The worse the blood sugar around the time of conception, the greater the risk of malformations in the child. Animal studies indicate that supplementation with vitamins and other nutrients can be used to prevent congenital malformations in children of diabetic mothers, but good human studies are lacking. At the DIP Symposium (The7th international Symposium on Diabetes, Hypertension, Metabolic Syndrome and Pregnancy) in Florence, Moshe Zloczower, MD, Haifa, Israel, presented the main ones.
Population studies show that the risk of cardiovascular malformations in children of diabetic mothers is five times higher than in the normal population. At the same time, the risk of neural tube defects and urinary tract anomalies is more than doubled [1–6]. In addition, congenital malformations increase the risk of stillbirths and perinatal mortality. Such malformations are responsible for nearly 50% of all deaths of children born to diabetic mothers [7, 8].
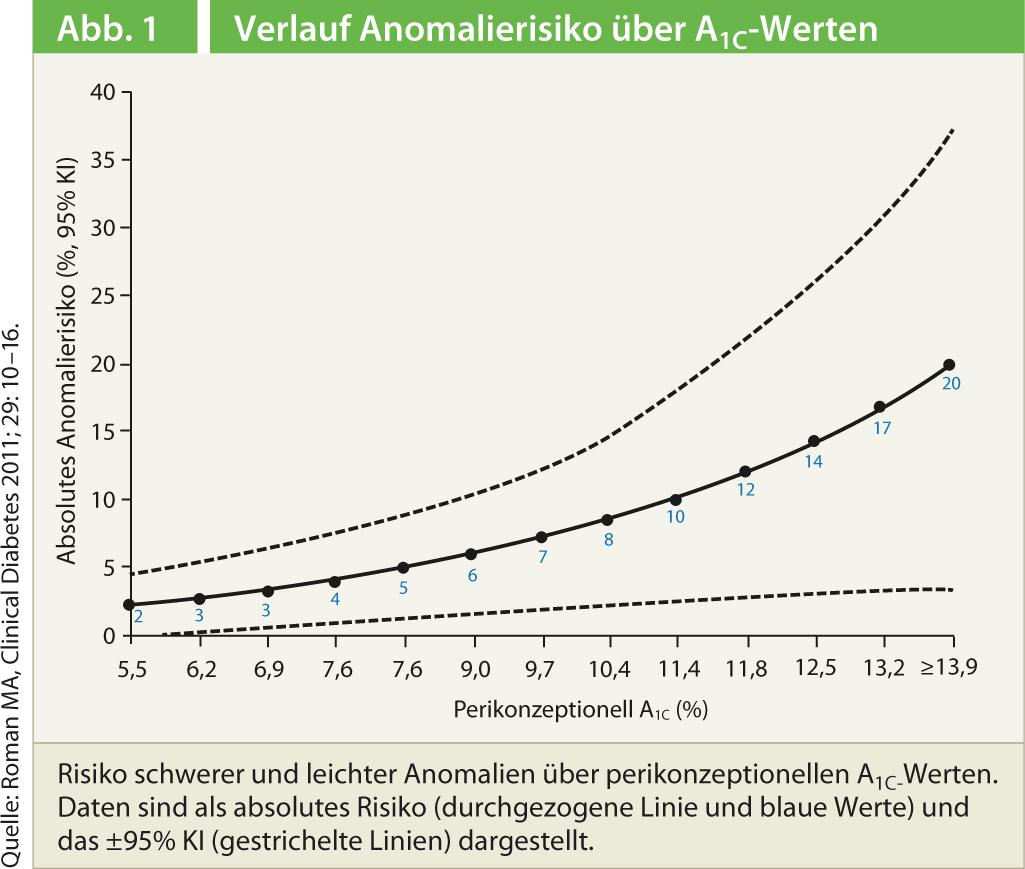
The higher the HbA1c level at the time of conception, the greater the risk of malformations in the child: if the HbA1c is lower than 8.5%, complications occur in 3.4% of cases; at higher HbA1c levels, the risk of malformations increases up to 22.4% (Fig. 1) [9].
