It is known that elevated levels of free fatty acids (FFA) are strongly associated with all-cause mortality in patients with coronary heart disease (CHD) and the development of type 2 diabetes (T2DM). However, there are few studies large enough to accurately examine the association between FFA levels and mortality in CHD patients with T2DM.
Free fatty acids (FFA), also known as nonesterified fatty acids (NEFA), are released from adipose tissue by lipolysis of triglycerides [2]. Previous studies indicated that elevated FFA levels are detrimental to cardiomyocytes and that FFA levels can independently predict the degree of stenosis in coronary arteries [3]. Research has found that FFAs are strongly associated with diabetes as well as cardiovascular disease and its associated risk factors. Elevated plasma FFA concentrations have been observed in some metabolic diseases associated with high risk of coronary CHD, including hypertension, T2DM, fatty liver disease, and obesity [4–7]. Excessive FFA concentration is also associated with the prognosis of CHD, including increased risk of arrhythmias, acute myocardial infarction, and all-cause and cardiovascular mortality [8–10]. However, the predictive value of FFA in cardiovascular disease remains controversial [11].
Excessive FFA is considered more harmful in cardiovascular patients with diabetes mellitus. The AleCardio study showed that baseline FFA was associated with worse prognosis in patients with T2DM and acute coronary syndrome [12]. Further data from 7535 patients from 20 provinces in China revealed that the coexistence of high FFA with pre-diabetes mellitus or diabetes mellitus multiplied the risk of worse outcomes in CHD patients [13]. However, there is currently a lack of data from additional larger cohorts reporting the role of FFA in CHD patients and individuals with different glucose metabolic status, and the actual association and mechanism of metabolic cardiovascular problems with FFA is still unclear. Therefore, a prospective study was performed to investigate the prognostic value of baseline FFA concentration in CHD patients with different T2DM status.
PRACTICE study – large, prospective cohort study.
The PRACTICE study is a large, prospective cohort study of 15,250 patients with CHD admitted to the Affiliated First Hospital of Xinjiang Medical University between December 2016 and October 2021. CAD was defined as at least one significant coronary artery stenosis with a luminal diameter of ≥70% detected by coronary angiography. Patients were excluded if they did not have FFA data, had acute infection, malignant disease, hepatobiliary disease, alcoholism, hematopoietic disease, or severe renal disease (GFR <45 ml/min, as described in the Kidney Disease Outcomes Quality Initiative (KDOQI) classification system). In addition, patients with congenital heart disease, rheumatic heart disease, valvular heart disease, cor pulmonale, or severe heart failure were excluded. Severe heart failure was defined as NYHA class IV. So that finally 10’395 CHD patients were prospectively enrolled in this study.
The primary end point was the assessment of long-term mortality, including all-cause mortality and cardiac mortality (CM), defined as death from coronary artery disease, cardiogenic shock, or sudden death. The secondary end points were serious adverse cardiovascular and cerebrovascular events (MACCEs), defined as MACE plus stroke, and serious adverse cardiovascular events (MACEs), defined as a combination of cardiac death, nonfatal myocardial infarction, and target vessel revascularization.
Data collection and measurement of free fatty acids
Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg at three time points on different days or taking antihypertensive medication. Diabetes mellitus was defined as the use of antidiabetic agents, a clear history of diabetes, fasting blood glucose ≥7.1 mmol/L, or two-hour post-exercise glucose ≥11.1 mmol/L. All definitions were given following a previous study [14].
