Retroperitoneal fibrosis (RPF) is a rare chronic inflammatory fibrosing disease of the posterior abdominal cavity. The CT or MRI abdomen shows a flat mass surrounding the large vessels and the ureter.
The previous articles on abdominal pain symptoms have largely dealt with urological diseases. Today’s article follows on from this, whereby the symptoms are not primarily based on a urological disease, but are the result of a compressive proliferation of connective tissue in the retroperitoneal space: retroperitoneal fibrosis (RPF), also known as Ormond’s disease. It is a less common condition with an incidence of around 1:200,000, with men being affected more frequently than women. The initial manifestation primarily affects the middle years of life [2]. The pathomechanism has not been clarified. Primary RPF often occurs in autoimmune diseases, e.g. with IgG4-associated cholangitis. Secondary forms can be caused by trauma, radiation or medication (vasoactive, analgesics). The association with aortic sclerosis or (inflammatory) aortic aneurysm has been described [1,3,4].
Overview 1 lists the organs affected by possible compression.
The symptoms are recruited from the organ alterations (Overview 2).
The first person to describe RPF was the Cuban urologist J. Albarrán. The publication of the American urologist Ormond made the disease known in 1948 [1].
The diagnosis is primarily made by imaging, but also by laboratory chemistry with determination of inflammation parameters, autoantibodies and rheumatoid factors.
