In clinical practice, besides mild forms, one is regularly confronted with three characteristic eczema situations: exacerbated (whole body) eczema, chronic (flexural/hand) eczema and nummular (superinfected) atopic eczema. All eczema situations require an individually adapted therapeutic strategy taking into account the following aspects: Use of anti-inflammatory preparations of sufficient potency, quantity and duration of application; use of (semi-)occlusive local therapy with special dressing/bandaging technique; regular cleansing of the skin by means of bath/shower (possibly with antiseptics), followed by moisturizing skin care; patient/parent training and instruction (if necessary, use of children’s Spitex). In atopic eczema, parents or treating physicians often have reservations about topical corticosteroid therapy. This and the often lacking knowledge of an efficient but safe eczema treatment in childhood often stand in the way of a successful therapy.
Every fifth to sixth child in Western civilization today is affected by atopic eczema. Peaks of disease are observed mainly at the age of five to six months, but also from two to three years. A (small) proportion of those affected experience a marked deterioration only at the beginning of school age. However, the symptoms are similar in the different age groups: recurrent inflammation of the skin with excruciating itching, scratching, chronicizing eczema sites, consecutive sleep disturbances and reduced quality of life of the affected child and his/her family. Although many children suffer only from a mild form of this eczema disease, we are regularly confronted with three characteristic, challenging eczema situations in everyday clinical practice:
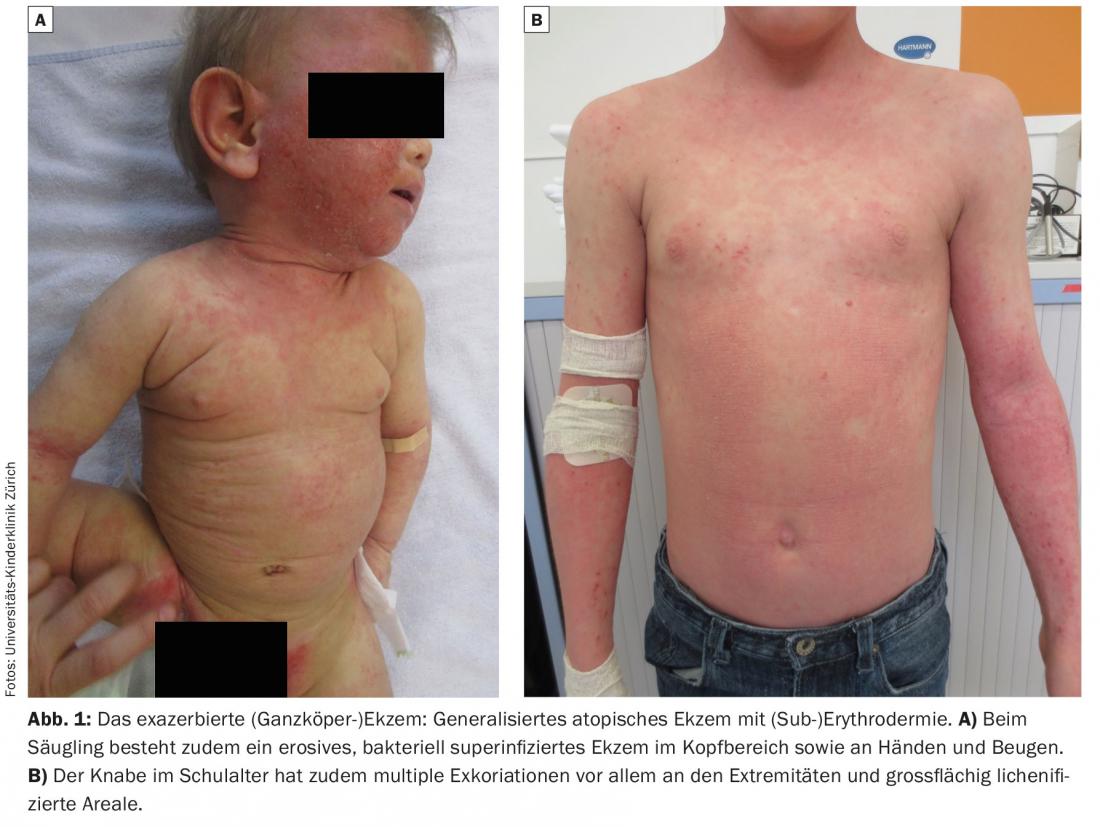
- Exacerbated (whole body) eczema: whole body infestation, erythroderma, bacterial superinfection, erosive-exacerbated eczema, face often severely affected. Typically infants and young children (Fig. 1).