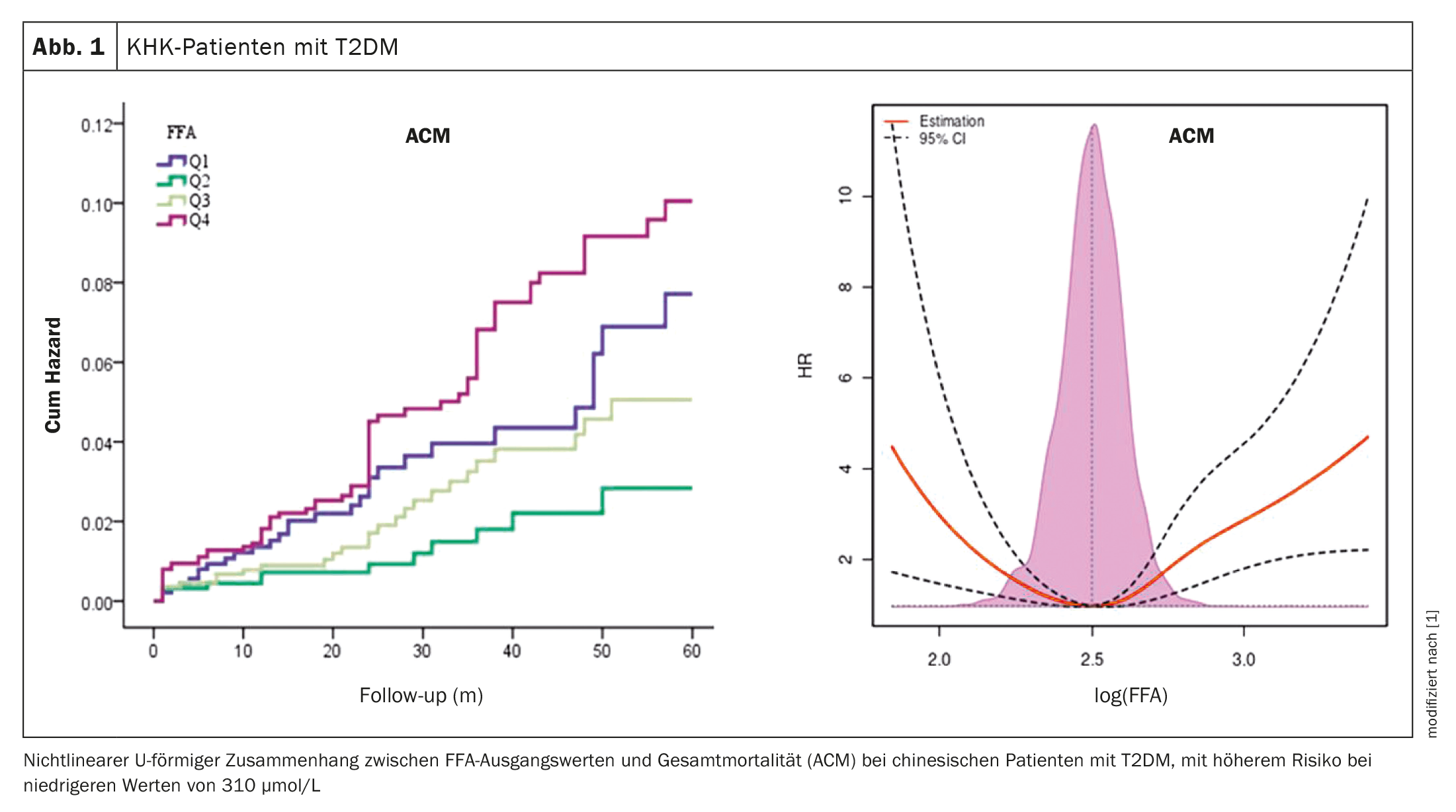
Blood samples were collected after patients had fasted for 12 to a minimum of four hours. Baseline plasma FFA was measured by the standard method of enzymatic colorimetry. The reference range is 100-900 µmol/L as described by the manufacturer. Patients were then divided into four groups according to baseline FFA: Q1: <310 µmol/L; Q2: 310–420 µmol/L; Q3: 420–580 µmol/L; Q4:>580 µmol/L.
Patient characteristics
Of the 10,395 CHD patients, those in the Q4 group tended to have a higher combination of hypertension, diabetes, MI, low eGFR, high TG, high TC, high LDL-C, elevated basal body temperature, and medication use (angiotensin receptor blockers/angiotensin-converting enzyme inhibitors), β-blockers, calcium channel blockers, and ticagrelor compared with those with lower FFA values. Similar results to baseline characteristics were found in both patients with T2DM and nondiabetic patients.
Relationship between baseline FFA levels and all-cause mortality established.
A total of 222 ACMs, 164 CMs, 718 MACEs, and 803 MACCEs were recorded during a median follow-up of 24 months. In general, as FFA categories increased from <310 to ≥580 µmol/L, there was a U-shaped curve for mortality (ACM or CM) and ischemic events (MACE or MACCE).
Individuals in Q1 and Q4 tended to have a higher risk of mortality and ischemic events compared with Q2 and Q3. Using Q2 as a reference, individuals in Q4 were found to be at higher risk for ACM [hazard ratios (HR) (95% CI): 2.496, p<0.001] and CM [HR (95% CI): 2.540, p<0.001]. In addition, individuals in Q1 had an increased risk of MACE [HR (95% CI): 1.475, p=0.001] and MACCE [HR (95% CI): 1.346, p=0.008] compared to Q3. Furthermore, individuals in Q4 had a higher risk of MACE [HR (95% CI): 1.296, p=0.029] and MACCE [HR (95% CI): 1.250, p=0.045]. Using Q2 as a reference, subgroup analysis also revealed that individuals with T2DM in Q4 had an increased risk of ACM [HR (95% CI): 3.628, p<0.001] and CM [HR (95% CI): 3.039, p=0.003]. Using Q3 as a reference, individuals with T2DM in Q4 had an increased risk of MACE [HR (95% CI): 1.586, p=0.005] and MACCE [HR (95% CI): 1.421, p=0.023]. Individuals with T2DM in Q1 were also at higher risk for MACE [HR (95% CI): 1.690, p=0.003] and MACCE [HR (95% CI): 1.515, p=0.013]. No similar results were observed in patients without T2DM.
