Protein electrophoresis is an inexpensive and widely available laboratory test and examines specific proteins in the blood. In internal medicine, it is mainly used to diagnose suspected multiple myeloma. The following article shows why it is also useful in gastroenterology.
In protein electrophoresis, the serum (i.e., the liquid portions of the blood when the cellular components are separated from a coagulated blood sample by centrifugation) is placed on a special pad, treated with a gel, and subjected to an electrical charge. Based on the different physical properties (size, electrical charge) of serum proteins, they are classified into five main classes (Fig. 1a) [1]:
Albumin
- Alpha-1 globulins (α1)
- Alpha-2-globulins (α2)
- Beta globulins (β)
- Gamma globulins (γ)

Protein electrophoresis is mainly used to diagnose suspected multiple myeloma, but it is also very useful as a screening test for many other diseases in internal medicine and especially in gastroenterology, which we would like to discuss in a little more detail in this article.
Components of protein electrophoresis
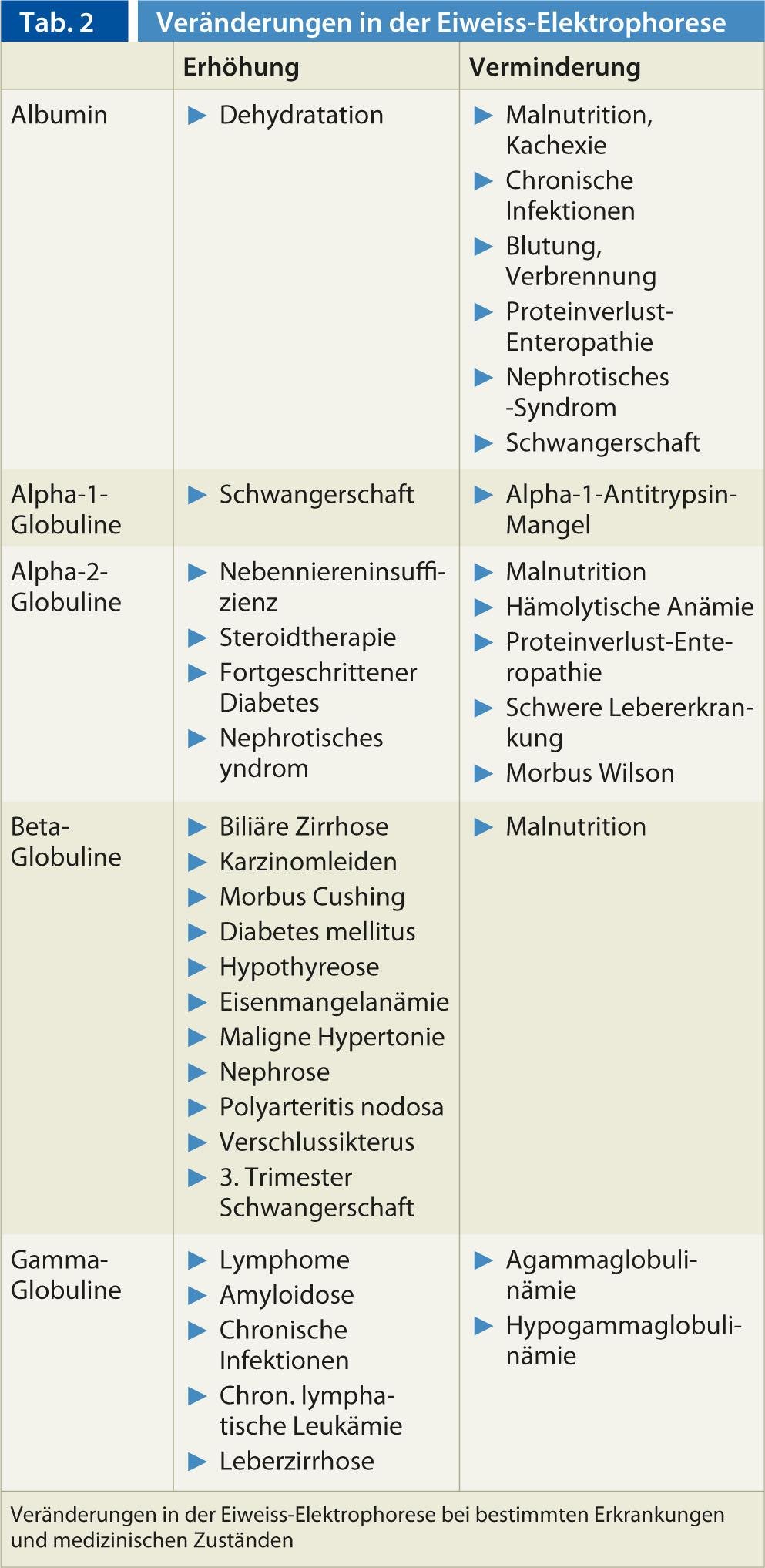
Basically, two main types of proteins can be distinguished: Albumin and globulins, which are present in the serum according to a specific distribution pattern (Tab. 1) . Certain medical conditions and diseases lead to a characteristic electrophoretic pattern (Tab. 2) [2]. The various components of protein electrophoresis are discussed in a little more detail below.
