Endovascular therapy for acute ischemic stroke focuses primarily on mechanical removal of thrombi from the affected cerebral vessel (mechanical thrombectomy). Using second-generation techniques (stent retrievers), high recanalization rates can be achieved in short intervention times. Single-arm studies show very good neurological recovery in treated patients. Using these techniques, treatment options for stroke patients have improved significantly, especially in cases of contraindications/persistent occlusion after intravenous thrombolysis or outside the 4.5-hour time window for systemic lysis. The extent to which mechanical thrombectomy replaces or complements systemic thrombolysis for proximal vessel occlusion is currently being investigated in randomized controlled trials.
Acute ischemic stroke is one of the leading causes of morbidity and mortality in industrialized nations. The lifetime risk of stroke is estimated at 1 in 5 for women and 1 in 6 for men. The relevant factors for neurological recovery after stroke are well known: the recanalization rate, the time window between symptom onset and recanalization, and the extent to which hemorrhagic transformation occurs in the affected area after stroke (symptomatic intracranial hemorrhage). Recanalization in particular has a significant impact on patient recovery. The chances of independent life after stroke are 4.4-fold higher after successful reperfusion compared with persistent occlusion. At the same time, mortality decreases significantly after recanalization [1].
Systemic and local therapy approaches
Systemic intravenous thrombolysis significantly improves neurological recovery in patients compared with control groups. Disadvantages are the narrow therapeutic window of 4.5 hours after symptom onset and the moderate recanalization rate, especially in proximal intracranial vessel occlusions (internal carotid artery and cerebri media artery). In addition, any application of fibrinolytics increases the rate of intracranial hemorrhage.
Endovascular therapy of acute ischemic stroke in transition.
Endovascular therapeutic approaches aim to prolong the therapeutic window, reduce fibrinolytics, and achieve high recanalization rates. As early as 1982, initial studies showed that local endovascular administration of fibrinolytics in the affected vessel beyond the 4.5-hour limit can lead to successful recanalization.