To estimate the relative hazard ratio in all populations, the constrained cubic splines were plotted. This revealed a nonlinear U-shaped relationship between FFA concentrations and mortality (ACM and CM) or ischemic events (MACE and MACCE). In addition, the FFA concentrations associated with the lowest risk of mortality and ischemic events were 310 µmol/L and 500 µmol/L, respectively. Similar results were observed in individuals with T2DM but not in individuals without T2DM.
Take-Home-Messages
- From December 2016 to October 2021, 10 395 patients with CHD from a prospective cohort study in China (PRACTICE) were enrolled and divided into four groups according to baseline FFA concentration.
- High and low FFA levels were associated with a higher risk of mortality and ischemic events in CHD patients with T2DM.
- Baseline plasma FFA level could be a powerful, effective, and easily detectable biomarker of adverse outcomes in CHD patients with T2DM.
- As the FFA value increases, a U-shaped curve for poor long-term prognosis becomes apparent.
Literature:
- Pan Y, et al.: Decreased free fatty acid levels associated with adverse clinical outcomes in coronary artery disease patients with type 2 diabetes: findings from the PRACTICE study. European Journal of Preventive Cardiology 2023;
doi: https://doi.org/10.1093/eurjpc/zwad073. - Stanley WC, Recchia FA, Lopaschuk GD: Myocardial substrate metabolism in the normal and failing heart. Physiol Rev 2005; 85: 1093–1129.
- Yang R F, et al.: A study on the relationship between waist phenotype, hypertriglyceridemia, coronary artery lesions and serum free fatty acids in adult and elderly patients with coronary diseases. Immun Ageing 2018; 15: 1–6.
- Tabara Y, et al.: Association of serum–free fatty acid level with reduced reflection pressure wave magnitude and central blood pressure: the Nagahama study. Hypertension 2014; 64: 1212–1218.
- Steffen BT, et al.: n-3 Fatty acids attenuate the risk of diabetes associated with elevated serum nonesterified fatty acids: the multi-ethnic study of atherosclerosis. Diabet Care 2015; 38: 575–580.
- Martchenko A, Brubaker PL: Effects of obesogenic feeding and free fatty acids on circadian secretion of metabolic hormones: implications for the development of type 2 diabetes. Cells 2021; 10: 2297.
- Lee MR, Park KI, Ma JY: Leonurus japonicus Houtt attenuates nonalcoholic fatty liver disease in free fatty acid-induced HepG2 cells and mice fed a high-fat diet. Nutrients 2017; 10: 20.
- Oliver MF, Opie LH: Effects of glucose and fatty acids on myocardial ischaemia and arrhythmias. Lancet 1994; 343: 155–158.
- Pilz S, et al.: Free fatty acids are independently associated with all-cause and cardiovascular mortality in subjects with coronary artery disease. J Clin Endocrinol Metab 2006; 91: 2542–2547.
- Roy VK, et al.: Plasma free fatty acid concentrations as a marker for acute myocardial infarction. J Clin Diagn Res 2013; 7: 2432–2434.
- Charles MA, et al.: High plasma nonesterified fatty acids are predictive of cancer mortality but not of coronary heart disease mortality: results from the Paris prospective study. Am J Epidemiol 2001; 153: 292–298.
- Schrieks IC, et al.: Adiponectin, free fatty acids, and cardiovascular outcomes in patients with type 2 diabetes and acute coronary syndrome. Diabet Care 2018; 41: 1792–1800.
- Jin JL, et al.: Impact of free fatty acids on prognosis in coronary artery disease patients under different glucose metabolism status. Cardiovasc Diabetol 2019; 18: 1–9.
- Zheng YY, et al.: Gamma-glutamyl transferase-to-platelet ratio as a novel predictor of long-term adverse outcomes in patients after undergoing percutaneous coronary intervention: a retrospective cohort study. Thromb Haemost 2019; 119: 1021–1030.
CARDIOVASC 2023; 22(3): 52–53