Today, biologicals are part of the standard therapy for psoriasis. Pharmaceutical companies are conducting intensive research into new drugs. Experts believe that new biologicals with a similar mechanism of action to those already approved are just as important as preparations that target other areas. An overview.
By chance, doctors from the New Jersey-Robert Wood Johnson Medical School in the USA discovered the therapeutic potential of biologicals in psoriasis. A 57-year-old female patient had suffered from Crohn’s disease for 15 years, which had become refractory to treatment. Two weeks after an infusion with the tumor necrosis alpha inhibitor infliximab, not only did her intestinal symptoms improve, but her psoriasis improved dramatically [1].
In Switzerland, just under 2% of the population suffer from psoriasis [2]. It is now considered a systemic disease with typical skin symptoms, joint involvement and comorbidities such as rheumatoid arthritis, inflammatory bowel disease, dyslipidemia, diabetes, obesity and arterial hypertension [3–10]. The disease can extremely limit the quality of life. Patients with severe psoriasis in particular have a shorter life expectancy: they die three to four years earlier than people without the skin disease, partly due to cardiovascular sequelae such as heart attack or stroke [11]. Comorbidities require careful selection, especially of systemic therapies, to avoid adverse effects and drug-drug interactions [12].

Physical symptoms can be objectified with scores. In clinical studies, the Psoriasis Area and Severity Index (PASI) is usually used, which is also used in official guidelines as a measure of severity. The PASI indicates the extent of erythema, infiltration, and scaling on the head, arms, trunk, and legs. PASI 50, 75, or 90 means the percentage of patients who have been found to have at least a 50-, 75-, or 90-percent improvement in PASI, respectively, at a given point in time. To assess the efficacy of a new drug, a minimum 75 percent reduction in PASI (PASI 75) within 12 to 16 weeks is usually required. “In addition, however, you always have to consider the quality of life,” says PD Alexander Navarini, MD, a dermatologist at the Psoriasis Outpatient Clinic at the University Hospital Zurich and currently a Senior Visiting Research Fellow at King’s College London. This can be measured with standardized questionnaires, such as the Dermatology Life Quality Index (DLQI).
The rule of 10 helps to estimate the severity level
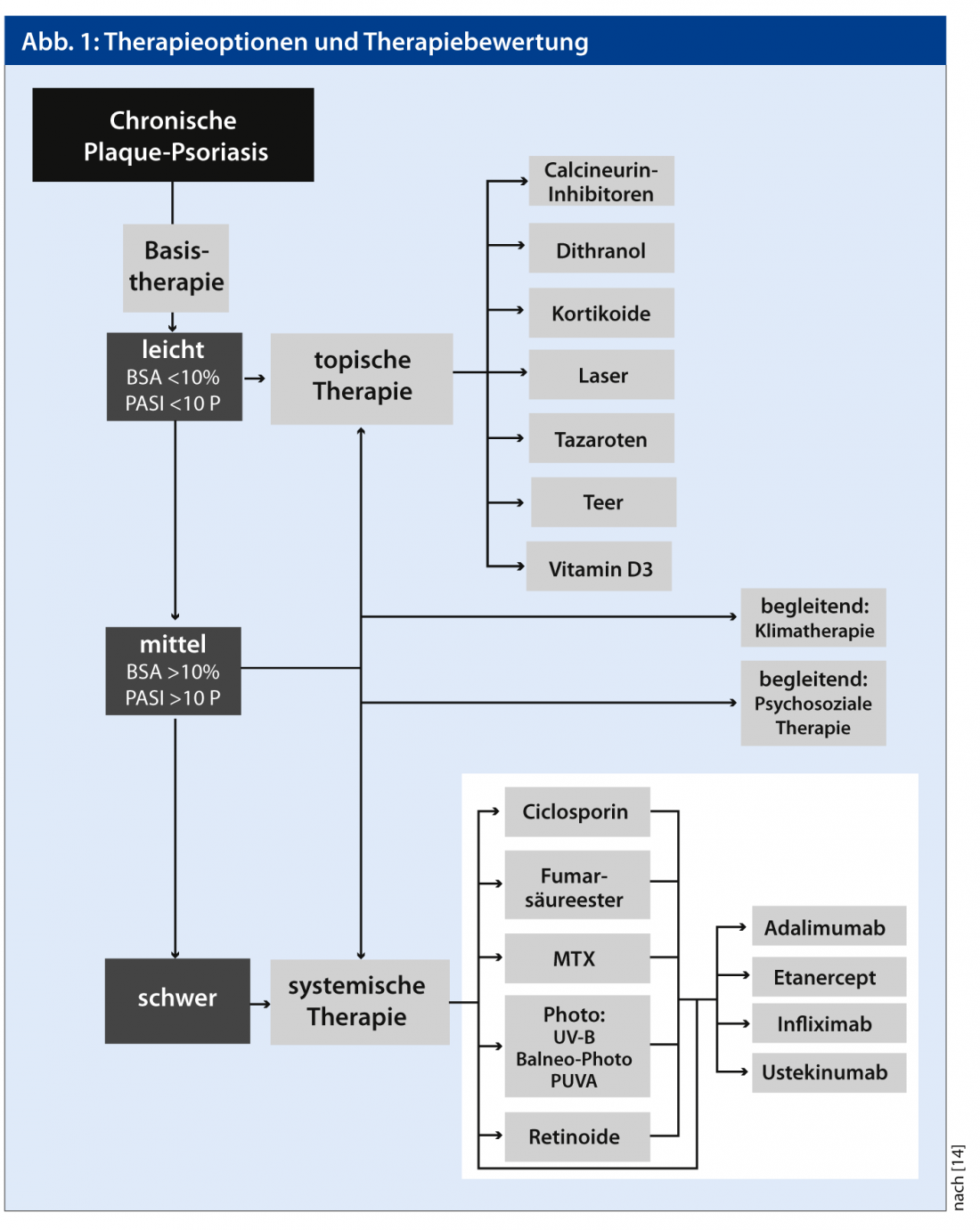
