ALPPS, a new two-step hepatectomy, proved to be a good alternative to the classical methods of portal vein embolization and portal vein ligation in several small studies. The results show rapid and extensive hypertrophy of the liver. Liver tumors previously considered uncurable benefit most from the surgical technique. This article provides an overview of recent study results and discusses the practical relevance of the innovative method.
In 1897, the Scottish surgeon and pathologist James Cantlie discovered that after injury to the right portal vein, the left lobe of the liver was greatly enlarged. This observation led him to speculate that by occluding the portal vein on one side of the liver, the opposite lobe of the liver could be made to grow [1]. It took 80 years for Japanese surgeons to realize this vision and show that therapeutic embolization of the right portal vein can lead to growth of the left hemisphere of the liver before liver resection [2].
Portal vein embolization and portal vein ligation
Nowadays, portal vein embolization (PVE) is a well-established component of modern liver surgery to resect large or multifocal tumors with small liver remnants [3]. In most cases, the right portal vein and the portal vein branch in segment four are occluded with microparticles by interventional radiologists after transcutaneous puncture of the portal vein. After that, the left lobe of the liver grows. When it has reached a sufficient volume, usually after four to eight weeks, the embolized portion of the liver can be resected (Fig. 1).
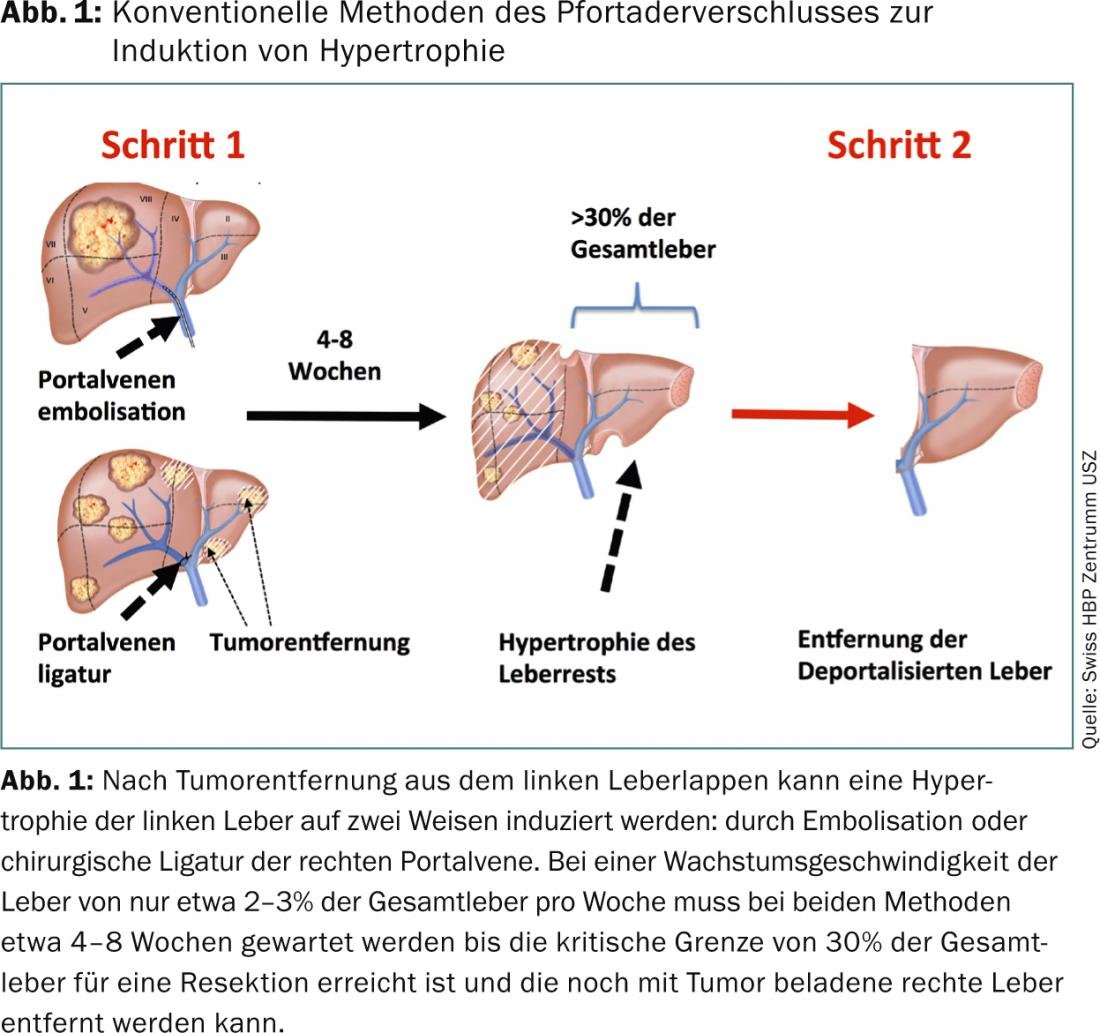
Another method of portal vein occlusion is portal vein ligation (PVL) by the surgeon [4]. To date, no difference in growth between interventional embolization and surgical ligation has been detected [5]. However, because embolization is less invasive, it is usually preferred. In multifocal tumors, on the other hand, two operations are usually performed in succession. This is especially the case when the patient first needs a “clean-up” of the hypertrophic flap before it is stimulated to grow. In these two-step liver resections, portal vein ligation is now frequently used in the first step to enlarge the liver remnant [6].