Albumin: Albumin is produced in the liver and is the major component of proteins in serum. It represents the highest peak in protein electrophoresis and is closest to the positive electrode (anode). Albumin is decreased in situations of reduced production in the liver or increased loss or degradation. An albumin drop of at least 30% is necessary for it to be visible in protein electrophoresis. Important examples of decreased albumin levels include malnutrition, severe liver disease, renal loss (e.g., nephrotic syndrome), hormone therapy, burns, or pregnancy. Increased albumin levels may be observed in patients with dehydration.
Globulins: The globulins group comprises a significantly smaller fraction of the total proteins in serum. As described earlier, this group includes the four subgroups alpha-1, alpha-2, beta and gamma. The tips of the globulins are closer to the negative electrode (cathode) than the albumin, with the gamma fraction closest to the cathode.
Albumin-alpha-1 intermediate zone: In this zone of protein electrophoresis, the alpha-1 lipoprotein (high density lipoprotein-LDL) is imaged. Decreases occur in severe inflammatory conditions, acute hepatitis, cirrhosis of the liver, or nephrotic syndrome. An increase is found in severe alcoholics, in pregnant women or during puberty.
Alpha-1 zone: the alpha-1 fraction consists of alpha-1 antitrypsin, alpha-1 glycoprotein, thyroxide-binding globulin, and transcortin. A decrease in this fraction is seen, for example, in alpha-1 antitrypsin deficiency, nephrotic syndrome, or decreased globulin production in severe liver disease. Neoplasia and acute inflammatory conditions can lead to an increase in alpha-1 globulins.
Alpha-2 zone: coeruloplasmin, alpha-2 macroglobulin and haptoglobin belong to the fraction of alpha-2 globulins. Typically, a decrease in the alpha-2 zone is seen in hemolytic anemias (consumption of haptoglobin, which binds to hemoglobin) or Wilson’s disease (decreased coeruloplasmin). Increased alpha-2 fraction is seen in patients with a nephrotic syndrome (alpha-2 macroglobulin is a large molecule that cannot pass through the glomeruli) or in inflammatory conditions (in terms of an acute phase reaction).
Beta fraction: The beta fraction consists of transferrin, complement factor C3, beta lipoprotein and the immunoglobulins IgA and (partially) IgM. Elevation is found in iron deficiency anemia, pregnancy, or in patients undergoing estrogen therapy, among other conditions.
Gamma fraction: The gamma region consists predominantly of the immunoglobulins (mostly IgG), although the various immunoglobulin classes (IgG, IgA, IgM, IgD and IgE) are also partially represented in the beta and alpha-2 regions. The zone of gamma globulins is decreased in hypo- or agammaglobulinemia. Diseases with increased production of gamma globulins include malignant lymphomas (including multiple myeloma and Waldenström’s disease), amyloidosis, chronic lymphocytic leukemia, skin diseases, rheumatologic diseases (e.g., rheumatoid arthritis or systemic lupus erythematosus), granulomatous diseases, or liver cirrhosis.
