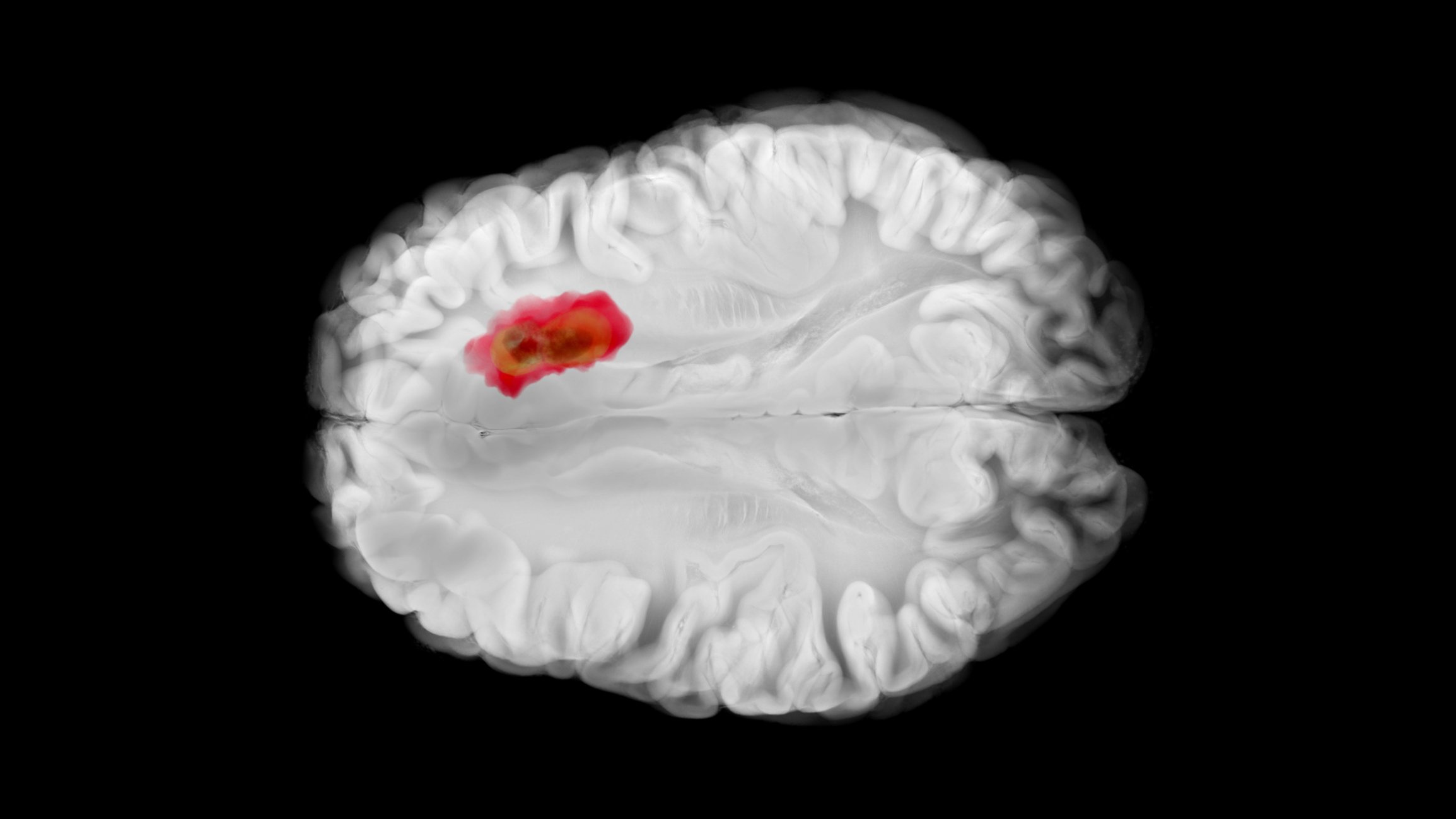
The pursuit of individuality was the focus of this year’s Congress of Oncology and Hematology in Switzerland. This paradigm shift is set to change patients’ lives and redefine cancer treatment. Advances in genomics, molecular biology and data analysis can be used to tailor treatments to the unique genetic and molecular profiles of each patient’s tumor.
