Asthma-like symptoms are common in early childhood and are often the reason for hospitalization, especially in young children. There are many risk factors for such an occurrence – approaches to counteract them in infants up to preschool age and to prevent later adult asthma were presented at the ERS Congress in Barcelona.
Previous research suggests that atopic dermatitis and allergic sensitization are major risk factors for the development of asthma. Norwegian researchers led by Anine Lie of Oslo University Hospital investigated whether primary prevention with skin softeners and early introduction of allergenic foods reduced the risk of asthma in preschool children [1].
2397 infants from the general population in Norway and Sweden were randomly assigned at birth to either no intervention, a skin intervention (regular skin emollients such as oils and skin creams from 2 to 32 weeks of age), or dietary intervention (exposure to peanuts, cow’s milk, wheat, egg from 3 months of age), or received both interventions. Asthma was defined by the occurrence of at least two of the three criteria:
- ≥3 episodes of bronchial obstruction.
- medical diagnosis of asthma
- Taking asthma medication after the 9th month of life.
Criteria were reported in questionnaires every 3-6 months from 3-36 months of age. The primary endpoint was asthma at three years of age after intention-to-treat (ITT).
Asthma risk could not be reduced
The overall prevalence of asthma at three years was 13.2%. 69 of 488 patients (14.1%) in the no intervention group, 53 of 418 (12.7%) with skin intervention, 70 of 510 (13.7%) with nutrition intervention, and 53 of 437 (12.1%) with both interventions. Asthma risk was not significantly affected by the interventions, with an ITT main effect risk difference of 2.7% (95% CI 1.3-6.8) and -0.5% (95% CI 5.2-4.3) by skin and food intervention, respectively. No significant interaction effect was observed (p=0.63).
Primary prevention strategies aimed at reducing atopic dermatitis and/or food allergies fail to reduce asthma risk at age three, the Norwegian researchers conclude.
Pollen exposure in childhood may be relevant for asthma
Pollen exposure is associated with respiratory symptoms in children and adults. However, the relationship between pollen exposure and respiratory symptoms in infancy, a particularly vulnerable period, remains unclear. PD Dr. Jakob Usemann and colleagues from the University Children’s Hospital of Basel, Switzerland, investigated whether pollen exposure is associated with respiratory symptoms in infants and whether maternal atopy, infant sex, or air pollution modify this association [1].
They examined 14 874 observations from 401 healthy infants in the Basel-Bern Infant Lung Development (BILD) cohort. The association between pollen exposure and respiratory symptoms, collected in weekly telephone interviews, was evaluated using generalized additive mixed models (GAMM). Effect modification by maternal atopy, infant sex, and air pollution (NO2, PM2.5) was assessed with interaction terms.
Per infant, 37 ± 2 (mean ± standard deviation) respiratory symptom scores were assessed during the analysis period (January to September). Pollen exposure was higher during the day (RR [95%-KI] per 10% pollen/m3: combined 1.006 [1.002, 1.009]; tree 1.005 [1.002, 1.008]; grass 1.009 [1.000, 1.23]) and during the night (combined 1.003 [0.999, 1.007]; tree 1.003 [0.999, 1.007]; grass 1.014 [1.004, 1.024]) were associated with increased respiratory symptoms. While there was no effect modification by maternal atopy and sex of the child, there was a complex crossover interaction between combined pollen and PM2.5 (p-value 0.002) (Fig. 1).
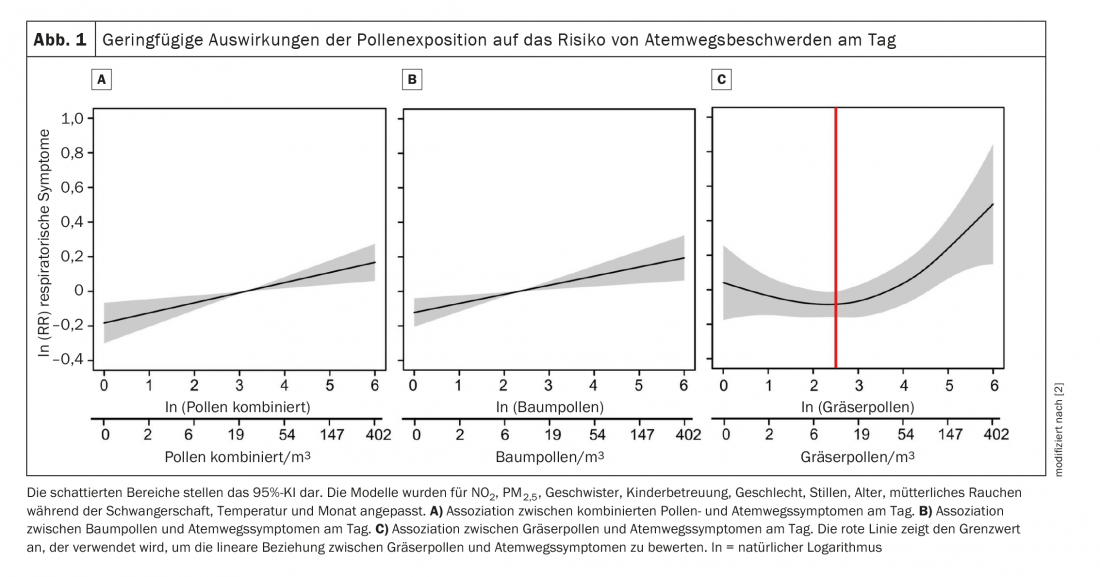
As early as the first year of life, exposure to pollen was associated with an increased risk of respiratory symptoms regardless of maternal atopy or infant sex, the speaker said. Because infancy is a particularly vulnerable time for lung development, the identified adverse effect of pollen exposure may be relevant to the development of chronic asthma in childhood.