- Chronic (flexural/hand) eczema: flexural and/or hand/foot eczema that does not heal completely or persistently despite therapy, accompanied by severe itching and scratching. Typically preschool and school age (Fig. 2).
- Nummular (superinfected) atopic eczema: with recurrent bacterial superinfection (S. aureus) and excoriations, often in combination with dyshidrotic erosive eczema of the hands and feet. Typically toddler to school age (Fig. 3).


The prevailing reservations about topical corticosteroid therapy in atopic eczema – whether on the part of the parents or the treating physicians – and the often lacking knowledge of an efficient but safe eczema treatment in childhood prevent a successful therapy and medium-term healing of the disease in these forms of manifestation. All eczema situations have in common that only an individually adapted therapy strategy taking into account the following aspects leads to a treatment success [1,2]:
- Use of anti-inflammatory preparations of sufficient potency, quantity and duration of application.
- Use of (semi-)occlusive local therapy with special dressing/bandaging technique
- Frequent cleansing of the skin by means of bath/shower (possibly with antiseptics), followed by moisturizing skin care
- Patient/parent training and instruction by skilled nursing staff, use of pediatric Spitex (Kispex) if necessary.
In the following, we summarize our therapy recommendations for the above three situations and describe the practical application of the techniques used in these situations. The mentioned brand names correspond to a subjective, limited selection – they can of course be replaced by equivalent other preparations.
Treatment methods
Bathing/showering: Regular skin cleansing by frequent (daily) lukewarm bathing – alternatively showering – from max. 10 min duration is of great importance. Bathing removes dandruff, crusts, ointment residues, irritants as well as allergens and thus counteracts unfavorable microbial colonization of the skin. Correct bathing moisturizes the skin and improves the penetration of emollients/topicals, if they are applied within max. be applied 10 minutes after the bath. This “soak and smear” technique also prevents increased transepidermal water loss, which is otherwise provoked by the evaporation of water on the skin [1–3]. Last but not least, bathing is also fun for many children and helps them fall asleep afterwards as a daily routine. If there is a tendency to bacterial superinfection, the use of an antiseptic skin-friendly wash lotion (e.g. Triclosan) or a so-called “bleach bath” – i.e. a diluted Javel water bath – once or twice a week is also advisable. We are having increasingly very good experience with diluted Javel water baths, analogous to American eczema experts; we have summarized instructions for practical application in a parent’s leaflet (available from the authors on request).
The Wet-Wrap-Therapy: The so-called Wet-Wrap-Therapy (WWT) is a treatment method, which brings a severe eczema – be it acute or chronic – quickly to healing. WWT is based on a decades-old tradition of various international treatment centers for infantile eczema. It has been used successfully on a regular basis at the Children’s Hospital Zurich since 2009. After bathing, a highly diluted topical corticosteroid is applied over a large area under moist tubular dressings (first layer moist, second layer dry) (Fig. 4). Numerous studies (including controlled ones) confirm the effectiveness and safety of WWT [1,4–6]. In addition to the corticosteroid, evaporization has an anti-inflammatory effect. The semi-occlusive application of the corticosteroid allows increased penetration into the skin, at the same time improving the hydration of the skin and preventing unfavorable scratching due to the mechanical barrier. Compared to peroral steroid shock therapy, there is no rebound effect after WWT and the systemic steroid effect is negligible if performed correctly (max. 14 days at a time) [5,6]. The use of the so-called Tubifast® Garments (Mölnlycke Health Care) in the form of size-adapted elastic cotton garments significantly simplifies therapy and facilitates compliance [5]. Occasionally, the cotton fabric on the wrists or ankles must be fixed with self-adhesive bandage for continuous covering of the skin. Depending on the eczema on the hands/fingers, these are included with the integrated mittens (up to 24 months) or with the additional Tubifast® gloves. If needed, thumbs or other fingertips can be cut free for daytime play.