The following PROACT II study (“Prolysis in Acute Cerebral Thromboembolism-2”) [2] could thus clearly show an improved outcome of stroke patients with A. cerebri-media occlusions compared to the control group. Intra-arterial thrombolysis continues to be used in almost all stroke centers in the six-hour time window in the anterior circulation and without a clearly defined time window in the posterior circulation. Technically, this procedure is simple: after angiographic visualization of the cerebral vessels via a transfemoral approach and advancement of a catheter into, for example, the A. carotis interna, a small catheter (microcatheter) is advanced into the thrombus, for example in the A. cerebri media (Fig. 1) . There, compared to systemic thrombolysis, a lower dose of the fibrinolytic agent is applied and, if necessary, mechanically manipulated.
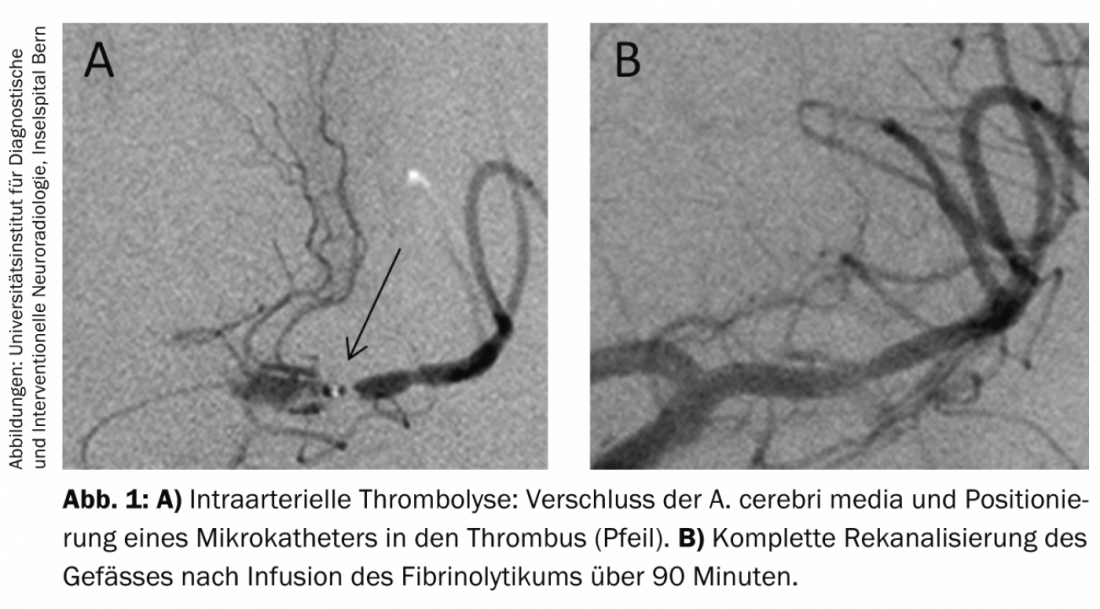
The disadvantage of this procedure is the duration of the intervention: intra-arterial thrombolysis is a relatively time-consuming procedure, lasting approximately 60-90 minutes per vascular segment. Furthermore, despite the lower dose and local application of the drug, there is an increase in symptomatic intracranial hemorrhage from approximately 2% (with natural history) to approximately 10%. At the same time, the procedure is technically simple; complications of the treatment in terms of perforation or dissection are very rarely found.
Since the majority of acute cerebral vessel occlusions are thromboembolic events, further treatment of the cerebral vessel is not necessary after dissolution or removal of the thrombus, e.g., by intra-arterial thrombolysis. Only in very few cases is PTA or stenting of the vessel necessary, as is virtually always performed in myocardial infarction. Only rarely are arteriosclerotic changes such as high-grade intracranial stenosis of the affected vessel found.
Intracranial stenting: Analogous to the treatment of acute myocardial infarction, studies on stenting of intracranial occlusion, for example in the middle cerebral artery, have been performed in the past. Recanalization rates are high at 80-90%, and the intervention duration is short. It proved to be a disadvantage that only rarely the original vessel caliber can be restored, because the thrombus is compressed against the wall. In addition, after stent implantation, there is a need for platelet aggregation inhibition with increased risk of intracranial hemorrhage after stroke [3].
Mechanical thrombectomy
Because of the pathophysiology and the usually mechanical obstruction of an otherwise healthy cerebral vessel, mechanical thrombectomy, i.e., removal of the flow obstruction from the vasculature, is obvious. Comparable to the Fogarty maneuver in peripheral vessels, this procedure could address some disadvantages of intra-arterial thrombolysis: short recanalization times, high recanalization rates, and reduction of intracranial hemorrhage rates by avoiding fibrinolytics. However, due to the anatomical requirements of intracranial vessels with tortuous course and small diameter, clinical implementation proved difficult.
