The new edition of the guideline “Diagnosis, prevention and treatment of hand eczema”, which was published this year under the auspices of the German Dermatological Society, focuses in particular on the classification of severity and the step-by-step therapy scheme. Topical, physical and systemic therapy options are currently available for the treatment of hand eczema. In addition, numerous research projects are underway to develop new treatment options.
Chronic hand eczema is eczema localized on the hands that lasts longer than three months or occurs at least twice a year [1]. Hand eczema can spread over a large area or be limited to certain parts of the hands, e.g. the palms, the spaces between the fingers and the fingertips. If a large area is affected at the beginning of the disease, this indicates a poor prognosis [2]. The severity of hand eczema ranges from very mild to severe, chronic and painful. “The Hand Eczema Severity Index (HECS) score or the validated Photographic Guide can also be used to assess the severity of hand eczema,” explained Prof. Dr. Andrea Bauer, Senior Physician at the Clinic and Polyclinic for Dermatology at the Carl Gustav Carus University Hospital in Dresden [3].
The symptoms are very distressing for those affected: the skin on the hands and wrists is red, itchy and painful. There are certain occupational groups that carry a particularly high risk of developing hand eczema. In addition to the healthcare sector, these include the hairdressing industry, the metal industry, cleaning companies and professions in the food industry and gastronomy (box). Cracked skin, swelling, blisters and inflammation with weeping, crusty lesions affect everyday life. “Chronic hand eczema has a high health economic and socio-medical significance,” summarized Prof. Bauer [3].
| Atopic dermatitis as a risk factor for hand eczema An atopic disposition increases the risk of developing hand eczema with regular exposure to irritants and allergens, as the skin’s protective barrier is usually impaired. If the epidermal barrier is impaired, this enables the penetration of allergens and irritants into the skin and leads to local immune activation. Mutations in the filaggrin gene with a reduction in structural proteins play an important role in the deficits in barrier integrity known to occur in atopic dermatitis. In an overview article by Ruff et al. it is pointed out that the point prevalence and lifetime prevalence of hand eczema is 2 to 4 times higher in patients with atopic dermatitis [26]. Dermatologists should therefore make younger patients with atopic dermatitis aware of the implications of the disease in relation to occupational aspects or career choices [27]. |
Symptomatology has far-reaching psychosocial consequences
Hand eczema has the same negative impact on health-related quality of life (HRQoL) as psoriasis or asthma [4,5]. These negative effects are more pronounced for women than for men and women [6,7]. The socio-economic consequences are also considerable: hand eczema can lead to a reduced ability to work, as various empirical studies have shown.
In a Danish prospective study, 57% of patients with work-related skin disease had been on sick leave in the previous 12 months, 44% reported a change of job, 15% took early retirement, and 72% suffered from impaired HRQoL [4]. In addition, severe occupational hand eczema, age 40 years or older and severely impaired HRQoL at baseline were predictors of long-term disability and unemployment [4]. A multicenter study found that hand eczema sufferers have significantly higher levels of stress, suicidal thoughts, depression and anxiety compared to control subjects [6]. In another multi-center study, 28% of hand eczema patients were unable to work, and in 12% of cases the inability to work lasted longer than 12 weeks [8]. Of the people who stated that they had suffered from hand eczema in the last 12 months, 67% were referred to a general practitioner and 44% to a dermatologist in Denmark [9].
Detailed medical history – possibly perform epicutaneous testing
In addition to the medical history, including personal and occupational exposure, the clinical examination and skin tests are important components of the diagnostic work-up [1]. Epicutaneous testing is indicated if the hand eczema has persisted for more than three months, if the symptoms do not respond to therapy or if there is a clinical suspicion of a contact allergy. If necessary, the diagnostic spectrum can be extended by a histopathological examination and microbiological tests.
The current guideline distinguishes between the following etiologic subtypes of hand eczema [1]:
- allergic contact dermatitis
- atopic hand eczema
- Protein contact dermatitis (with and without contact urticaria)
- Irritant contact dermatitis
For the diagnosis of allergic contact dermatitis, local and temporally relevant allergen exposure and contact sensitization to the suspected allergen(s) must be proven. Atopic hand eczema can be associated with an inherent impairment of the skin barrier, e.g. filaggrin deficiency. Further indications of atopic hand eczema may be a positive personal history of atopic eczema, atopic eczema in another location (e.g. flexural eczema) or other atopic diseases. Hand eczema due to protein contact dermatitis is rare, the diagnosis is made on the basis of evidence of an immediate type sensitization to a protein (prick test, specific IgE) and an eczema reaction to this protein (usually meat, fish, vegetables and fruit in people who handle food). Protein contact dermatitis can also be accompanied by contact urticaria on the protein. Irritant contact dermatitis is a diagnosis of exclusion; it requires that other etiologies, in particular allergic contact dermatitis, have been ruled out and that exposure to skin irritants is present.