Platelet concentrates are crucial for the treatment of severe thrombocytopenia, which is particularly common in onco-hematology. Currently, platelets are obtained exclusively from blood donations, but their short shelf life (5-7 days) leads to significant supply shortages, especially during health crises or vacation periods. To overcome these limitations, a method has been developed to obtain platelets from a genetically engineered megakaryocyte cell line derived from adult CD34+ hematopoietic cells using a modified rotating bioreactor [1]. CD34+ hematopoietic cells were isolated from G-CSF-mobilized peripheral blood of adult donors. These cells were transduced with over 40 different gene combinations driven by doxycycline. The cells were cultured in serum-free media for expansion and differentiated into megakaryocytes (MKs) in the absence of doxycycline. The derived megakaryocytes were analyzed by flow cytometry for key surface markers, including GPIIIa, GPIIb, GPIb and GPVI. CD34+ cells transduced with specific members of the homeobox gene family showed long-term culture viability (up to 4 months) and megakaryocytic differentiation potential. The megakaryocytes generated from the cell mass expressed GPIIIa+GPIb+ and GPVI+GPIIb+ markers and are polyploid. The platelet-like particles generated in the HemostOD bioreactor were intact and functional and showed GPIIIa+GPIb+CalceinAM+ expression and fibrinogen binding after activation with convulxin or thrombin.
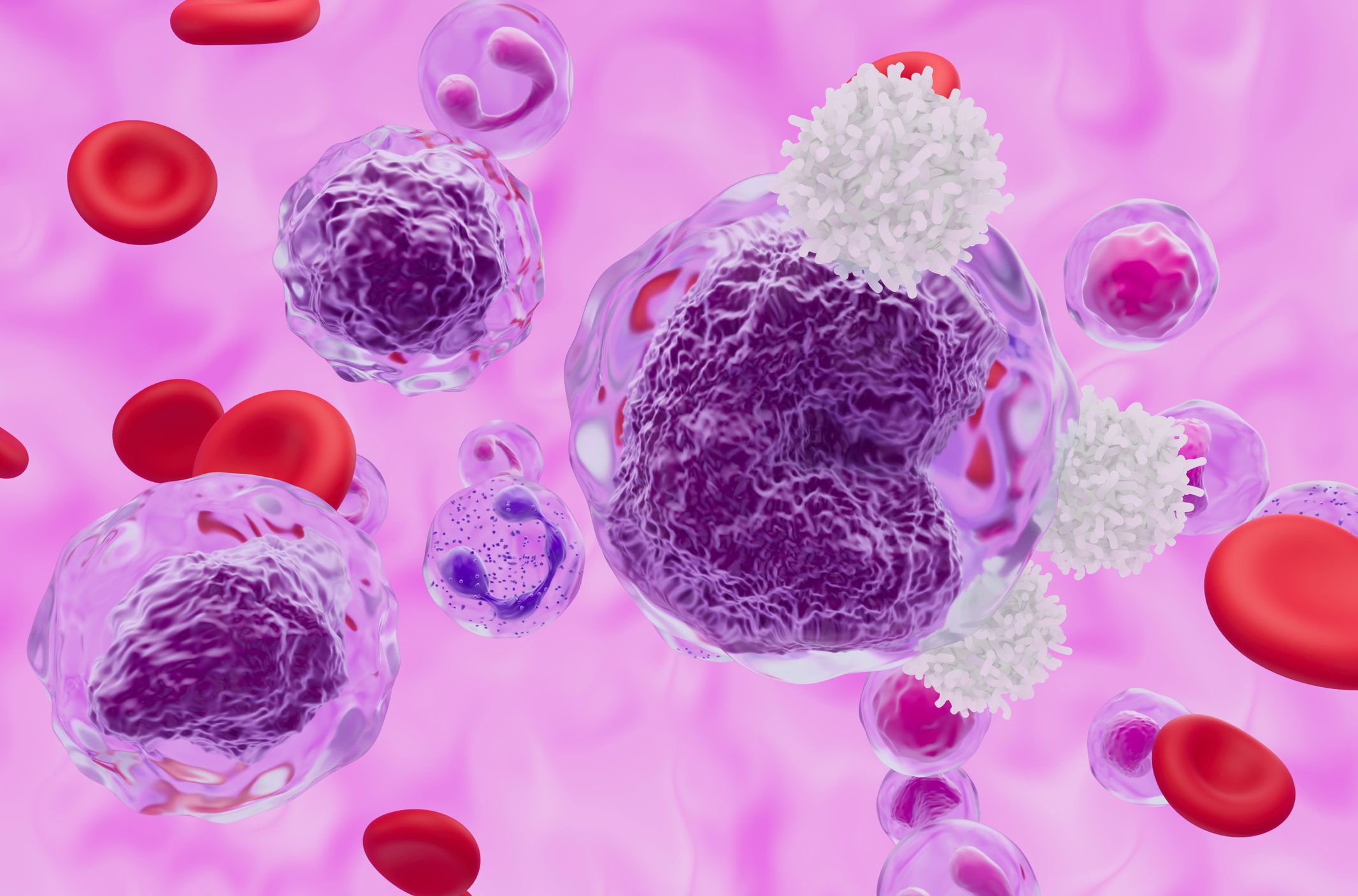
CAR-T cell therapy for AML
The development of chimeric antigen receptor (CAR) T cell therapy for AML has so far encountered difficulties. Recently, CD70 has emerged as an attractive target due to its differential expression in malignant and normal hematopoiesis, its obvious role in AML biology and its compelling safety profile. Accordingly, a rational approach was adopted to generate novel CD70 CARs with enhanced efficacy against AML [2]. To determine the optimal composition of the CAR structure, the extracellular domain of the natural ligand CD27 was paired with different hinge, transmembrane (TM) and endodomains and encoded into a third-generation lentiviral vector. Protein design calculations using physical and deep learning-based algorithms were performed to optimize the CD27-CD70 binding interface. CAR-T cells produced using a protocol compatible with good manufacturing practice were evaluated for cytotoxicity in a sequential killing assay in co-culture with CD70+ MOLM-13.GFP-ffLuc AML cells. In vivo anti-leukemic activity was assessed in a MOLM-13.GFP-ffLuc xenograft or a CD70low patient-derived xenograft model. Off-target screening of the final candidate was performed using Retrogenix Cell Microarray technology.
