The drug treatment options for many chronic inflammatory dermatoses have improved enormously in recent years. And yet light therapy has a firm place in the therapeutic landscape
and should also be offered to patients in the sense of personalized medicine, according to a statement by the German Society of Dermatology (DDG). In this context, a publication recently appeared in the JDDG that provides an up-to-date overview of the practical implementation of phototherapy.
“Irradiation with UV light is still an indispensable part of dermatological work,” says Prof. Dr. med. Mark Berneburg, Director of the Clinic and Polyclinic for Dermatology at Regensburg University Hospital and Secretary General of the DDG [1]. Only the long-wave UV-A rays and the shorter-wave UV-B rays are used for therapeutic purposes. “Phototherapy deserves a renaissance. Patients with comorbidities who are already receiving many medications will benefit in particular,” added Prof. Dr. med. Silke Hofmann, Chief Physician at the Center for Dermatology, Allergology and Dermatosurgery, HELIOS University Hospital Wuppertal [1]. The expert currently responsible for the DDG’s public relations work pointed out that polypharmacy, i.e. taking five or more different medicines, is a reality for many people – not just senior citizens – and that phototherapy is a very good option for treating a skin disease for this patient group.
Can be used for various dermatological indications
In the overview article published in the JDDG by Kurz et al. the following indications for phototherapy are described in more detail [2].
- Psoriasis
- Atopic dermatitis
- Prophylaxis of photodermatoses
- Mycosis fungoides
- Vitiligo
- Graft versus host disease (GvHD)
- sclerosing connective tissue diseases
The following mechanisms of action are named as key components of phototherapy: Proapoptotic effects, immunomodulatory effects, propigmenting effects (production of proopiomelanocortin and α-MSH; depletion of antimelanocytic CD8 T cells), antifibrotic mechanisms (induction of collagen-degrading matrix metalloproteinases), antipruritic effects, pro- and prebiotic effects.
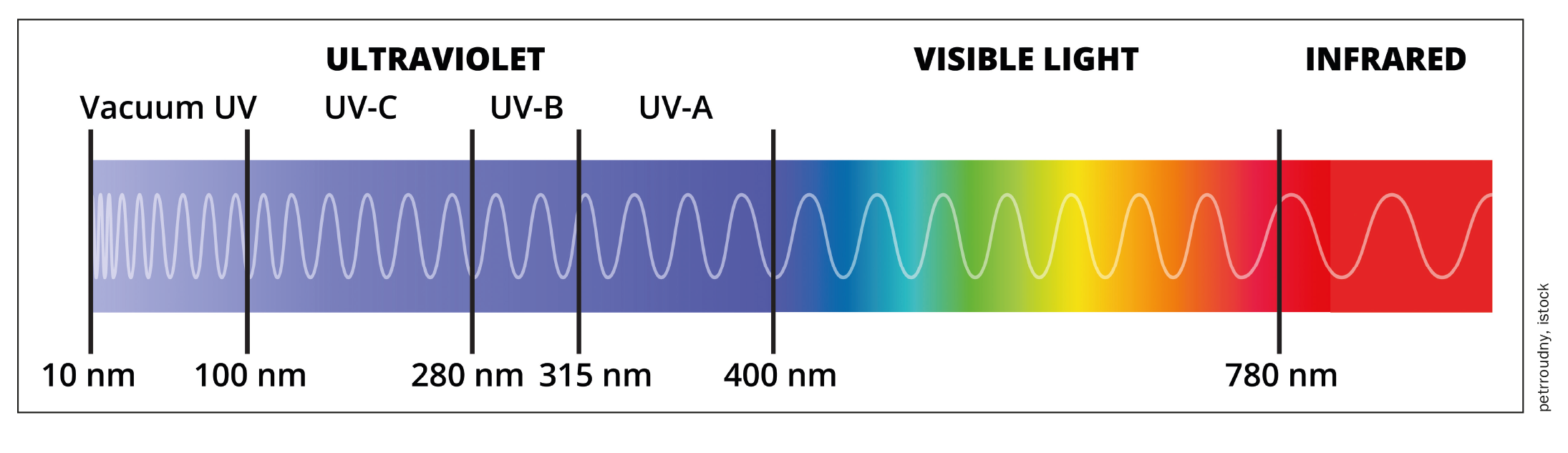
UV-A rays have a wavelength of 315-380 nm and penetrate the dermis. They act on inflammatory cells and specific connective tissue cells. The combination of UV-A with the photosensitizer psoralen (PUVA therapy) has proven to be an effective treatment option for psoriasis and cutaneous T-cell lymphomas, for example.