In addition to the differentiation according to the causes of eczema, the following classification according to clinical manifestations is proposed:
- hyperkeratotic HE
- Acute recurrent vesicular HE
- nummular HE
- Pulpitis (eczema of the fingertips)
If more than one aetiological and clinical subtype is present (e.g. aetiologically combined irritant contact dermatitis and atopic hand eczema), this is referred to as a “mixed form”. The epicutaneous test is the gold standard for the diagnosis of contact allergies [11].
Topical and physical treatment measures
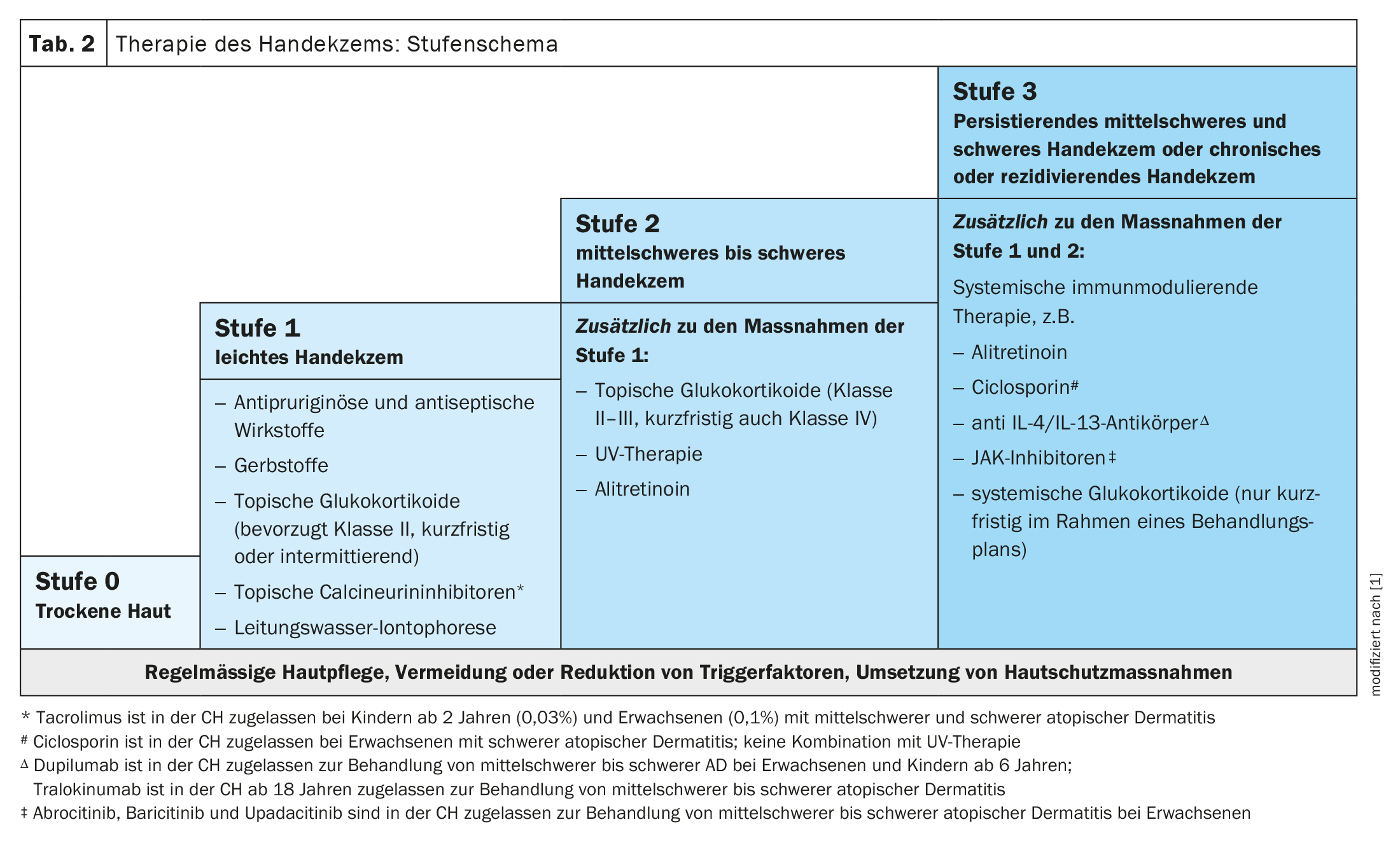
In addition to general protective measures and exposure prophylaxis, the regular use of skin care products is advisable both for basic therapy and for the prevention of hand eczema. This is intended to supply the skin with moisture and lipids, which contributes to the regeneration of the skin barrier after skin stress [12–16]. Any further therapy should be carried out according to the severity of the hand eczema (Table 1). The Hand eczema severity index (HECS) score is a validated, morphology-based tool that maps the severity on a point scale (0=healed, 1-16= almost healed, 17-37= moderate, 38-116= severe, ≥ 117 = very severe) [17–20].