The waiting time required for patients to progress to complete resection after portal vein embolization and portal vein ligation depends on three factors: (1) the starting volume, (2) the rate of liver tissue growth, and (3) the volume needed to progress to final resection.
In most centers, a minimum residual liver volume of 30% is required as a lower limit for liver resections [7], and in this sense, 30% is also considered the target volume after volume manipulation [6]. In a meta-analysis of publications on portal vein embolization, the mean growth after embolization was reported to be 40% of total liver volume in four weeks [3]. The most important factor for growth velocity is probably the quality of the liver parenchyma, as studies have shown that cirrhotic livers, for example, grow less rapidly [3]. Furthermore, the smaller the initial volume, the longer the waiting time for resection.
In some cases with extremely small initial volumes or cirrhotic livers, the target volume of 30% is not reached and consequently the second step cannot be performed. A long wait can also cause the tumor to recur and the original plan to get the patient completely tumor-free has to be abandoned. Chemotherapy is then re-initiated and the plan to treat the patient curatively is changed back to a palliative strategy. Previously published work on portal vein embolization and posterior vein ligation demonstrates that approximately 30% of patients do not progress to definitive resection.
ALPPS
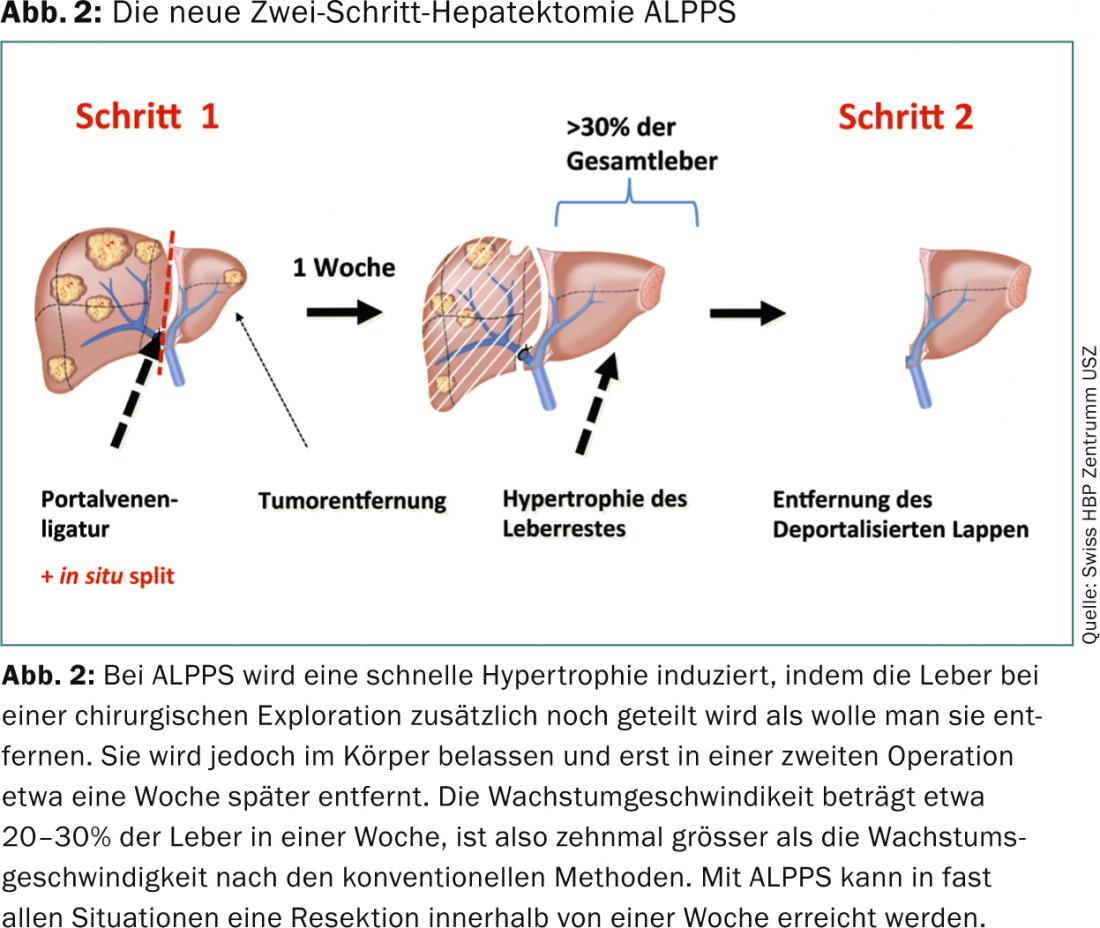