Drug therapy includes the use of corticosteroids, also in combination with anti-oestrogens, or cytostatics such as methotrexate or azathioprine. If conservative treatment is unsuccessful, a decompressive surgical reduction of the fibrous proliferation, stent implantation, surgical displacement of the ureters or creation of a urostoma is indicated.
Other renal diseases, other retroperitoneal tumors, arteriosclerotic vascular occlusions and gynecological diseases should be excluded in the differential diagnosis.
X-ray examinations are no longer relevant in the imaging diagnosis of retroperitoneal fibrosis. In the age of excretory urography, stenosis or obstruction of the ureters could be visualized.
Sonography can detect the retroperitoneal mass under good acoustic conditions, as well as the congested hollow system of the kidneys.
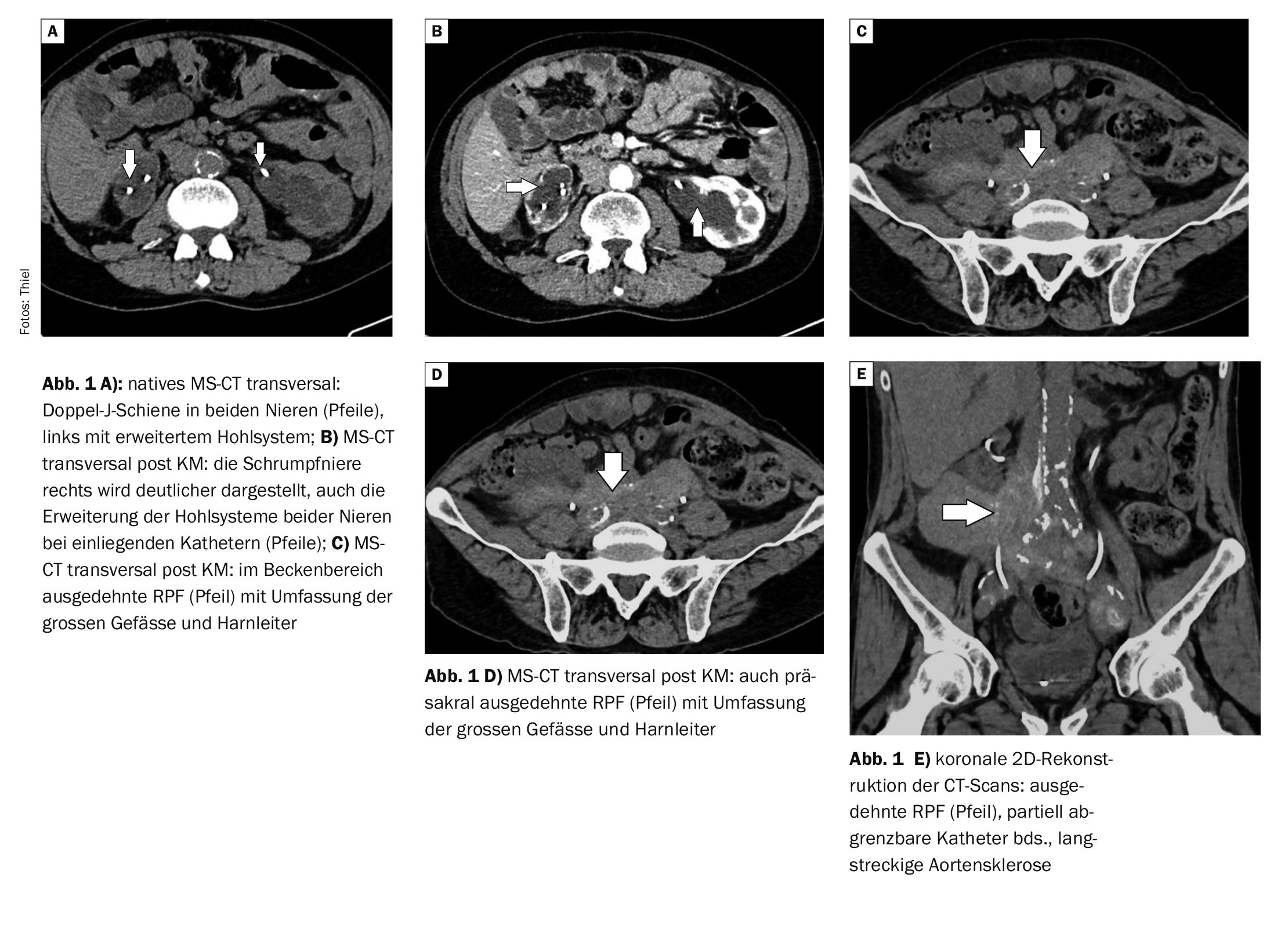
Computed tomography as a cross-sectional imaging procedure with native scans and also after contrast medium administration is the common imaging procedure for the detection of RPF and its possible complications [2]. A CT-guided biopsy can also be performed for tissue clarification of the mass [3].
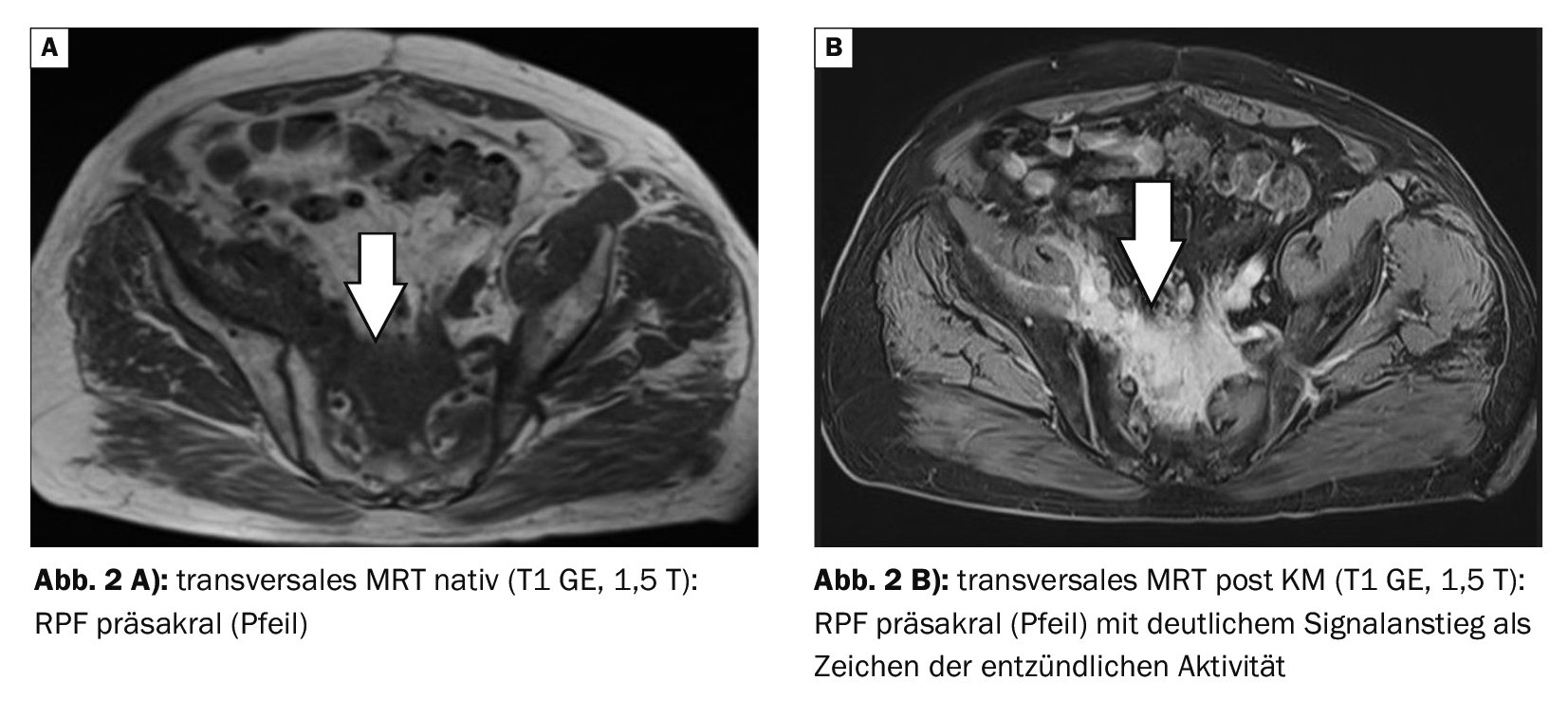
Magnetic resonance imaging is also very good at visualizing the RPF [2]. The contrast-enhanced sequences can detect the inflammatory activity of fibrous tissue proliferation very well.
Case study
In case example 1 (Fig. 1A to 1E) , a 71-year-old patient has an extensive RPF that is dominantly expansive to the right on abdominal computed tomography. Shrunken kidney on the right, the renal function values were pathologically altered (creatinine increased above 2, GFR decreased to 33). Double J-rails were inserted on both sides. The patient complained of flank pain on both sides.