A compact overview of the treatment recommendations is shown in Table 2 .
Topical glucocorticosteroids with low atrophogenic potential are the treatment of choice for mild HE (stage 1) and moderate to severe HE (stage 2). A Cochrane review on the treatment of hand eczema published in 2019 included nine studies on the use of topical glucocorticoids [21]. Six studies were of short duration (three weeks or less) and mostly compared two glucocorticoids or the same glucocorticosteroid, but with different vehicles or dosages or application intervals. All studies mentioned show a reduction in the severity of the disease, although the certainty of the evidence was not assessed according to GRADE. The occurrence of side effects of topical glucocorticoids depends on the potency, the amount used, the duration of treatment, the frequency of application and the anatomical localization. The authors of the guidelines recommend once-daily treatment with glucocorticoids. This is sufficient and possibly even superior to twice-daily application.
Topical calcineurin inhibitors may be considered alternating with or combined with topical glucocorticosteroids to reduce adverse effects of steroids [22]. The 2019 Cochrane review included four studies with limited numbers of participants on tacrolimus (107 participants in total) and five larger studies on pimecrolimus (1059 participants), of short duration (≤8 weeks) [21]. Tacrolimus 0.1% ointment improves symptom control measured after three weeks compared to vehicle (14/14 tacrolimus versus 0/14 vehicle) according to medical opinion [23].
Phototherapy (topical PUVA, narrowband UVB, UVA1) of the hands may be considered in adult patients with moderate to severe chronic hand eczema that does not respond to topical glucocorticoids. Undesirable effects of phototherapy, especially local PUVA, in which only the affected skin areas are treated with psoralen-containing creams or baths, are erythema and skin burns [24]. In addition, long-term use increases the risk of non-melanocytic skin cancer [24].
Systemic therapy – alitretinoin has proven its worth
The oral vitamin A derivative (retinoid) alitretinoin has been used successfully for years as an oral therapy for stage 2 and stage 3 (persistent moderate and severe hand eczema). Alitretinoin should be used if topical treatment and/or phototherapy alone are not sufficiently effective. It has also been shown that the efficacy of systemic treatment with alitretinoin is increased by additional topical therapy with glucocorticoids.
Four studies of alitretinoin compared with placebo were included in the Cochrane review published in 2019 [21]. These studies included doses of 10 mg and 30 mg compared to placebo and were evaluated according to GRADE. Two RCTs (n=1210) investigated the efficacy of alitretinoin 30 mg compared to placebo in patients with severe chronic hand eczema that did not respond to standard treatment (skin care products could be used in both arms). The most important endpoints included the proportion of participants who achieved good/excellent symptom control (=symptom-free or almost symptom-free; IGA/PaGA 0 or 1 on a scale of 0-4). According to the investigators, 44.4% achieved good or very good control with alitretinoin (30 mg) and 15.7% with placebo. According to the participants’ assessment, 39.6% achieved good or very good control with alitretinoin (30 mg) compared to 14.3% with placebo.
The same primary endpoints were used in two RCTs on alitretinoin 10 mg compared to placebo (n=781). Here, the investigators reported good/very good control in 29.3% with alitretinoin and in 19.4% with placebo. From the participants’ point of view, 24.8% achieved good or very good control with alitretinoin compared to 14.4% with placebo. The rate of adverse events did not differ between alitretinoin 10 mg and placebo. The risk of headaches increased with alitretinoin 30 mg.
Other systemic active substances: off-label or still under investigation
With the exception of alitretinoin, no other systemic therapies are currently approved for the treatment of chronic hand eczema. Oral glucocorticoids (maximum three weeks, starting at 0.5 mg/kg/day), acitretin, ciclosporin, azathioprine and methotrexate are sometimes used off-label. Further systemic active substances are currently being researched. In a prospective observational study of 47 patients with atopic dermatitis and hand eczema, dupilumab led to at least 75% improvement in HECSI (HECSI-75) after 16 weeks in 60% of patients [25]. IL-13 antagonists and systemic JAK inhibitors are also expected to prove effective in atopic hand eczema.
As the aetiology, morphology and endotypic characteristics of hand eczema vary between individuals, one focus of research into drug therapies is to investigate how different subgroups of patients respond to certain active substances. Hyperkeratotic subtypes are thought to benefit more from retinoids, while Th2-triggered forms are more likely to respond to Th2-targeted therapies such as dupilumab or tralokinumab. The efficacy profile of JAK inhibitors in hand eczema is also currently the subject of research.