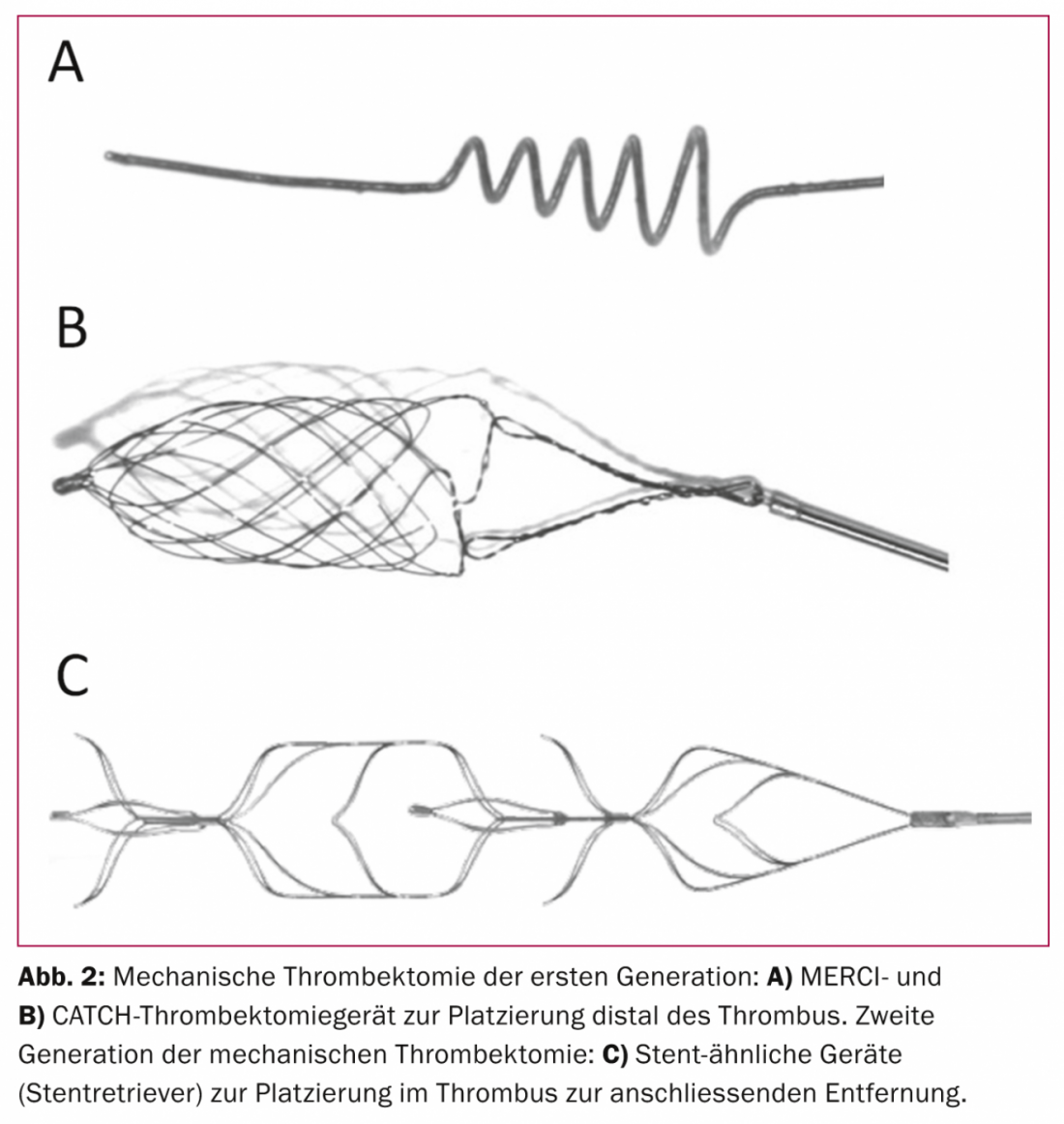
Distal thrombectomy approaches: The first generation of thrombectomy techniques included distal thrombectomy. In this procedure, the thrombus is passed through a microcatheter and a small basket or coil is deployed behind the thrombus. With retraction of this unfolded basket, the thrombus should be removed. This approach has been the subject of many studies over about a decade since 2004. Typical representatives of this thrombectomy were the Merci or the Catch device (Fig. 2) . In fact, recanalization rates proved to be only slightly higher compared with intra-arterial thrombolysis. At the same time, intervention times, complication rates, and clinical recovery of patients in recent studies are significantly inferior to newer approaches using second-generation techniques, and this type of mechanical recanalization is increasingly being abandoned [4,5].