Case 2 demonstrates (Fig. 2A and 2B) Ormond’s disease, extending prevertebrally at the level of the lower lumbar spine to presacral with clear inflammatory activity on contrast-enhanced MRI. Laboratory chemistry showed an increase in creatinine levels with a persistent increase in erythrocyte sedimentation rate and CRP. New onset of leg edema on both sides without evidence of cardiac insufficiency.
Take-Home-Messages
- Ormond’s disease is an inflammatory proliferative retroperitoneal fibrosis of as yet unknown cause.
- Men in the middle years of life are affected more frequently than women.
- This can lead to compression of the ureters, retroperitoneal vessels and adjacent organs.
- If primary drug treatment fails, surgical measures are used.
- In addition to laboratory diagnostics, imaging, primarily with CT or MRI, provides further diagnostic information.
Literature:
- “Retroperitoneal fibrosis”, https://de.wikipedia.org/wiki/Retroperitonealfibrose,(last accessed 18.12.2023)
- “Retroperitoneal fibrosis”, https://flexikon.doccheck.com/de/Retroperitonealfibrose,(last accessed 18.12.2023)
- Nelius T, et al: Idiopathic retroperitoneal fibrosis (Ormond’s disease). Current Urol 2006; 37(4): 284-288.
- Vogt B, Meier P, Burnier M: Retroperitonel fibrosis, Ormond’s disease, periaortitis, …? TherUmsch 2008; 65(5): 265-268.
FAMILY PHYSICIAN PRACTICE 2024; 19(1): 46-47