Actinic keratosis is an intraepidermal neoplasia that can potentially develop into an invasive growing spinocellular carcinoma (SCC). The current study situation does not allow reliable risk stratification. With this in mind, experts recommend treating all actinic keratoses.
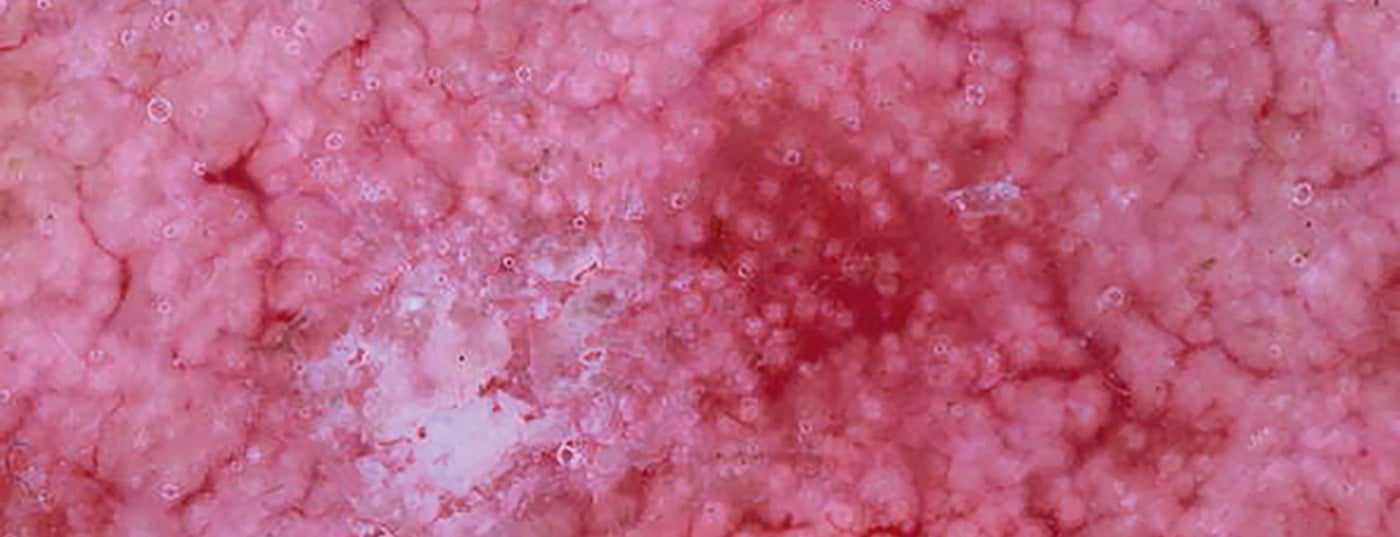
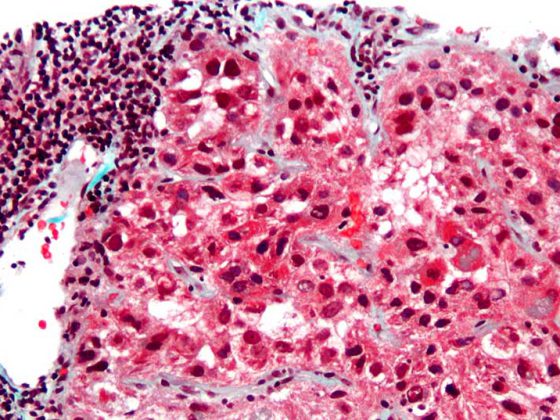
Actinic keratoses (AK) (Fig. 1) are among the most common dermatoses on chronically sun-damaged skin, especially in individuals with fair skin types. In European countries, the prevalence in those over 60 years of age is around 20-35% [1–3]. In recent decades, incidence rates have increased significantly. Clinical features of AK are erythematous and usually hyperkeratotic skin lesions at light-exposed body sites. The histomorphologic picture of AK ranges from the spectrum of merely actinically damaged skin with initial atypia of single keratinocytes to complete replacement of the localized epidermis by atypical keratinocytes, which is termed “carcinoma in situ” or, in the case of high-grade atypia and polymorphism of keratinocytes, “Bowen’s disease.”