UV-B rays have a wavelength of 280-315 nm and reach the epidermis. The long-wave component of UV-B light has a particular effect in the lower layers of the epidermis, especially in the basal cell layer. Cell division in the basal cell layer of the epidermis is inhibited, which leads to an improvement in the inflammatory skin changes and a reduction in scaling and is therefore particularly useful in the treatment of psoriasis. According to Prof. Berneburg, patients with moderate and severe psoriasis in particular would benefit from this. In the indications psoriasis, atopic dermatitis (AD), vitiligo and polymorphic light dermatosis, narrowband UVB therapy has proven to be therapeutically superior to broadband UVB therapy [3].
UVB therapy and medium- to low-dose UVA1 therapy can be used for moderate chronic AD [4]. In acutely exacerbated severe AD, high-dose UVA1 therapy and systemic PUVA therapy showed the highest efficacy [5,6]. According to the current European guideline for the treatment of AD, children with moderate AD (SCORAD index 25-50) can also be treated with narrowband UVB [7].
“Modern phototherapy is not only very effective, but also has few side effects,” emphasized Prof. Berneburg [1]. According to current knowledge, there is no increased risk of skin cancer for narrow-band UVA and UVB therapy when used correctly. High broadband UVB doses (over 300 treatments) are associated with a moderate increase in non-melanocytic skin tumors [8]. The study data for narrow-band UVB therapy do not yet allow any clear conclusions to be drawn. [10]. A significantly increased risk for the occurrence of squamous cell carcinoma has only been described after more than 150 PUVA treatments [9].
What needs to be considered during practical implementation?
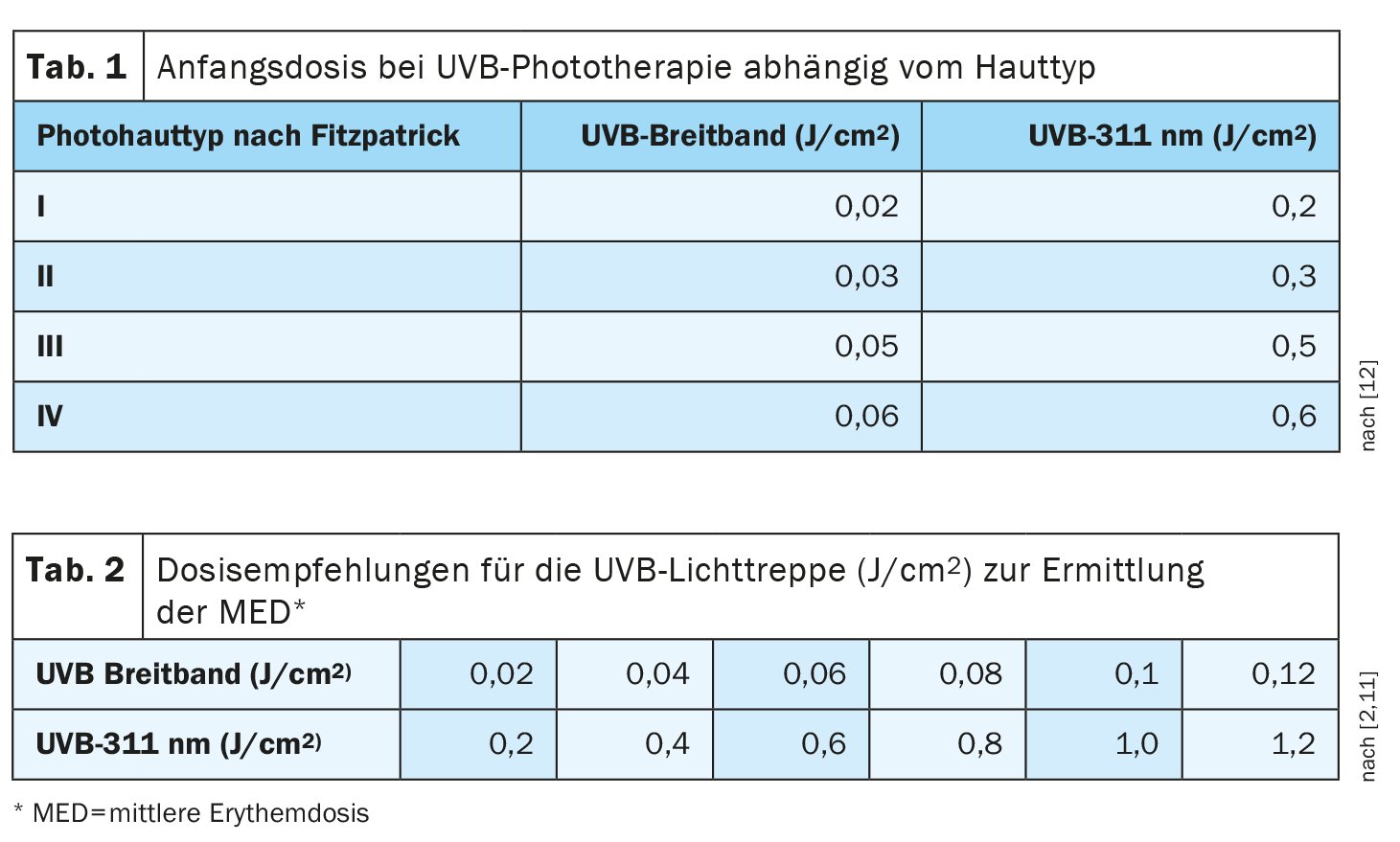
In the overview article by Kurz et al. The following are various points that need to be observed for proper application in order to ensure the most effective and safe phototherapy possible [2]. Before starting UVB phototherapy, the first irradiation dose is generally determined either according to the skin type according to Fitzpatrick using a standardized scheme (Table 1) or by determining