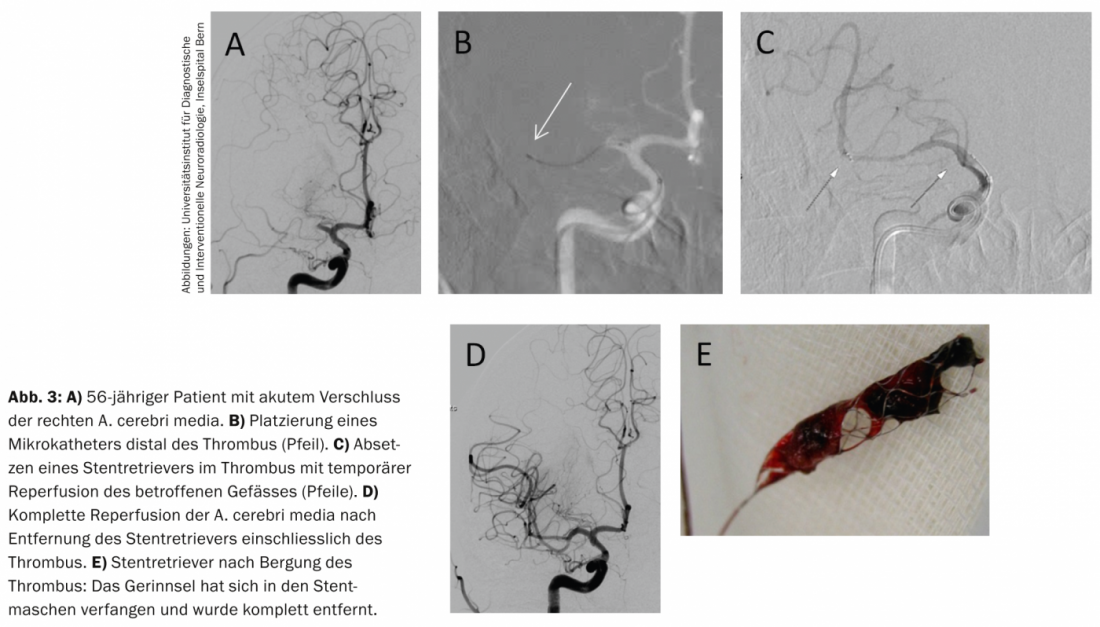
Stent retriever thrombectomy: Since 2009, a more advanced variant of mechanical thrombectomy has been used; this is increasingly gaining international acceptance. Second-generation thrombectomy is a combination of intracranial stenting and thrombectomy. As with distal approaches, a microcatheter is first advanced through the thrombus into the distal vessel segment, and a stent is subsequently placed in the thrombus. In all cases, this “temporary” stent leads to compression of the thrombus and a bypass effect with restoration of intracranial perfusion after weaning. However, the stent is firmly attached to a wire (Fig. 2) . Unlike typical stenting, this device is withdrawn and removed from the cerebral vessels after about five minutes. In most cases, the thrombus gets caught in the stent meshes and can also be completely removed.
Some studies have shown that the relevant parameters of stroke treatment are favorably influenced by this. High recanalization rates in short intervention time with good patient recovery are shown. Because of the avoidance of fibrinolytic drugs, the rate of symptomatic intracranial hemorrhage has been low in studies to date.