Estimation of the risk of progression is difficult
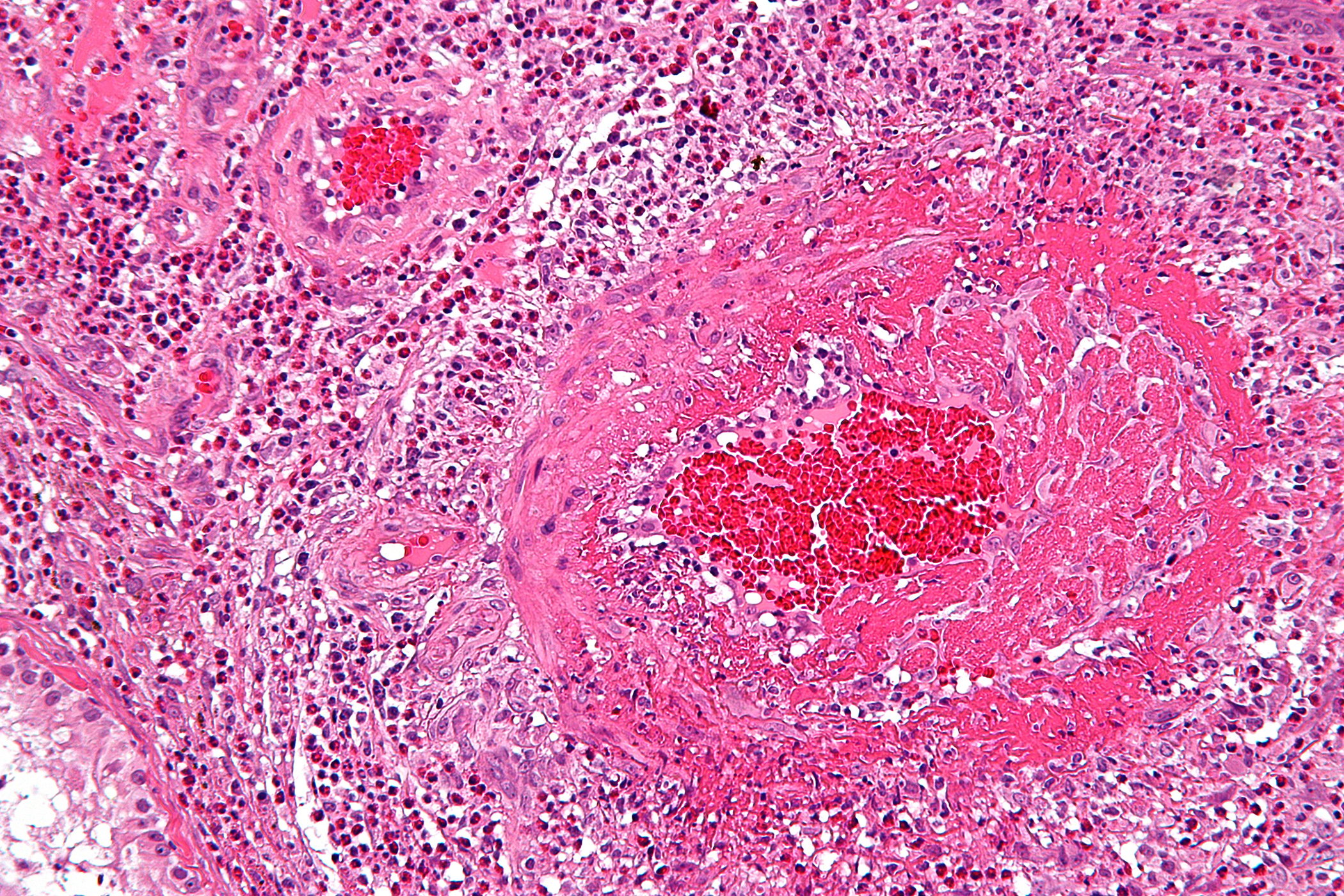
The mechanism of development of invasive SCC based on AK has been known for a long time. However, exact figures on the frequencies of this event are available only to a limited extent. Values reported in the literature for progression of AK to invasive SCC vary widely and have been quantified from 0.03% to 20% per lesion per year [4–6]. On the other hand, there are observations that about 60% of invasive SCC originate from an AK [5]. If an area affected by multiple AKs with evidence of field carcinogenesis (box) is present, there is evidence for a lower rate of spontaneous regression [8]. Recent studies on the pathogenesis of AK also suggest that transformation is possible even from early, i.e. clinically and histologically discrete lesions, and does not necessarily occur in a stepwise fashion via moderate and eventually hyperkeratotic AK [7].