Literature:
- S2k guideline “Diagnosis, prevention and therapy of hand eczema”, AWMF register no.: 013-053, status: 23/02/2023, valid until: 22/02/2028.
- Meding B, Wrangsjö K, Järvholm B: Hand eczema extent and morphology–association and influence on long-term prognosis. J Invest Dermatol 2007; 127: 2147-2151.
- “Guideline hand eczema: Severity classification and therapy step scheme updated. Outlook on the potential of modern topical and systemic therapeutics”, DDG, 19.07.2023
- Cvetkovski RS, et al: Quality of life and depression in a population of occupational hand eczema patients. Contact Dermatitis. 2006; 54: 106-111.
- Moberg C, Alderling M, Meding B: Hand eczema and quality of life: a population-based study. BJD 2009; 161: 397-403.
- Agner T, et al: Hand eczema severity and quality of life: a cross-sectional, multicenter study of hand eczema patients. Contact Dermatitis 2008; 59: 43-47.
- Marron SE, et al: The psychosocial burden of hand eczema: Data from a European dermatological multicenter study. Contact Dermatitis 2018; 78: 406-412.
- Diepgen TL, et al: Guideline on the management of hand eczema ICD 10 Code: L20. L23. L24. L25. L30. JDDG 2009; 7 Suppl 3: S1-16.
- Hald M, et al: Medical consultations in relation to severity of hand eczema in the general population. BJD 2008; 158: 773-777.
- Meding B, Swanbeck G: Predictive factors for hand eczema. Contact Dermatitis 1990; 23: 154-161.
- Johansen JD, et al: European Society of Contact Dermatitis guideline for diagnostic patch testing – recommendations on best practice. Contact Dermatitis 2015; 73: 195-221.
- Williams C, et al: A double-blind, randomized study to assess the effectiveness of different moisturizers in preventing dermatitis induced by hand washing to simulate healthcare use. BJD 2010; 162: 1088-1092.
- De Paépe K, et al: Beneficial effects of a skin tolerance-tested moisturizing cream on the barrier function in experimentally-elicited irritant and allergic contact dermatitis. Contact Dermatitis 2001; 44: 337-343.
- Ramsing DW, Agner T: Preventive and therapeutic effects of a moisturizer. An experimental study of human skin. Acta Derm Venereol. 1997; 77: 335-337.
- Hannuksela M: Moisturizers in the prevention of contact dermatitis. Curr Probl Dermatol 1996; 25: 214-220.
- Zhai H, Maibach HI: Moisturizers in preventing irritant contact dermatitis: an overview. Contact Dermatitis 1998; 38: 241-244.
- Held E, et al: The hand eczema severity index (HECSI): a scoring system for clinical assessment of hand eczema. A study of inter- and intraobserver reliability. BJD 2005; 152: 302-307.
- Oosterhaven JAF, Schuttelaar MLA: Responsiveness and interpretability of the Hand Eczema Severity Index. BJD 2020; 182: 932-939.
- Yüksel YT, Agner T, Ofenloch R: New evidence on the minimally important change (MIC) for the Hand Eczema Severity Index (HECSI). Contact dermatitis. 2021 Mar 3. doi: 10.1111/cod.13828.
- Coenraads PJ, et al: Construction and validation of a photographic guide for assessing severity of chronic hand dermatitis. BJD 2005; 152: 296-301.
- Christoffers WA, et al: Interventions for hand eczema. Cochrane Database Syst Rev 2019; 4: Cd004055.
- Schnopp C, et al: Topical tacrolimus (FK506) and mometasone furoate in treatment of dyshidrotic palmar eczema: a randomized, observer-blinded trial. JAAD 2002; 46: 73-77.
- Pacor ML, et al: Tacrolimus ointment in nickel sulphate-induced steroid-resistant allergic contact dermatitis. Allergy Asthma Proc 2006; 27: 527-531.
- Nijsten TE, Stern RS: The increased risk of skin cancer is persistent after discontinuation of psoralen + ultraviolet A: a cohort study. J Invest Dermatol 2003; 121: 252-258.
- Oosterhaven JAF, et al: Effect of dupilumab on hand eczema in patients with atopic dermatitis: An observational study. J Dermatol 2019; 46: 680-685.
- Ruff SMD, et al: The association between atopic dermatitis and hand eczema: a systematic review and meta-analysis. BJD 2018; 178: 879-888.
- Wollenberg A, et al: ETFAD/EADV eczema task force 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. JEADV 2020; 34: 2717-2744.
DERMATOLOGY PRACTICE 2023; 33(5): 23-26