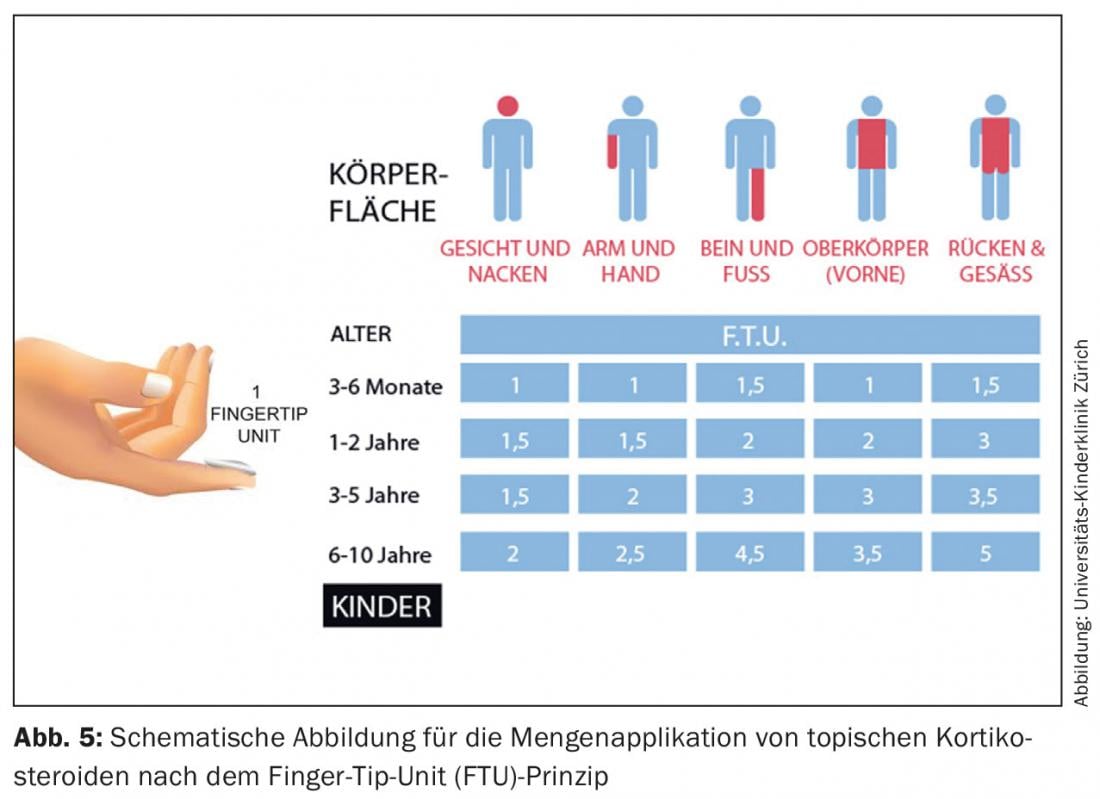
WWT can be performed on an outpatient basis with instruction from skilled nursing staff or on an inpatient basis. As a rule, WWT with prior bathing is applied once a day, but the moist dressing layer is additionally rewetted once or twice a day. In severe eczema cases we perform WWT (including application of topical corticosteroid) twice a day, including only once with bath. Proper implementation to avoid a systemic steroid effect includes the use of a 5-fold (or up to 10-fold in young infants) diluted potent class III corticosteroid. At the Children’s Hospital Zurich, we use Elocom® (mometasone) cream 1:5 in soft ointment KA, with a quantity application according to the finger-tip unit (FTU) principle (Fig. 5).
A possible complication under WWT is the occurrence of folliculitis (S. aureus), favored by the fat-moist semi-occlusive dressing therapy. In cases of severely superinfected eczema, oral antibiotic therapy (amoxicillin-clavulanic acid) starting two days prior to WWT has thus proven to be preemptive. However, mild folliculitis usually heals even with continued antiseptic and anti-inflammatory local therapy (with corticosteroids).