As a base, treatment is with drug-free ointment bases, urea (3-10%), salicylic acid (3-10%), and corticosteroids, often in combination with vitamin D3 derivatives, calcineurin inhibitors, and, in the hospital, dithranol. However, there are few good studies that have tested the efficacy of these topicals under controlled, comparative conditions. “For mild psoriasis, topical therapies are sufficient,” says Prof. Wolf-Henning Boehncke, MD, Chief of the Department of Dermatology at the University Hospital of Geneva. “In moderate to severe psoriasis, however, the patient needs phototherapy or systemic therapy.” As a guide to severity, the dermatologist recommends the so-called 10 rule: moderate psoriasis is present when at least 10% of the body surface is affected, the PASI is at least 10 or the quality of life is massively impaired, i.e. a DLQI of at least 10 is measured. “When considering systemic therapy, one must additionally consider other aspects, such as whether the patient has severe nail changes,” explains Prof. Boehncke.
Once it has been established that the patient suffers from at least moderate psoriasis, the next two most important questions are how quickly the therapy should take effect and whether joints are affected. For example, erythroderma requires a more rapid onset of action than marked but largely stable plaque psoriasis. With UV-B phototherapy, 50-75% of patients achieve a PASI 75, and with PUVA, 75-100% of affected individuals (AWMF guideline). Phototherapy does not serve as a long-term therapy because of the expense and long-term side effects.
Customize systemic therapy
Various preparations are available for systemic therapy (Fig. 1). “I try to take into account as many factors as possible and make a selection tailored to the patient profile, i.e. I offer personalized medicine,” says Dr. Navarini. “We have the most experience with methotrexate (MTX). If the patient tolerates it well and there are no contraindications, I like to use that as a long-term medication.” The long-known fumaric acid would be considered if someone prefers to be treated with tablets rather than the subcutaneous MTX injections. However, fumaric acid relatively often causes side effects such as flushing, nausea, diarrhea, or headache. Both drugs usually take effect within eight to twelve weeks. “If you want faster therapeutic success, you can try ciclosporin,” Dr. Navarini says. However, this is associated with even more side effects such as hypertension or renal dysfunction and is therefore only possible as a short-term therapy.
