Just over 70% of the Swiss population engage in sports at least occasionally. In addition to general fitness training, this mainly involves endurance sports such as jogging, cycling or swimming. Skiing and hiking are of great importance simply because of the geographical location. In addition to the positive, health-promoting aspects, sport can also lead to accidents and illness. Thus, the skin can also be affected by specific sports-related changes and diseases. Although these are often harmless and easy to treat, they can occasionally present diagnostic difficulties, for which this article is intended to provide an overview.
Great sport begins where it has long since ceased to be healthy (Bertold Brecht).
As a borderline organ, the skin is naturally exposed to exogenous influences, which is why many causes of sports-related skin changes are mechanical or environmental ( Table 1).

In mechanical damage, many changes such as blisters or hyperkeratosis are evident. Hemorrhages at the heel (“black heel”) or subungual, sometimes associated with further nail changes or onycholysis (“runner’s toes”), may occasionally worry the patient and must be differentiated from melanocytic changes. Often, due to the superficial localization in the epidermis, the finding can be scraped tangentially with the scalpel blade and thus differentiated from deeper melanocytic changes (Fig. 1a-c). In addition to jogging, which can also lead to irritative eczema of the nipples (“jogger’s nipple”), it is mainly stop-and-go sports such as tennis or squash that can lead to skin changes on the feet.

In the case of pre-existing skin diseases such as psoriasis or lichen ruber, the isomorphic stimulus effect can lead to the appearance of new skin changes. Finally, fatty tissue hernias, so-called piezogene nodules at the edge of the foot, can occur due to the increased pressure load during running sports (Fig. 2).

Environmental influences
In the case of mountain sports, which are frequently practiced in Switzerland, UV and cold exposure in particular must be taken into account. In addition to the longer-term increased risk of cutaneous neoplasia, UV exposure can also lead to acute changes such as dermatitis solaris or provocation of UV-induced dermatoses if protection is inadequate. Herpes labialis due to UV-induced immunosuppression may occur more frequently.
Frostbite may be observed in addition to diseases due to cold exposure, which are primarily due to an individual abnormal response to cold such as acrocyanosis, pernions, cold urticaria, and cold panniculitis. In cold, controlled by the hypothalamus, vasoconstriction occurs, leading to the formation of an insulating subcutaneous layer. To avoid necrosis, vasodilation occurs again cyclically and the temperature begins to chase (so-called “hunting phenomenon of Lewis”). With prolonged pronounced exposure to cold or accompanying factors such as wet clothing or immobilization (Fig. 3) , frostbite may eventually occur.

Infections
Cutaneous infections are a particular problem in contact or martial arts. In addition to tinea gladiatorum (Fig. 4) , herpes and bacterial infections (impetigo) can also be transmitted in this way. Not only the opponent, but also, for example, in the case of tinea, the floor mats in martial arts or, in the case of bacterial infections, gloves or helmets can be a source of pathogens.
Contact allergies
Sports sometimes require special equipment and clothing. These can be the source of allergic sensitization. Thus, late-type sensitization to rubber components (thiourea, mercaptobenzothiazole), phenylenediamines, or disinfectants may occur during water sports such as diving or surfing. Anglers may develop immediate-type sensitization to fish bait (larvae of C. vomitoria and Chironomus thummi thummi).
In land sports, contact sensitization to metal parts (nickel, potassium dichromate) and rubber components (thiuram, mercaptobenzothiazole, accelerators) of sports equipment may exist. Epoxy resins as further contact allergens are very common, e.g. in protective masks for field hockey and in lacquers for billiard cues. Rarer allergens include IPPD in squash balls and the red dye Sudan IV in judo mats.
Sports creams may contain eucalyptus or peppermint as contact allergens. Topical NSAIDs, which have contact sensitizing potency, are often used for minor injuries (Fig. 5).

Doping
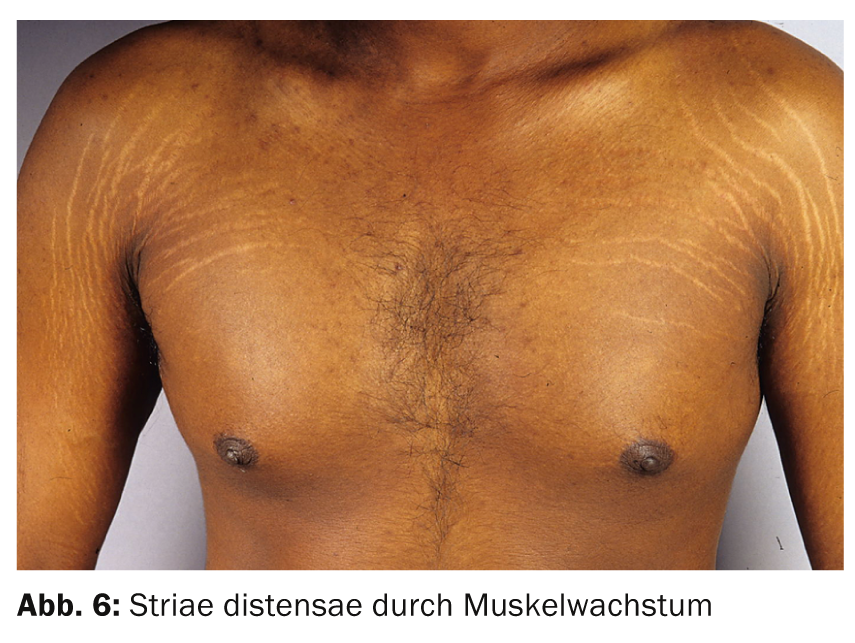
Anabolic steroids entail a variety of side effects. On the skin, acne and androgenetic alopecia are common. Striae may occur due to very rapid muscle growth (Fig. 6).
Varia
Finally, we would like to point out a clinical picture that can occur in connection with physical exercise, especially in the presence of heat: “erxercise-induced” purpura (Fig. 7) .

In this case, erythematous, urticarial plaques or purpura occur after long-distance running or walking. Women are often affected. Histology reveals leukocytoclastic vasculitis. The cause is unclear, but there does not appear to be a link with chronic venous insufficiency, although compression may be helpful as a preventive measure.
CONCLUSION FOR PRACTICE
- Many causes of sports-related skin changes are mechanical or environmental.
- In mountain sports, UV and cold exposure are the most common.
- Contact or martial arts can promote cutaneous infections.
- The equipment and clothing used in certain sports can be a source of allergic sensitization.
- Anabolic steroids often show up on the skin as acne and androgenetic alopecia.
- In “erxercise-induced” purpura, erythematous urticarial plaques or purpura occur after long-distance running or walking.
Literature:
- Levine N: Dermatologic aspects of sports medicine. J Am Acad Dermatol 1980; 3: 415-424.
- Conklin RJ: Common cutaneous disorders in athletes. Sports Med 1990; 9: 100-119.
- Pharis DB, Teller C, Wolf JE Jr: Cutaneous manifestations of sports participation. J Am Acad Dermatol 1997; 36: 448-459.
- Karamfilov T, Elsner P: Sport as a risk factor and therapeutic principle in dermatology. Dermatologist 2002; 53: 98-103.
- Möhrle M, Blum A: Skin and sport. JDDG 2004; 2: 695-702.
- Ramelet AA: Exercise-induced purpura. Dermatology 2004; 208(4): 293-296.
- Kockentiet B, Adams BB: Contact dermatitis in athletes. J Am Acad Dermatol 2007; 56: 1048-1055.
DERMATOLOGIE PRAXIS 2014; 24(3): 30-33











