 Aug; 46(8) :2121-2131.
- Lertratanakul A, et al: 25-Hydroxyvitamin D and cardiovascular disease in patients with systemic lupus erythematosus: Data from a large international inception cohort. Arthritis Care Res (Hoboken) 2014 Jan 27. doi: 10.1002/acr.22291. [Epub ahead of print].
- Bertsias GK, et al: EULAR recommendations for the management of systemic lupus erythematosus with neuropsychiatric manifestations: report of a task force of the EULAR standing committee for clinical affairs. Ann Rheum Dis 2010 Dec; 69(12): 2074-2082.
DERMATOLOGIE PRAXIS 2014; 24(4): 38-37