the minimum erythema dose (Table 2). The minimum erythema dose (MED) is determined using the type of lamp intended for the therapy by applying light stairs to skin that is not exposed to light (e.g. buttocks or lower back). The MED is defined as the lowest radiation dose that causes a barely visible erythema. It is determined 24 hours after irradiation. For safety reasons, 70% of the determined MED is used as the initial dose.
It is recommended that UVB treatment be carried out three to five times a week using a standardized dose schedule. The UVB 311 nm erythema is maximally pronounced after 12-24 hours. The increase in the light dose depends on the effect of the previous irradiation and can vary between 10-30%. Depending on the indication, around 25 radiotherapy sessions are required to achieve remission. Once freedom from manifestations has been achieved, long-term maintenance therapy (with the exception of selected cases of mycosis fungoides) is not indicated [11].
| Combination therapy for atopic dermatitis Phototherapy for AD is usually carried out 3-5 times a week for 6-12 weeks and can also be combined well with topical glucocorticoids. With the increasing use of biologics, their combination with UV radiation is also being investigated. Rossi et al. published a study in 2021 in which 45 patients with severe AD received 12 weeks of treatment with dupilumab alone or with dupilumab plus narrow-band UVB. After week 12, all patients received only dupilumab. The combined regimen resulted in greater clinical improvement of the lesions and relief of symptoms after 4 weeks. After 12 and 16 weeks, however, the additional therapeutic effect of phototherapy weakened. |
| to [2,13] |
There is also information on the practical implementation of UVA1 phototherapy and photochemotherapy (PUVA) in the review article by Kurz et al. detailed information. The relatively new concept of UVA1 phototherapy is not as standardized as UVB irradiation, but can be divided into three dose ranges [11]:
- low-dose UVA1 therapy with a single dose of 10-20 J/cm2,
- Medium-high dose UVA1 therapy with a single dose of >20-70 J/cm2,
- High-dose UVA1 therapy with a single dose >70-130 J/cm2.