Main indications in internal medicine
Protein electrophoresis (with immunofixation, which is more sensitive in detecting the small monoclonal M protein or paraprotein) should be performed in all patients with suspected multiple myeloma, Waldenström disease, or suspected amyloidosis. These diseases belong to the group of monoclonal gammopathies, which are distinguished from polyclonal gammopathies (Table 3) [3]. The monoclonal gammopathies are a group of diseases characterized by the proliferation of a single clone of plasma cells. These produce an immunologically homogeneous protein called paraprotein or M protein (M stands for monoclonal).
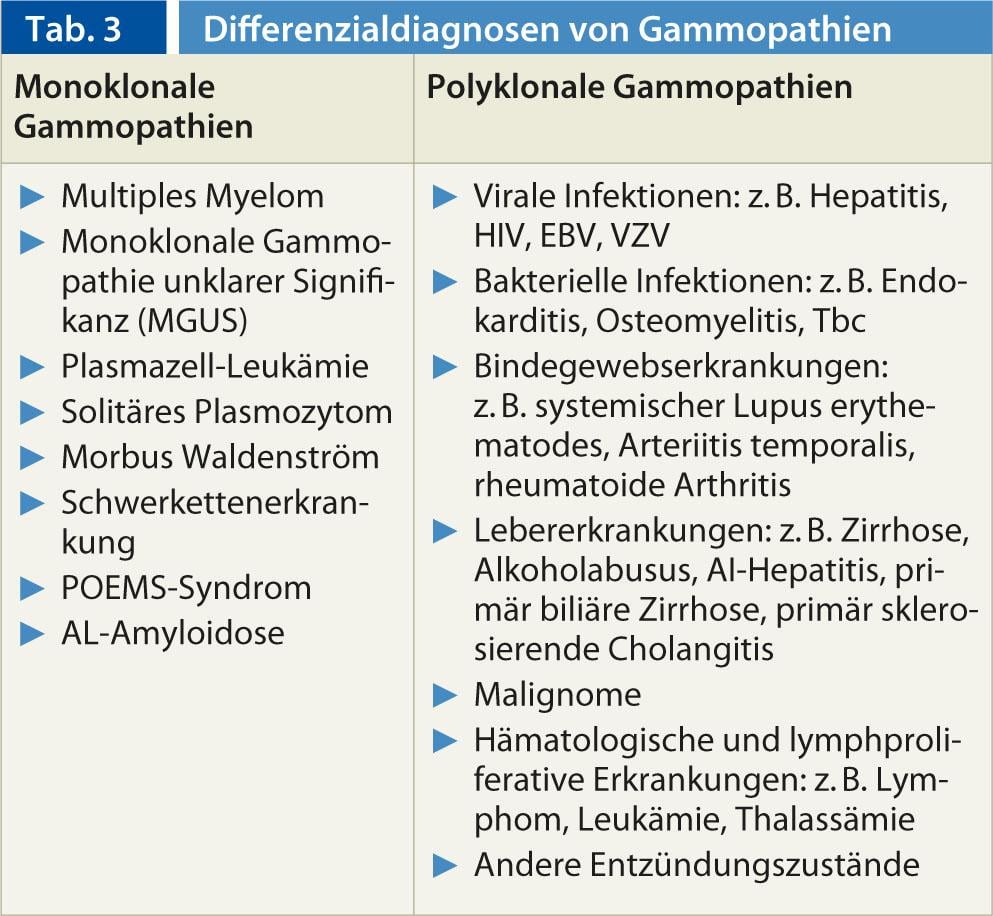
In contrast, no M protein can be detected in polyclonal gammopathies. Polyclonal gammopathies are often caused by reactive or inflammatory processes.
Indications in gastroenterology
Protein electrophoresis is mainly used in gastroenterology for the clarification of unclear hepatopathies. In liver disease, albumin is typically decreased, alpha-2 globulins may be decreased, and the gamma fraction is often polyclonal (Fig. 1b). Rarer causes of hepatopathy, such as autoimmune hepatitis, alpha-1 antitrypsin deficiency (Fig. 1c), or Wilson disease, can be excluded rapidly and inexpensively with normal protein electrophoresis.
However, patients with amyloidosis, multiple myeloma, or Waldenström’s disease also present relatively frequently with gastrointestinal symptoms [4, 5]. In cases of unclear gastrointestinal symptoms, the indication for protein electrophoresis should therefore be generous, especially if the patients also complain of general symptoms such as weight loss or fever.