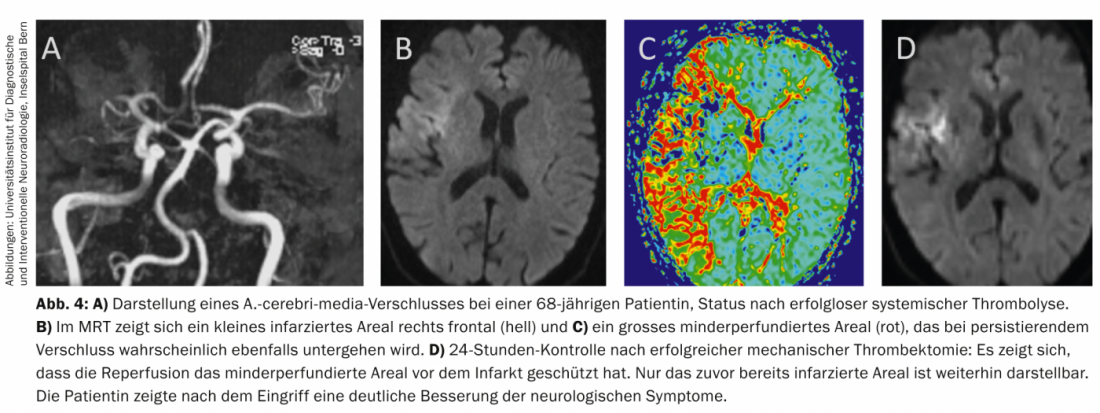
The largest study of second-generation thrombectomy, the STAR trial, was initiated in Switzerland and conducted in Europe, North America, and Australia [6]. This prospective thrombectomy study for the treatment of acute stroke examined 202 patients with vascular occlusions of the anterior circulation (internal carotid artery, cerebri medial artery) in a single-arm design. The mean age was 72 years, and the NIHSS score was 17, equivalent to severe stroke. All patients were treated in the eight-hour time window, some after intravenous thrombolysis had been performed but was unsuccessful. Relevant recanalization (≥TICI2b, “thrombolysis in cerebral infarction” grading) was achieved in 79.2% of cases, and favorable clinical recovery of patients was found in 57.9% (modified rankin scale ≤2). The recanalization time was 29 minutes on average. The study had a patient mortality rate of only 6.9%, and the rate of symptomatic intracranial hemorrhage was low at 1.5% (Figs. 3 and 4).
Current study situation
To date, the study situation regarding endovascular therapy of stroke is confusing and inconsistent. In February 2013, three randomized trials appeared in the New England Journal of Medicine [7–9], which examined the effect of endovascular therapy compared with systemic therapy. None of these studies demonstrated a significant effect of endovascular therapy compared with the control group receiving only systemic intravenous thrombolysis. It is noteworthy, however, that because of the described historical development of endovascular stroke therapy, none of these studies applied second-generation therapy methods to a relevant extent.
Thus, despite the high recanalization rates, the short intervention time, and the good clinical outcome of patients after therapy with stent retrievers in single-arm studies, the efficiency of this procedure remains unproven at the level of randomized-controlled trials. Currently, this aspect is being specifically investigated in several further studies. Of note here is the Swift-Prime trial, which is investigating the treatment of stroke initiated within the first 4.5 hours. Patients with only intravenous thrombolysis and patients with intravenous thrombolysis followed by mechanical recanalization were compared.
Summary
The key to successful stroke therapy is rapid restoration of cerebral blood flow.
Mechanical thrombectomy, especially with second-generation techniques (stent retrievers), has high recanalization rates and short intervention times. This correlates with very good patient recovery in recent single-arm studies.
This technique offers the possibility of recanalization in patients with contraindications to intravenous thrombolysis after unsuccessful thrombolysis and beyond the 4.5-hour time window, significantly improving the patient’s chances of recovery.
The extent to which endovascular therapy with modern approaches complements or replaces established systemic therapy within the 4.5-hour window is still unclear.
Prof. Dr. med. Jan Gralla
Literature:
- Rha JH, Saver JL: The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 2007; 38(3): 967-973.
- del Zoppo GJ, et al: Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Ann Neurol 1992; 32(1): 78-86.
- Levy EI, et al: First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke: SARIS (stent-assisted recanalization in acute ischemic stroke). Stroke 2009; 40: 3552-3556.
- Nogueira RG, et al: Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 2012; 380(9849): 1231-1240.
- Saver JL, et al: Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 2012; 380(9849): 1241-1249.
- Pereira VM, et al: Prospective multi-center single-arm study of mechanical thrombectomy using solitaire FR in acute ischemic stroke (STAR). Stroke 2013; 44: 2802-2807.
- Broderick JP, et al: Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013; 368(10): 893-903.
- Ciccone A, et al: Endovascular treatment for acute ischemic stroke. N Engl J Med 2013; 368(10): 904-913.
- Kidwell CS, et al: A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013; 368(10): 914-923.
CARDIOVASC 2014; 13(4): 9-12