In 2012, a series of 25 liver resections from five German centers was published in the Annals of Surgery, presenting a new technique of liver hypertrophy with which a faster and larger volume increase of the residual liver is possible [8]. The authors from Germany transsected the liver parenchyma as if they were removing the right liver, but left it in place and additionally ligated the portal vein on the right side (Fig. 2). In this way, they induced a growth of 21-192% within nine days. This is a growth rate previously observed only after liver resection, and is approximately ten times higher than that previously achieved with PVE and PVL [9].
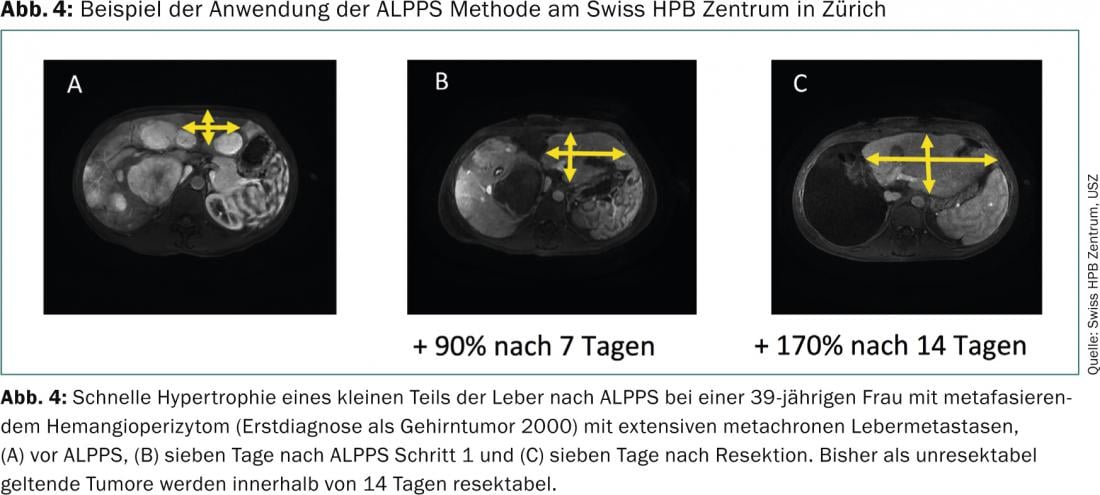
The new operation was given the eponym ALPPS (Associating Liver Partition with Portal Vein ligation for Staged hepatectomy) in an editorial in the Annals of Surgery [10]. The initial series reported 24 cases of extended resections of the right lobe of the liver, right trisectionectomies, and four cases of multifocal metastases in both lobes of the liver that required cleanup of the left lobe before hypertrophy induction [8]. All patients achieved resection. Other series reported 15 patients from Buenos Aires with a volume increase of 78% in one week [11], seven patients at Uniklink Düsseldorf with a volume increase of 63% within three days [12], and nine patients at Uniklinik Tübingen with a median volume increase of 87% after 13 days [13]. In Zurich, we evaluated the results of 18 patients with ALPPS at the Swiss HPB Center together with 30 additional patients from other international centers [9].