We usually perform WWT for a total of five to seven days and then switch to interval therapy of corticosteroid application (e.g., three days in a row per week) without moist double-layer dressings. However, the continued wearing of a dry Tubifast® garment layer at night (after application of the evening moisturizing care cream and/or topical steroid) for several weeks following WWT has proven to be effective and is experienced as comfortable by patients and families alike.
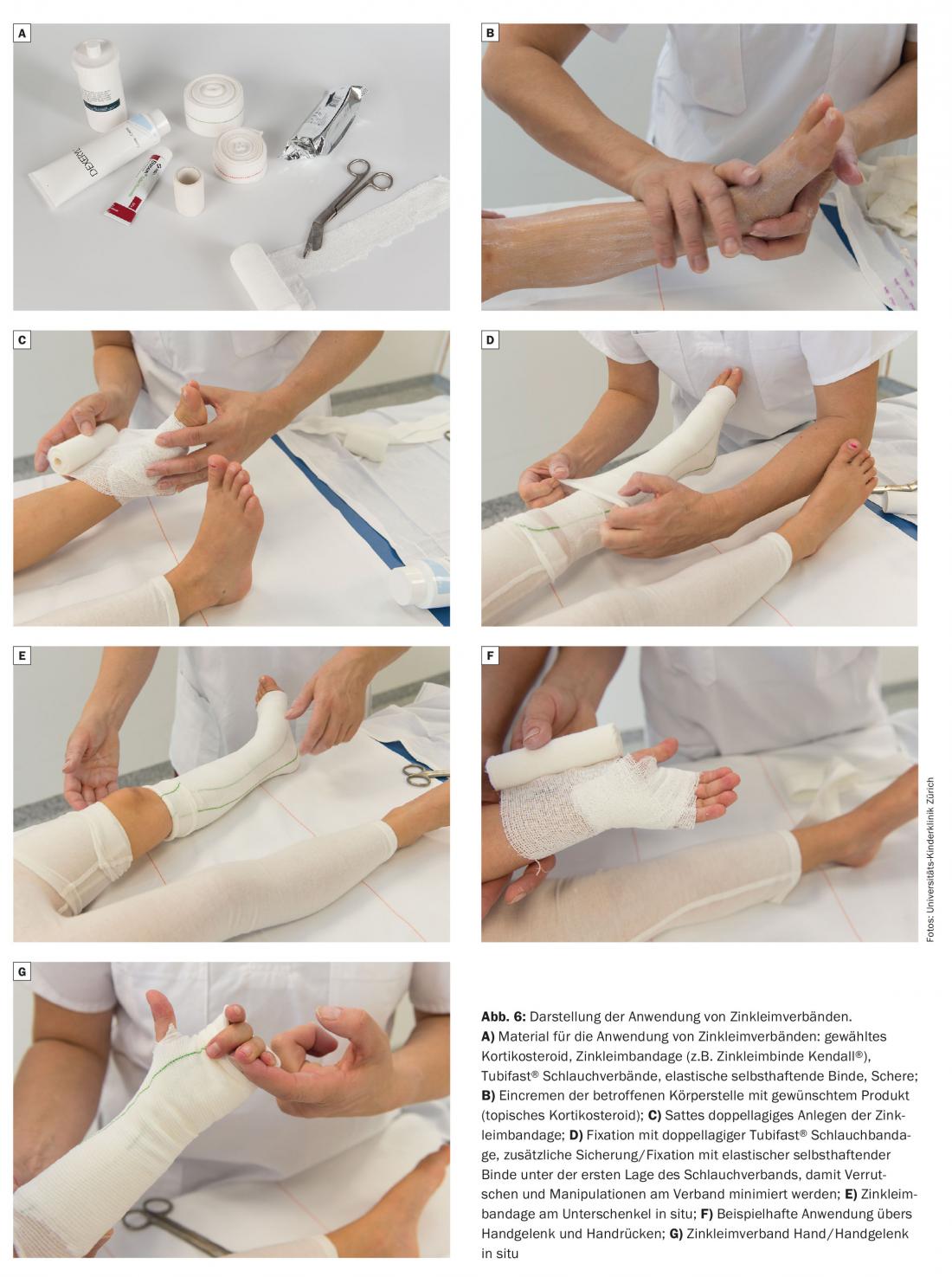
Zinc glue bandages: The zinc glue bandage (ZLV) consists of gauze bandages impregnated with a zinc paste. The longitudinally and transversely elastic carrier fabric with two-dimensional deformability enables precise bandage guidance without cutting in or off, even at difficult anatomical transitions. Commercially available ready-to-use zinc paste bandages (usually 7-10 cm wide) are very well tolerated by the skin, have an anti-inflammatory effect and allow efficient occlusive local therapy [7]. In our experience, the use of ZLV in children has proven particularly effective in cases of persistent chronic eczema on the extremities such as the elbows, wrists/hands, knees and lower legs/ankles. We use ZLV together with mostly moderate to potent corticosteroids (class III; if necessary, class III steroid diluted 1:1 with nursing cream). After bathing/showering, the corticosteroid ointment is applied to the affected eczema areas in rather small areas (possibly supplemented by a care cream for unaffected areas). The zinc paste bandage is then applied and covered with Tubifast® tubular bandage or alternatively Tubegaze® tubular bandage (Fig. 6) . Although ZLVs can in principle be left in place for two to three days, they should be changed daily in children and in everyday practice, in combination with prior skin cleansing (bath/shower). We use ZLV over topical corticosteroid occasionally for five to seven days at the beginning (full day or overnight only), but then the majority of the time we use it as an anti-inflammatory interval therapy for, say, three consecutive nights per week. It should be noted that in areas of thinner skin such as the elbows or the back of the knees, excessive daily occlusive steroid application with ZLV may well provoke steroid atrophy of the skin (clearly visible in the appearance of striae).
Practical treatment examples