Interpretation of results of protein electrophoresis
Early phase of acute inflammation (Fig. 1d): This image may be seen in acute infection, trauma, necrosis formation (e.g., myocardial infarction), or burns. Elevated levels of fibrinogen, alpha-1-antitrypsin, haptoglobin, coeruloplasmin, CRP, complement C3, and alpha-1-acid glycoprotein are seen.
Albumin normal-↓, alpha-1↑, alpha-2↓, gamma normal
Late phase of inflammation (Fig. 1e): This picture is seen in the late phase of infections. Conspicuous compared to the early phase of inflammation are the decreased albumin and increased gamma globulins.
Albumin↓ alpha-1↑, alpha-2↓, gamma↑
Chronic (active) inflammation: These conditions include viral diseases (e.g., hepatitides, mononucleosis, tuberculosis), rheumatologic diseases, or inflammatory bowel disease.
Chronic active inflammation (Fig. 1f):
Albumin↓, alpha-1↑, alpha-2↑, beta normal, gamma↑
Chronic inflammation (Fig. 1g):
Albumin↓, alpha-1, alpha-2 and beta normal, gamma↑
Malignant tumors: All malignant tumors show an increase in alpha-globulins (especially alpha-2) in the sense of an acute phase reaction. Tumors with immunosuppressive properties (lymphomas) can lead to a decrease in the gamma fraction.
Albumin↓, alpha-1 and alpha-2↑, beta normal,
gamma normal, ↓ or ↑
Autoimmune hepatitis: In addition to signs of chronic hepatopathy (decreased albumin and often low alpha fraction), autoimmune hepatitis shows a marked increase in gamma fraction.
Albumin↓, alpha-1 and alpha-2 normal or↓ , beta normal, gamma ↑ ↑ ↑
Nephrotic syndrome (Fig. 1h): Renal disease with glomerular damage and urinary protein loss of at least 3 g/day can lead to this pattern. The alpha-2 fraction can sometimes be very pronounced and look similar to a monoclonal gammopathy with an M gradient.
Albumin↓, alpha-1↓, alpha-2↑ ↑, beta↑, gamma↓
Antibody deficiency (Fig. 1i) : Antibody deficiency states can affect either a single fraction or all fractions. Congenital antibody deficiency syndrome presents with multiple infections already during childhood. Acquired antibody deficiency may be caused by drugs (e.g., cytostatics or prednisone), chronic lymphocytic leukemia, multiple myeloma, malignant tumors, or nephropathy.
Albumin, alpha-1, alpha-2 and beta normal, gamma↓
pregnancy (Fig. 1j): In the first trimester, alpha-2 globulins increase and in the second as well as third trimester additionally the beta fraction (due to iron deficiency anemia).
Albumin↓, alpha-1 normal, alpha-2 and beta↑,
gamma normal
CONCLUSION FOR PRACTICE
- Protein electrophoresis is an inexpensive and readily available laboratory test that can quickly identify or rule out certain diseases.
- In protein electrophoresis, proteins are separated based on different physical properties, resulting in a specific pattern. This pattern indicates a specific disease (e.g., multiple myeloma) or medical condition (e.g., acute inflammation).
- Typically, protein electrophoresis is used in internal medicine to identify patients with multiple myeloma or other monoclonal gammopathy
- In gastroenterology, protein electrophoresis can provide important clues to the presence of hepatopathy or other underlying disease manifesting in the gastrointestinal tract.
Literature:
- O’Connell TX, Horita TJ, Kasravi B: Understanding and interpreting serum protein electrophoresis. Am Fam Physician 2005; 71: 105-112.
- Kyle RA: The monoclonal gammopathies. Clin Chem 1994 ; 40: 2154-2161.
- Dispenzieri A, Gertz MA, Therneau TM, Kyle RA: Retrospective cohort study of 148 patients with polyclonal gammopathy. Mayo Clin Proc 2001; 76: 476-487.
- Kyle RA, Grepp PR : Amyloidosis (AL): clinical and laboratory features in 229 cases. Mayo Clin Proc 1983; 58: 665-683.
- Bohus R, et al: Retroperitoneal haemorrhage with abscess formation complicating Waldenström’s macroglobulinemia. Int Urol Nephrol 1985; 17: 255-259.