Results with ALPPS
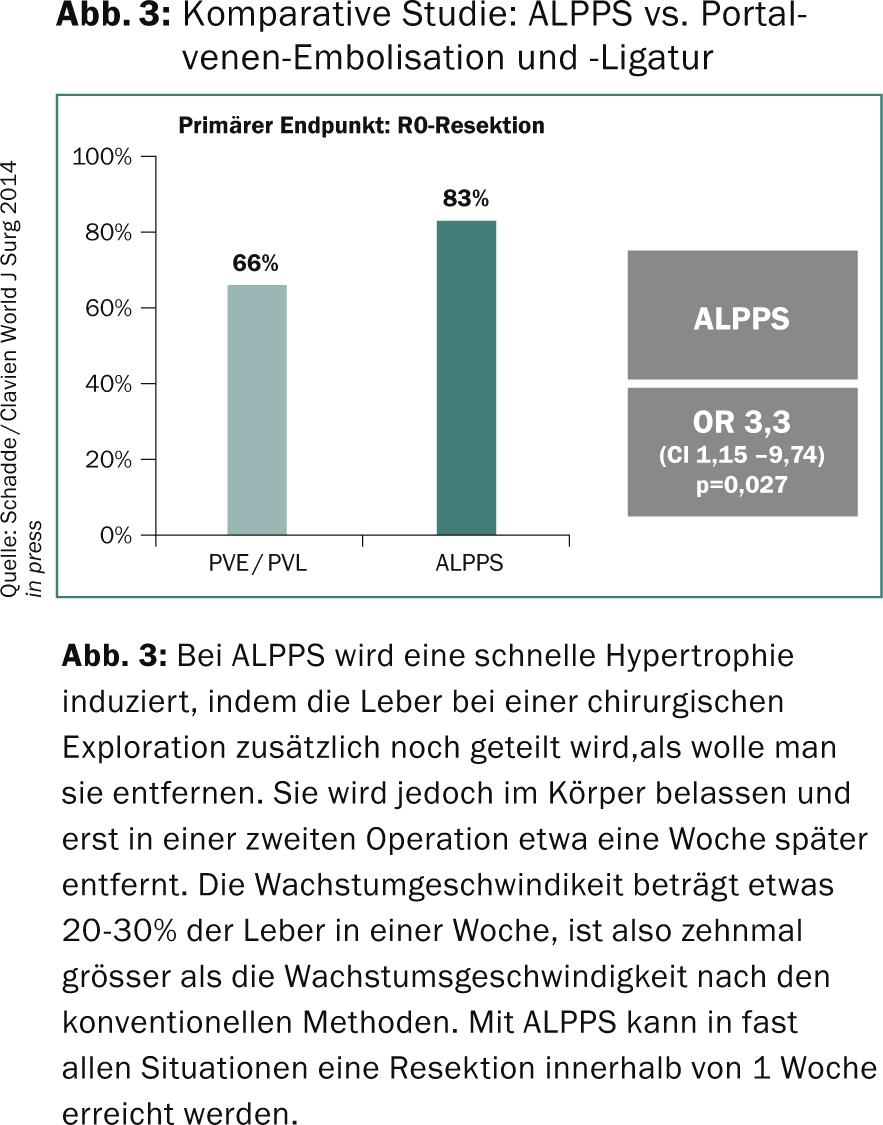
In agreement, the authors describe that in all cases complete resection could be performed at the end of the growth process and in none of the cases the tumor proved to be unresectable at the second step, probably due to the short interval between the first and second step. Schnitzbauer et al. reported that R0 resection was achieved in 100% of cases. 5/25 of patients had tumor recurrence within 180 days, but this was not very meaningful because of the mixed tumor etiology. Alvarez et al. reported 100% R0 resections with a follow-up of 188 days and 27% (4/15) recurrences. Knoefel et al. showed a 100 percent R0 resection without tumor recurrence in their results. We therefore performed a comparative study between ALPPS and conventional methods in Zurich to test whether ALPPS or the conventional methods PVE and PVL are more able to achieve complete tumor resection. We chose three months as the short-term end point, because at these time points either complete surgical resection should or should not be possible for large or multifocal liver tumors.