In summary, then, it is difficult to predict which lesions will develop into squamous cell carcinoma. Squamous cell carcinoma of the skin (SCC) is the most common malignant skin tumor after basal cell carcinoma, and there has been a massive increase in age-standardized incidence numbers in recent decades. The highest incidence rates were reported in Wales, the Netherlands, and Switzerland (CH: 28.9/100,000 population in 2012) [9,10]. In Germany, about 21% of people over 65 years of age developed SCC in 2016. SCC can metastasize primarily to the regional lymph nodes and form distant metastases. The rate is up to 20% in individual subgroups. The presence of distant metastases of SCC is prognostically very unfavorable.
Literature:
- Ferrándiz C, et al; EPIQA Study Group, Prevalence of actinic keratosis among dermatology outpatients in Spain. Actas Dermosifiliogr 2016; 107(8): 674-680.
- Flohil SPC, et al: Prevalence of actinic keratosis and its risk factors in the general population: the Rotterdam Study. J Invest Dermatol 2013; 133(8): 1971-1978.
- Eder J, et al: Prevalence of actinic keratosis among dermatology outpatients in Austria. Br J Dermatol 2014; 171(6): 1415-1421.
- Criscione VD, et al: Actinic keratoses: natural history and risk of malignant transformation in the Veterans Affairs Topical Tretinoin Chemoprevention Trial. Cancer 2009; 115(11): 2523-2530.
- Marks R, et al: Malignant transformation of solar keratoses to squamous cell carcinoma. Lancet 1988; 1(8589): 795-797.
- Quaedvlieg PJ, et al: Actinic keratosis: how to differentiate the good from the bad ones? Eur J Dermatol 2006; 16(4): 335-339.
- Fernandez-Figueras MT, et al: Actinic keratosis with atypical basal cells (AK I) is the most common lesion associated with invasive squamous cell carcinoma of the skin. Journal of the European Academy of Dermatology and Venereology: JEADV 2015; 29(5): 991-997.
- Werner RN, et al: The natural history of actinic keratosis: a systematic review. Br J Dermatol 2013; 169(3): 502-518.
- Hollestein LM, et al: Trends of cutaneous squamous cell carcinoma in the Netherlands: Increased incidence rates, but stable relative survival and mortality 1989-2008. Eur J Cancer 2012; 48(13): 2046-2053.
- Xiang F, et al: Incidence of nonmelanoma skin cancer in relation to ambient UV radiation in white populations, 1978-2012: empirical relationships. JAMA Dermatol 2014; 150(10): 1063-1071.
- Balcere A: Dermatoscopy of Facial Non-Pigmented Actinic Keratosis and Intraepidermal Carcinoma, 2021, www.intechopen.com/chapters/77640, (last accessed Aug. 23, 2022).
- Figueras Nart I, et al: Progressing Evidence in AKWG. Defining the actinic keratosis field: a literature review and discussion. JEADV 2018; 32: 544-563.
- Heppt MV, et al: S3 guideline: actinic keratosis and squamous cell carcinoma of the skin. JDDG 2020; 18(3): 275-294.
DERMATOLOGY PRACTICE 2022; 32(4): 19