Individual test regimens apply to cream PUVA therapy, but these are closely based on bath PUVA therapy and their dosage depends on the concentration used in the cream. Locally circumscribed light-sensitive dermatoses in particular are a good indication for cream PUVA therapy.
With regard to relative and absolute contraindications, Kurz et al. following notes [2]:
- Genetic defects with increased sensitivity to light or an increased risk of skin cancer (e.g. xeroderma pigmentosum, Cockayne syndrome, trichothiodystrophy, Rothmund-Thomson syndrome, Bloom syndrome, Gorlin-Goltz syndrome) are absolute contraindications to phototherapy.
- Taking photosensitizing medication (usually in the UVA wavelength range) that cannot be discontinued is not automatically a contraindication to light therapy. However, precautionary measures such as lower radiation doses and a slower increase in the light dose are necessary.
- Other relative contraindications that should be checked before initiating light therapy are: familial melanoma syndromes, lupus erythematosus, previous excessive UV exposure, previous exposure to ionizing radiation, current or previous malignant skin tumors, current precancerous lesions (actinic keratoses, Bowen’s disease) and previous use of immunosuppressive medication (ciclosporin, azathioprine, mycophenolate mofetil, tacrolimus).
- Simultaneous systemic therapy with ciclosporin, azathioprine, mycophenolate mofetil or tacrolimus is generally contraindicated.
- Frail patients, patients with poor circulation or people with uncontrolled epilepsy who cannot stand upright in the UV cabin for long enough are also not eligible for the therapy.
- PUVA therapy (system and bath PUVA) is contraindicated in pregnant and breastfeeding women in accordance with the expert information for psoralens, although there is no evidence to date of teratogenicity of psoralens. However, light therapy with UVB (broadband and narrowband) can also be carried out during pregnancy and breastfeeding. Since folic acid degrades at cumulative doses above 40 J/cm2 or an average of 2 J/cm2 per therapy, women of childbearing age who wish to have children and pregnant patients undergoing narrow-band UVB therapy should receive 0.8 mg folic acid daily.
Literature:
- “‘Healing light’ for diseased skin: phototherapy with UV-A and UV-B rays”, German Dermatological Society (DDG), 16.01.2024.
- Kurz B, et al: Phototherapy in theory and practice. JDDG 2023; 21(8): 882-898.
- Stege H, Ghoreschi K, Hünefeld C: UV phototherapy. The dermatologist 2021; 72(1): 14-26.
- Krutmann J, Hönigsmann H: Handbook of dermatologic phototherapy and photodiagnostics. Springer-Verlag, 2013.
- Krutmann J, et al: High-dose UVA1 therapy for atopic dermatitis: results of a multicenter trial. J Am Acad Dermatol 1998; 38(4): 589-593.
- Krutmann J, et al: High-dose UVA1 therapy in the treatment of patients with atopic dermatitis. J Am Acad Dermatol 1992; 26(2): 225-230.
- Wollenberg A, et al: Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol 2018; 32(5): 657-682.
- Lim JL, Stern RS: High levels of ultraviolet B exposure increase the risk of non-melanoma skin cancer in psoralen and ultraviolet A-treated patients. J Invest Dermatol 2005; 124(3): 505-513.
- Star RS. Study PF-U: The risk of squamous cell and basal cell cancer associated with psoralen and ultraviolet A therapy: a 30-year prospective study. J Am Acad Dermatol 2012; 66(4): 553-562.
- Archier E, et al: Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012; 26: 22-31.
- Herzinger T, et al: S1-Guidelines on UV phototherapy and photochemotherapy. J Dtsch Dermatol Ges 2016; 14(8): 853-876.
- Fitzpatrick TB: The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol 1988; 124(6): 869-871.
- Rossi M, et al: A short cycle of narrow-band UVB phototherapy in the early phase of dupilumab therapy can provide a quicker improvement of severe atopic dermatitis. Dermatology 2021; 237(3): 407-415.
DERMATOLOGY PRACTICE 2024; 34(2): 47-48