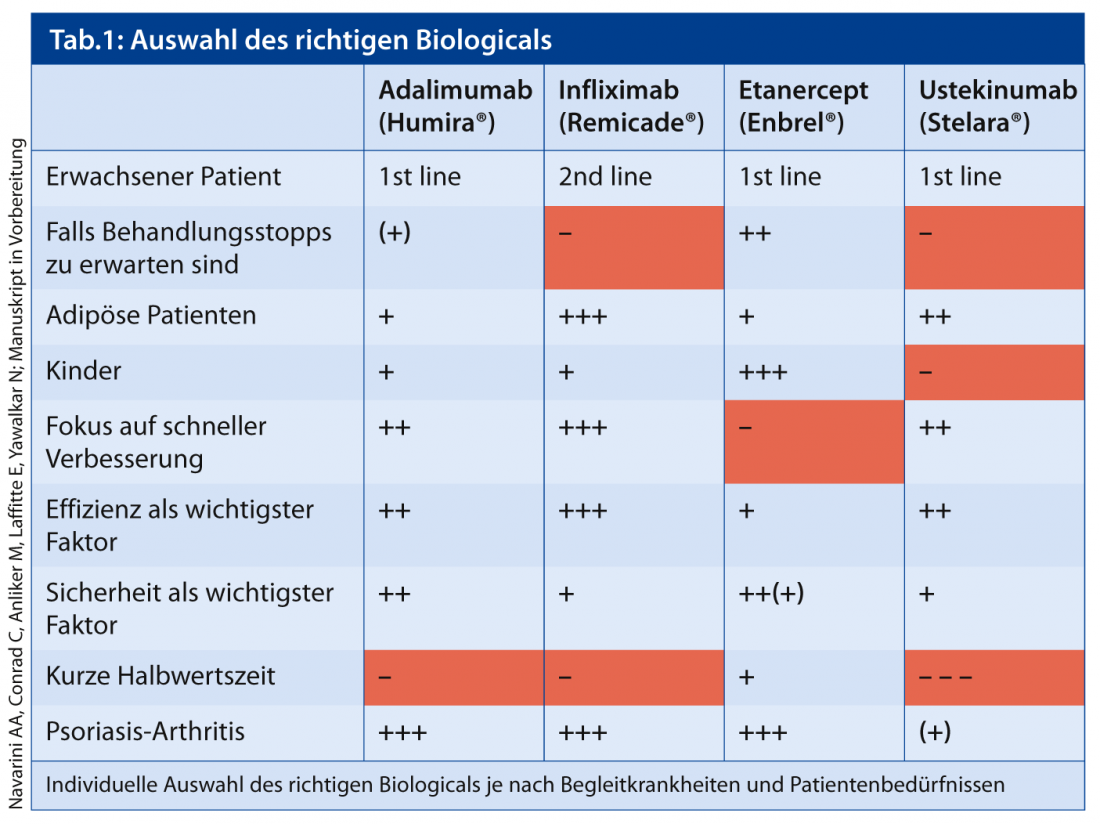
If these preparations do not help, the dermatologist recommends biologicals. “They cause fewer side effects overall and are more convenient to use – but are also much more expensive.” Which biological he uses depends on many factors (Table 1). For overweight patients with joint involvement, infliximab, for example, is a good choice. If it is foreseeable that the patient will interrupt therapy for several months, Dr. Navarini tends to recommend etanercept. “Antibodies are produced against the biologicals during the therapy pause, which bind to the drug – then the effectiveness decreases. after,” explains Dr. Navarini. Antibodies also develop against etanercept, but this does not inactivate the drug. An alternative is to combine infliximab with MTX – this should also prevent the production of the antibodies.
The TNF-alpha inhibitor golimumab is approved for the treatment of active and progressive psoriatic arthritis when the patient has had an inadequate response to prior baseline antirheumatic therapy. Currently, there are no registered studies evaluating golimumab alone in chronic plaque psoriasis. “I assume that golimumab will not be approved for the indication of skin psoriasis,” says Prof. Boehncke. “Companies are probably aware that given the rapid developments in this field, commercial success is questionable.” The TNF inhibitor certolizumab is currently being tested in Phase II and III trials. In addition to these TNF inhibitors, various preparations with other mechanisms of action are also currently being tested in clinical trials, and some could be approved in the coming years. These are, on the one hand, further biologics such as antagonists of IL-17 or IL-23 and so-called small molecules.