We pooled the experience with ALPPS and the conventional methods PVE and PVL in four international centers and found that complete tumor resection was achievable in 83% of cases with ALPPS and only in 66% of cases with PVE/VPL (Fig.3). We also showed that despite this short-term success, there was no higher recurrence rate with ALPPS than with PVE and PVL [9]. We therefore consider the prerequisites for a multicenter randomized trial to be given and have initiated such a study(www.alpps.net).
In parallel, we have established an international case registry in collaboration with Buenos Aires in Zurich (ALPPS REGISTRY[www.alpps.net]) in which more than 250 cases from 56 centers worldwide have been registered to date. An initial evaluation has shown a recurrence-free survival of 41% at two years for patients after ALPPS for colorectal metastases. A good result when compared with other series of two-step surgery for colorectal cancer [14].
The perioperative complications and mortality of ALPPS prompted discussion. The initial study showed perioperative mortality in 12% (3/25) of cases. Other studies reported no mortality in a population of 15 patients [11], another likewise reported no deaths among a total of seven patients [12]. Li et al. recorded two deaths among a total of nine patients [13]. It appears that the cause of most mortalities occurred in the context of sepsis and biliary leakage. Because the numbers in these series are too small to draw clear conclusions, we examined the worldwide mortality of 202 patients in 41 centers in the ALPPS REGISTRY with complete follow-up and found a 90-day mortality of in 9%, or 19 of 202 patients in total. It appears that this figure is within the range that can be expected for extended and complex hepatectomies [15]. The 90-day mortality of ALLPS REGISTRY patients under 60 years of age with colorectal metastases is only 5.1%, which is well within the range of what international series report for two-step surgery [14]. Because the data are currently insufficient to draw reliable conclusions despite all efforts, a comparative analysis of the perioperative risks of ALPPS versus conventional methods of inducing hypertrophy using PVE and PVL should probably be left to a randomized trial.
Summary
ALPPS is a new two-step hepatectomy that results in rapid and extensive hypertrophy of the liver. This will allow resection of liver tumors that are either unresectable in one step or at high risk of recurrence during the waiting period with other methods of inducing hypertrophy. Although the rapid hypertrophy caused by ALPPS has not yet been explained physiologically, it is a reproducible phenomenon and the operation allows resection of liver tumors previously considered unresectable because of their extension. Randomized trials should clarify the value of this innovation in oncologic liver surgery in the future.
Supported by:
- University of Zurich (Clinical Research Focus: Non-resectable Liver Tumors)
- Liver and Gastro-intestinal Foundation (LGID) Swiss HPB Centre, Zurich
Literature:
- van Gulik TM, van den Esschert JW: James Cantlie’s early messages for hepatic surgeons: how the concept of pre-operative portal vein occlusion was defined. HPB (Oxford) 2010; 12(2): 81-83.
- Kinoshita H, et al: Preoperative portal vein embolization for hepatocellular carcinoma. World J Surg 1986; 10(5): 803-808.
- van Lienden KP, et al: Portal Vein Embolization Before Liver Resection: A Systematic Review. Cardiovasc Intervent Radiol 2012.
- Kianmanesh R, et al: Right portal vein ligation: a new planned two-step all-surgical approach for complete resection of primary gastrointestinal tumors with multiple bilateral liver metastases. J Am Coll Surg 2003; 197(1): 164-170.
- Aussilhou B, et al: Right portal vein ligation is as efficient as portal vein embolization to induce hypertrophy of the left liver remnant. J Gastrointest Surg 2008; 12(2): 297-303.
- Clavien PA, et al. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 2007; 356(15): 1545-1559.
- Breitenstein S, et al: “State of the art” in liver resection and living donor liver transplantation: a worldwide survey of 100 liver centers. World J Surg 2009; 33(4): 797-803.
- Schnitzbauer AA, et al: Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 2012; 255(3): 405-414.
- Schadde E, et al: ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumours. Results of a Multicentre Analysis. World J Surg 2014; in press.
- de Santibanes E, Clavien PA: Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 2012; 255(3): 415-417.
- Alvarez FA, et al: Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg 2013; 17(4): 814-821.
- Knoefel WT, et al: In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 2013;100: 388-394.
- Li J, et al: ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure? J Gastrointest Surg 2013; 17(5): 956-961.
- Brouquet A, et al: High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol 2011; 29(8): 1083-1090.
- Lang H, et al: Left hepatic trisectionectomy for hepatobiliary malignancies. J Am Coll Surg 2006; 203(3): 311-321.
InFo Oncology & Hematology 2014; 2(3): 20-23.