Exacerbated (whole body) eczema (Fig. 1) : Both patients shown have very extensive atopic eczema involving the entire integument with (sub)erythroderma. In the infant, there is erosive, bacterial superinfected eczema on the head area and on the hands and flexures. The school-aged boy also has multiple excoriations, especially on the extremities, and extensive lichenified areas. Both children are also plagued by severe itching at night. The following treatment plan was used here in the acute phase, carried out daily on an outpatient basis by our skin care team and accompanied by a doctor:
- Wet-wrap therapy (Fig. 4) all over the body with Elocom® (mometasone) cream 1:5 in soft ointment KA for seven days; in infants with trial face dressing overnight.
- In combination with daily bath, lukewarm, max. 10 min, with some oil added (e.g. Balmed Hermal Plus® or Antidry Badeöl® or Xeracalm Badeöl®) and antiseptic skin wash at the end of the bath (e.g. with Procutol® wash lotion).
- In the infant, due to the pronounced bacterial superinfection (smear: S. aureus) during WWT, oral antibiotic administration (amoxicillin-clavulanic acid, 40 mg/kg 2×/d).
- Fixed antihistamine administration during WWT (in infants Feniallerg® drops, in schoolchildren Xyzal® tablets during the day, Atarax® tablets in the evening).
After completion of WWT, there was a change to the following regimen for another four weeks (with Kispex support if necessary – this is to be determined individually):
- In the morning: Apply moisturizing cream all over the body.
- Evening: Daily bath, lukewarm, max. 10 min, alternatively showers
- Immediately afterwards, apply Elocom® cream 1:1 in Dexeryl® cream KA, dispenser of 200 g, generously to severely affected areas on three consecutive days per week. For the remaining, unaffected skin areas, as well as on cortisone-free days for the entire body, apply moisturizing skin care cream.
- After applying the evening creams, wear Tubifast® Garments overnight
- On the face daily in the evening application of Protopic® Ointment 0.1%
- Antihistamines only as needed.
Further therapy is then determined on the occasion of the follow-up after four weeks (e.g. further reduce corticosteroid application to two consecutive days per week and to smaller areas).
The chronicized (flexural/hand) eczema (Fig. 2): The patient pictured presents with highly chronic atopic eczema predominantly of the extremities with multiple excoriations and marked lichenification, accompanied by severe pruritus and nocturnal scratching. Topical corticosteroids are already used (with restraint).
The following treatment plan was recommended here for the first four weeks and instructed by our skin care team:
- In the morning: Apply moisturizing cream all over the body.