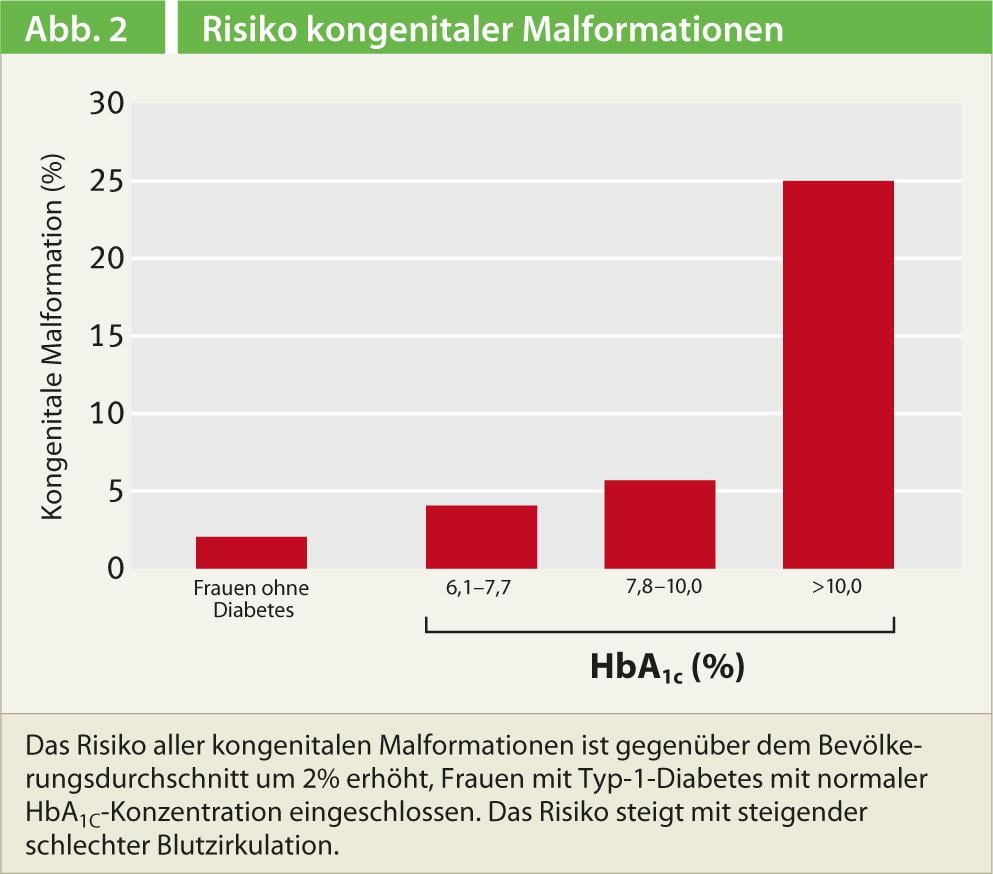
Poor glycemic control increases the risk of malformations by over 25%, but improved glucose levels can significantly reduce this (Fig. 2) [10]. “Even when HbA1c levels are normal, there are always shorter periods of hyperglycemia,” explained Moshe Zloczower, MD, Haifa, Israel, “Even these short periods can already harm the embryo.” Hyperglycemia primarily affects the embryo during organogenesis, which occurs in the first 42 days of pregnancy. The brain and heart, for example, begin to develop by the third week. “If we don’t start supplementation until then, it’s too late. To prevent malformations of the central nervous system, for example, we need to start supplementation before conception,” Dr. Zloczower said.
Several pathophysiologic mechanisms would contribute to the development of the malformations, Dr. Zloczower explained. On the one hand, lipid metabolism in the cells is disturbed. This damages the structure in the cells, free oxygen radicals are released and the oxidative stress on the tissue is increased. Second, there are fewer endogenous antioxidants. In addition, proangiogenic effects play a further role.
The molecular biological mechanisms for the teratogenic effects are not yet fully understood. A crucial role seems to be played by changes in gene expression in the embryo and yolk sac: in the signaling pathways of the Wnt gene [11, 12], protein kinase C [13], in Pax3 [14] and p53 [14], and responses of the body to hypoxia and oxidative stress [16–19].
Good evidence that supplements can be used to reduce the risk of birth defects comes from animal studies, Dr. Zloczower said. Thus, supplementation of pregnant animals with vitamins C and E [19–22], lipoic acid [23], arachidonic acid [24, 25], myo-inositol [26] or folic acid [27–29] reduced the risk of congenital anomalies. Researchers from Singapore recently showed that supplementation with zinc prevented congenital heart defects in the offspring of diabetic mice [30].
Oxidative stress caused by maternal diabetes may play a role in the development of cardiac embryopathy, the scientists suggest. Further, zinc supplementation could be a potential therapy of cardiac embryopathy.
Data on pregnant women mainly from retrospective analyses.
Studies in pregnant women have been few and of good quality, Dr. Zloczower reported. Scientists from the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in the United States retrospectively analyzed data from 3278 children with birth defects associated with diabetes in 2003 and compared them with 3029 children without congenital anomalies. Babies born to mothers with diabetes had a higher risk of birth defects if they did not take multivitamins during conception. In contrast, the risk was not increased when vitamins were taken [31]. However, these and other retrospective analyses would not allow any conclusion about a true causal relationship, according to Dr. Zloczower’s assessment.
Researchers from the National Birth Defects Prevention Study at Stanford also retrospectively analyzed the influence of maternal diet on birth defects. Mothers of 3824 infants with birth defects and 6807 controls were interviewed using a standardized dietary questionnaire. A healthier diet, as measured by the Mediterranean Diet Score (MDS), was associated with a lower risk of neural tube defects and cleft palate [32]. Another option for preventing embryonic malformations could be epigallocatechin-3-gallate (EGCG), better known as green tea. In rats, EGCG prevented hyperglycemia-induced embryopathy [33].
Literature list at the publisher
Source: DIP 2013. The7th international Symposium on Diabetes, Hypertension, Metabolic Syndrome and Pregnancy. March 13-16, 2013.