Of the four CAR assemblies tested, one showed robust killing of AML cells with significantly higher IFNγ and IL-2 production in vitro. At non-curative doses, the construct strongly suppressed leukemia growth and improved overall survival of mice in vivo. A total of 32 affinity-modulated variants with optimized binding interface were selected from computational designs and functionally tested. Two variants with better efficacy than the parental construct in were identified, accompanied by long-term persistence of functional CAR-T cells. An off-target screen of the most effective variant against 6500 human proteins showed no off-target interactions. The data show that it is possible to integrate computational protein design into CAR development to identify effective candidates and make better molecule selection for clinical translation.
Older patients with non-Hodgkin’s lymphoma
As patients live longer and longer, the phenomenon of ageing poses a major challenge in the treatment of cancer. This is particularly true for patients with non-Hodgkin’s lymphoma (NHL), where the average age at diagnosis is around 70 years. A study examined the outcomes of older patients treated for NHL in the clinic [3]. It showed that a favorable toxicity profile in older patients treated for NHL is possible by adjusting the intensity of treatment. Such adjustment allows multiple lines of treatment regardless of age, but based on the CIRS-G score.
Congress: 7th Swiss Oncology and Hematology Congress (SOHC)
Literature:
- Humbert M, et al: Functional Platelet Generation from Engineered Megakaryocyte Cell Line Derived from Adult CD34+ Hematopoietic Cells Using a Modified Rotating Bed Bioreactor. Abstract 377.7th Swiss Oncology and Hematology Congress (SOHC), November 20-22, 2024.
- Que T, et al: Potency tuned novel CD70 CAR-T Cells with a computationally designed CD27: CD70 binding interface for acute myeloid leukemia. Abstract 442.7th Swiss Oncology and Hematology Congress (SOHC), November 20-22, 2024.
- Nasrinfar K, et al: Older patients with non-Hodgkin lymphoma receive as much treatment lines as younger ones through adjustment, in a real life setting. Abstract 395.7th Swiss Oncology and Hematology Congress (SOHC), November 20-22, 2024.
InFo ONKOLOGIE & HÄMATOLOGIE 2024; 12(6): 20 (published on 11.12.24, ahead of print)