- Evening: Daily bath, lukewarm, max. 10 min, alternatively showers
- Immediately afterwards, apply Elocom® ointment generously to affected areas (hands, forearms incl. elbows) under a zinc glue bandage (Kendall® zinc glue bandage), extending from the base of the fingers to above the elbows (Fig. 6) – this on four consecutive days per week.
- On cortisone-free days, apply moisturizing cream all over the body; if itching persists, apply Tubifast® tubular bandage over the arms (or Tubifast® garments for the entire upper body).
- Antihistamines as needed.
After four weeks, the situation is evaluated and, if progress is good, the corticosteroid application is reduced to two to three consecutive days per week, still with or without ZLV, depending on the skin condition. A calcineurin inhibitor (Protopic® ointment 0.1% or Elidel® cream) can be used on cortisone-free days to treat persistent eczema (e.g., hands, elbows).
The nummular (superinfected) atopic eczema (Fig. 3) : These two patients have – despite ongoing therapy – a long-standing persistent nummular superinfected eczema with pronounced erosive plaques. After taking bacteriological swabs, we used the following treatment regimen here (performed daily on an outpatient basis by our skin care team and monitored by a physician):
- Wet-wrap therapy (Fig. 4) with Elocom® (mometasone) cream 1:5 in soft ointment KA on large areas of the extremities for seven days (for the most severely affected circumscribed plaques, use Elocom® ointment undiluted if necessary).
- In combination with a daily bath, lukewarm, max. 10 min, with some oil added (e.g. Balmed Hermal Plus® or Antidry Badeöl® or Xeracalm Badeöl®) and antiseptic skin wash at the end of the bath (e.g. with Procutol® wash lotion).
- Due to the pronounced bacterial superinfection (smear: S. aureus) during WWT oral antibiotic administration (amoxicillin-clavulanic acid, 40 mg/kg 2×/d).
- Fixed antihistamine administration during WWT (Xyzal® drops during the day, Atarax® drops in the evening).
After completion of WWT, topical corticosteroid under zinc glue dressings (Fig. 6) is applied to the extremities for, say, three consecutive days per week (with Kispex support, if necessary) until the next evaluation after four weeks.
Instruction and advice
In everyday clinical practice, it is evident that families of children with atopic eczema have a very great need for advice, especially initially. For the effectiveness and success of the therapy, it is essential to discuss the implementation of the treatment plan with the family and the patient several times and in detail. Not insignificant are objective and subjective explanatory approaches of the respective family and resulting accordingly used additional (often undeclared) treatment approaches. At the Children’s Hospital Zurich, as in other treatment institutions for infantile eczema, this counseling service is provided by specialized staff. A counseling center for atopic dermatitis, directly accessible to all those affected, is being set up on behalf of aha! (Allergy Center Switzerland) in collaboration with CK-Care and the Children’s Hospital Zurich. This counseling center ensures interprofessional care and is available free of charge to all affected patients and their families. Availability: Monday to Friday at 044 266 84 35 or at www.aha.ch.
Literature:
- Eichenfield LF, et al: Guidelines of care for the management of atopic dermatitis. J Am Acad Dermatol 2014; 71(1): 116-132.
- Atopic eczema in children: Management of atopic eczema in children from birth up to the age of 12 years. NICE Clinical Guidelines 2007.
- Gutman AB, et al: Soak and smear: a standard technique revisited. Arch Dermatol 2005; 141: 1556-1559.
- Janmohamed SR, et al: The proactive wet-wrap method with diluted corticosteroids versus emollients in children with atopic dermatitis: A prospective, randomized, double-blind, placebo-controlled trial. J Am Acad Dermatol 2014; 70: 1076-1082.
- Devillers ACA, Oranje AP: Wet-wrap treatment in children with atopic dermatitis: a practical guideline. Pediatr Dermatol 2012; 29: 24-27.
- Goodyear HM, Spowart K, Harper JI: ‘Wet-wrap’ dressings for the treatment of atopic eczema in children. Br J Dermatol 1991; 125: 604.
- Parboteeah S, Brown A: Managing chronic venous leg ulcers with zinc oxide paste bandages. Br J Nurs 2008; 17(6): 30, 32, 34-36.
DERMATOLOGIE PRAXIS 2015; 25(6): 6-13