Psoriasis researcher Navarini considers drugs that target IL-17 or IL-23 in particular to be promising (see interview). “The pure IL-23 antagonist, which unlike ustekinumab inhibits IL-23 exclusively, sounds exciting, but it is still in very early development. The IL-17 antagonists will hopefully be approved soon and could be a good alternative for TNF inhibitors.” Prof. Boehncke suspects pharmaceutical companies are currently hesitating with their applications for approval of biologicals. “It is difficult to assess whether these drugs have good sales prospects given the biologicals that have already been approved,” Prof. Boehncke says. From a physician’s point of view, however, he says it is desirable to have as many biologicals available as possible, even if they have the same mechanisms of action. “Switching to a different biological might be a good way out if the body produces neutralizing antibodies.” The new small molecules interrupt various intracellular signaling pathways involving, for example, Janus kinase, protein kinase-C, or phosphodiesterase-4. “The charm of small molecules is primarily that they can be taken as tablets,” says Prof. Boehncke. He adds that they are no more effective than biologicals, and whether they are safer will only be clarified by longer-term observation. “Unfortunately, the small molecules will probably be similarly expensive as the biologicals.”
The dermatologist cannot imagine how psoriasis will be cured in the next few decades. “But we already have the opportunity to treat many patients so that they are no longer limited by this disease and have an almost unrestricted quality of life – much like with good diabetes therapy.” Primary care physicians should screen every psoriasis patient for joint involvement. “Early treatment of psoriatic arthritis can prevent structural damage and loss of function.” It is also important to look for comorbidities and treat them adequately. Prof. Boehncke would like to see psoriasis taken more seriously as a serious disease. “The care of patients with psoriasis is expensive, but the use of expensive biologicals is well justified in some.”
Literature:
- Oh CS, Das KM, Gottlieb AB: Treatment with antitumor necrosis factor alpha monoclonal anti-body dramatically decreases the clinical acivity of psoriasis lesions. J Am Acad Dermatol 2000; 42: 829-830.
- Ivanova K, et al: Psoriasis. Pathogenesis, clinic comorbidities. Switzerland Med Forum 2012; 12(20-21): 410-415.
- Augustin M, Reich K, Glaeske G, Schaefer I, Radtke M: Co-morbidity and age-related prevalence of psoriasis: Analysis of health insurance data in Germany. Acta Derm Venereol 2010; 90: 147-151.
- Mrowietz U, Elder JT, Barker J: The importance of disease associations and concomitant therapy for the long-term management of psoriasis patients. Archives of Dermatological Research 2006; 298: 309-319
- Mallbris L, Akre O, Granath F, Yin L, Lindelöf B, Ekbom A, Stahle-Bäckdahl M: Increased risk for cardiovascular mortality in psoriasis inpatients but not in outpatients. Eur J Epidemiol 2004; 19: 225-230.
- Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB: Risk of myocardial infarction in patients with psoriasis. JAMA 2006; 296: 1735-1741.
- Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, Giannetti A, Girolomoni G: Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. British Journal of Dermatology 2007; 157: 68-73.
- Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, Wang X, Margolis DJ, Strom BL: The risk of mortality in patients with psoriasis: results from a population-based study. Archives of Dermatology 2007; 143: 1493-1499.
- Sommer DM, Jenisch S, Suchan M, Christophers E, Weichenthal M: Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Archives of Dermatological Research 2006; 298: 321-328.
- Ludwig RJ, Herzog C, Rostock A, Ochsendorf FR, Zollner TM, Thaci D, Kaufmann R, Vogl TJ, Boehncke WH: Psoriasis: a possible risk factor for development of coronary artery calcification. British Journal of Dermatology 2007; 156: 271-276.
- Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, Wang X, Margolis DJ, Strom BL: The risk of mortality in patients with psoriasis: results from a population-based study. Archives of Dermatology 2007; 143: 1493-1499.
- Gerdes S, Mrowietz U: Impact of comorbidities on the management of psoriasis. Curr probl dermatol 2009; 38: 21-36.
- Laws PM, Young HS: Current and Emerging Systemic Treatment Strategies for Psoriasis AWMF-Guideline Psoriasis
DERMATOLOGIE PRAXIS 2013, issue 1; 26-28