Age-related patterns identified
Julie Nyholm Kyvsgaard of the COpenhagen Prospective Studies on Asthma in Childhood (COPSAC) unit at University Hospital in Copenhagen and her colleagues took as an opportunity that while episodes of asthma-like symptoms are common in young children, little is known about risk factors and patterns of daily symptom burden. They investigated possible risk factors and their age-related influence on the number of asthma-like episodes at the age of 0-3 years [1].
The study population included 700 children from the COPSAC2010 mother-child cohort who were followed prospectively from birth to 3 years of age with asthma-like symptoms recorded by parents in daily diaries. Symptoms included cough, wheeze, shortness of breath/dyspnea. Risk factors were analyzed by quasi-Poisson regressions that examined the interaction with age. An episode was defined as asthma-like symptoms for ≥3 consecutive days, and individual episodes had to be interrupted by ≥3 days without symptoms.
662 children had available diary data with a median prevalence of five asthma-like episodes during the first three years of life (interquartile range, IQR, 2-11). A peak appeared during the second year of life. A seasonal pattern was also evident, with a peak in the winter season. The median duration of an episode was five days (IQR 3-10). Maternal asthma, maternal antibiotic use, low birth weight, male sex, high polygenic asthma risk score, and high airway immune score predicted a higher number of episodes in a multivariable analysis (Table 1) .
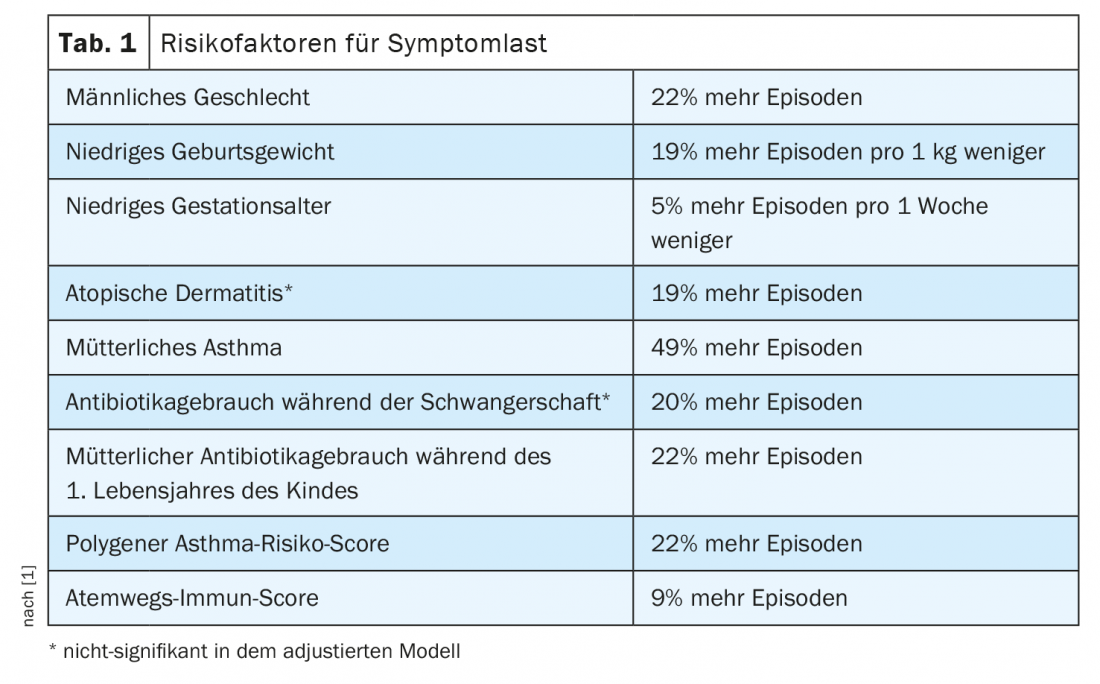
For each additional clinical risk factor a child had, the Danish researchers found a 34% increase in the number of episodes (sex, birth weight, maternal asthma, incidence ratio 1.34; 95% CI 1.21-1.48; p<0.001). Maternal asthma, preterm birth, cesarean section, low birth weight, and siblings at birth interacted significantly with age (p<0.05), indicating an increasing number of episodes in 1st trimester, 2. and 3 years of age for all but children with siblings shows where symptom burden decreased with age.
Thanks to diary records of asthma-like symptoms in the first three years of life, the researchers were able to identify risk factors of symptom burden with different age-dependent patterns. This offers new insights into the etiology of early asthmatic symptoms and could help clinicians identify patients at risk and, if necessary, initiate early therapy, the speaker concluded.
Congress: ERS Congress 2022
Sources:
- Oral presentation: Early childhood risk factors for wheezing and later asthma. European Respiratory Society Congress, Barcelona, Sept. 4, 2022.
- Gisler A, Eeftens M, de Hoogh K, et al: Pollen exposure is associated with risk of respiratory symptoms during the first year of life. Allergy 2022; doi: 10.1111/all.15284.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(4): 20-21 (published 12/1/2012, ahead of print).











