At this year’s ESH Congress in Milan, more detail was provided on how to improve adherence and compliance in hypertension therapy. In particular, simplification of drug treatment results in better adherence rates. Furthermore, international studies and models were presented that could have a decisive influence on future hypertension control.
Prof. Jean-Jacques Mourad, MD, Paris, spoke about the goals for blood pressure control within Europe: in most European countries, good control is achieved in less than 50% of patients treated. Therefore, France has set a goal to increase the success rate of blood pressure control in hypertensive patients to 70% based on important key points [1].
“Italy has targeted the same success rate. Several Randomized Control Trials (RCTs) show that it is possible to achieve effective blood pressure control in 70-80% of treated hypertensive patients. In particular, the more extensive use of combination therapy based on two or three classes of antihypertensive drugs working synergistically together could significantly improve control,” Dr. Mourad said. “An exemplary example is Canada, which achieved a control rate of 64.6% in 2009. The so-called Canadian Hypertension Education Program (CHEP) began in 1999 and includes annual hypertension updates.” According to current recommendations, all Canadian adults should have their blood pressure measured at every eligible doctor visit. Optimal blood pressure control also includes a survey of overall cardiovascular risk. For those who are ill, self-monitoring and control at home is appropriate. Lifestyle modifications are not only effective in prevention but, when combined with medications, are also effective in treating and reducing cardiovascular risk. In any case, a treat-to-target strategy is useful and adherence should be a constant focus.
Prof. Massimo Volpe, MD, Rome, gave some tips on how to improve patient care: “Simplifying therapy is one of the best ways to improve compliance, which in turn is crucial for achieving treatment goals. Complicated medical cures are a hindrance in this regard [2], and the pill burden can be reduced by fixed doses (“fixed-dose combination” FDCs) [3]. Further, a home blood pressure measurement (HBPM) creates a partnership between patient and physician, which also has a positive impact on blood pressure management.”
Current topics
Joseph Redon, MD, Valencia, went into more detail about “electronic health registries” (EHRs). Such systematically collect data from individual patients or entire populations and could improve the management of noncommunicable diseases (NCDs) such as hypertension. In particular, whole-population studies allow monitoring of risk factors, show incidence, and provide insight into the effectiveness of therapies. “A European network would be desirable, but can only be achieved through good interoperability between different systems,” Dr. Redon said.
The implications of recent U.S. hypertension studies for the international management of this disease were presented by Prof. William C. Cushman, MD, Tennessee:
- The results of the ACCORD, SPS3, HALT, and SPRINT trials raise the question of whether blood pressure should be treated to a lower level
- NEPHRON-D and HALT address the risk and benefit of combined blockade of the renin-angiotensin-aldosterone system in diabetic nephropathy (chronic kidney disease)
- CORAL aims to show whether angioplasty or a vascular stent could be effective for renal artery stenosis
- SYMPLICITY HTN-3 is designed to provide further data on the short-term efficacy and safety of renal denervation in resistant hypertension.
Guidelines for arterial hypertension
An important simplification from the 2007 guidelines is the establishment of a target blood pressure <140 mmHg independent of cardiovascular risk. The new 2013 guidelines also consider out-of-office blood pressure in addition to office blood pressure in the risk stratification model. Blood pressure measured at home (home BP) correlates more strongly with organ damage and prediction of cardiovascular events is thus significantly better. The two forms of measurement should ultimately be used in a complementary manner because they provide different information.
Lifestyle modifications such as reduced salt intake, weight control (BMI of 25 kg/m2), and smoking cessation continue to be an important component in the prevention and treatment of hypertension.
Regarding the choice of antihypertensive medication, several points should be considered. First, there is no evidence that age and sex are relevant in the decision, except that caution should still be exercised in the use of RAS blockers in women planning pregnancy. Overall, it also appears that most patients require combination therapy with at least two medications to achieve sufficiently good blood pressure control.
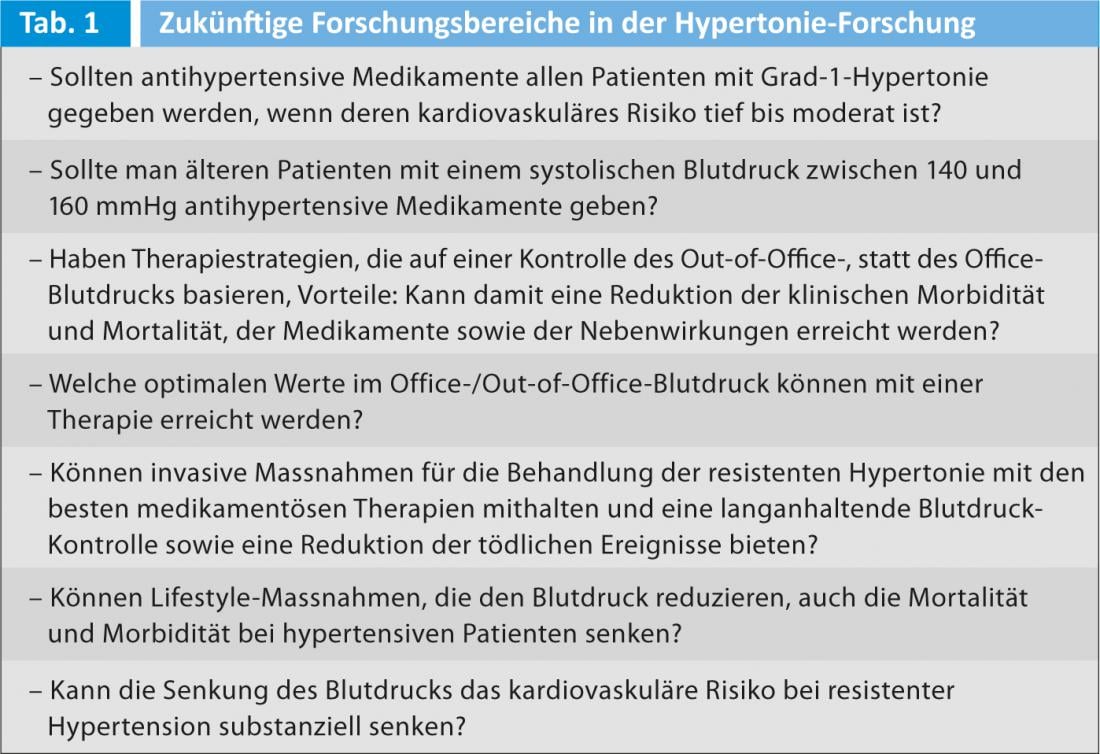
Various questions remain unanswered, and the evidence from research is still lacking here (Tab. 1).
Source: 23rd European Meeting on Hypertension & Cardiovascular Protection, June 14-17, 2013, Milan, Italy.
Literature:
- Mourad JJ, Girerd X: Objective for 2015: 70% of treated and controlled hypertensive patients. Seven key points to reach this goal in practice. A joint call for action of the French League Against Hypertension and the French Society of Hypertension. J Mal Vasc. 2012 Dec; 37(6): 295-9. doi: 10.1016/j.jmv.2012.09.002. Epub 2012 Oct 31.
- Burnier M, et al: Issues in blood pressure control and the potential role of single-pill combination therapies. Int J Clin Pract. 2009 May; 63(5): 790-8. doi: 10.1111/j.1742-1241.2009.01999.x. Epub 2009 Feb 11.
- Redon J, et al: Practical solutions to the challenges of uncontrolled hypertension: a white paper. J Hypertens Suppl. 2008 Dec; 26(4): 1-14. doi: 10.1097/01.hjh. 0000343507.74401.45.











