In treatment-resistant severe cases, a biologic representative of a new class of substances is available. Several evaluations of different forms of therapy came up with exciting results. One study made the first head-to-head comparison of first-line biologics.
In bacterial osteomyelitis in childhood important to know: It is a usually hematogenous metastasis. The externally associated, postoperative, post-traumatic osteomyelitis, which is more common in adults, plays only a minor role, Dr. Jakob Armann made clear right at the beginning of his lecture with regard to the differences between children and adult patients. What you have to think about, however, according to the colleague from the Pediatric Immunology Department of the Clinic and Polyclinic for Pediatrics and Adolescent Medicine at the University Hospital Carl Gustav Carus in Dresden, are the vertebral osteomyelitides and spondylodiscitides, which can occur at any age and whose symptoms are often very unclear. With back pain and fever, you have to at least keep in mind that it can also be bacterial spondylodiscitis. The specific forms of osteomyelitis or spondylitis (due to M. tuberculosis) should also be considered secondary, but should be included, for example, when traveling to high-prevalence countries or migrating, even in children. “But that’s a post-primary form, so that’s where an x-ray can definitely be worthwhile if you’re in doubt to see if there’s anything there at all before you digress too much.”
Diagnostics
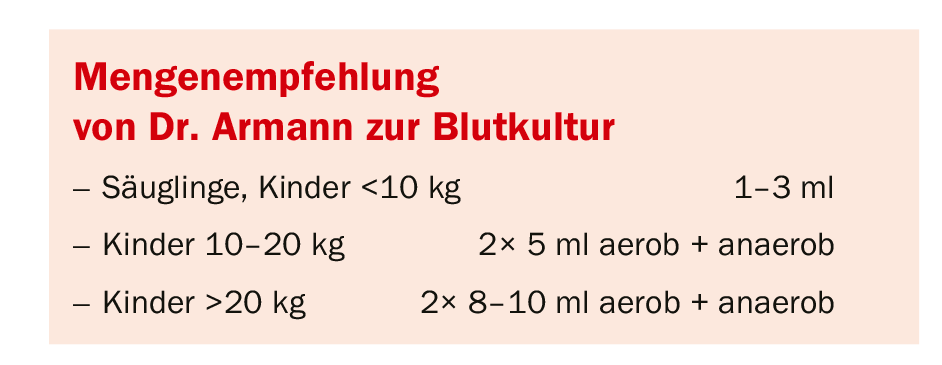
Blood cultures are a very important factor in the diagnosis of osteomyelitis. In at least 30% of cases, the pathogen can be confirmed by blood culture. It is therefore also essential that the blood is drawn before starting antibiotic therapy. The basic rule for blood culture is: a lot helps a lot. “The more blood you put in the blood culture bottles, the higher the chance that you will also find the pathogen.” But Dr. Armann warned: “With the children’s blood culture bottles, which are usually designed for 3 ml, overfilling has no positive effect. “So if you have more blood than you can fit in the children’s blood culture bottles, you’d better take an adult bottle,” the doctor advised.
The question of imaging then arises: in cases of suspected bacterial arthritis, sonography is the primary diagnostic imaging modality of choice and is usually sufficient. MRI should only be used for arthritis if the findings are unclear. It is different with osteomyelitis: here MRI is definitely called for. X-ray is really only of value in the differential diagnosis of a fracture or in situations where, for example, an MRI is not available prior to surgery.
With regard to a possible puncture, Dr. Armann reminded the patient: “Puncturing always means securing the pathogen. The infectiologist therefore says: everyone is punctured. This gives you the pathogen and allows you to choose the best possible therapy. “On the other hand, we do have to pragmatically ask ourselves the question: Do we have to puncture every bone now?” The expert reminded of the not inconsiderable effort – it is a major intervention with greater risks, the puncture requires anesthesia, you need an orthopedist for it, etc.. His recommendation therefore: “You should always puncture joints! It is easy to do, it only needs a short sedation, you can even do it on a septic patient in the ICU. There are really no reasons not to do it. Bone is a little different. If everything is relatively typical – typical MRI image, typical clinic – you can do without it from my point of view.” Exceptions are situations in which the differential diagnosis is unclear, the course is strange, or the patient has abscesses, in which case it is not only a matter of securing the pathogen, but also a therapeutic measure by means of surgery.
Therapy
For therapy from an infectiological point of view, the decisive factor is always the type of pathogen involved. “Actually, it’s relatively simple,” says Dr. Armann: “It’s staphylococci for the vast majority, no matter what age group you take.” And from that, you can also quickly deduce what the best therapy is for it, which is flucloxacillin or, alternatively, cefazolin in appropriate doses.
If you look at it a little more closely, it’s not just the staph that plays a role. Kingella kingae, a gram-negative rod bacterium that causes a number of infections that should not be underestimated, is also frequently found, especially in children <3 years. And in the case of animal bites, the pathogens located in the tooth space of the respective animal are added (Tab. 1) . In this regard, Dr. Armann warned that children are not always able to clearly name a bite. They have, for example, cats or pet rats, and then in the course of playful actions there is an injury, which is not even perceived as a bite. “And with something like that, we just get to the point: if you don’t have the very classic osteomyelitis, if something seems weird in the course, then a puncture is just indicated!”
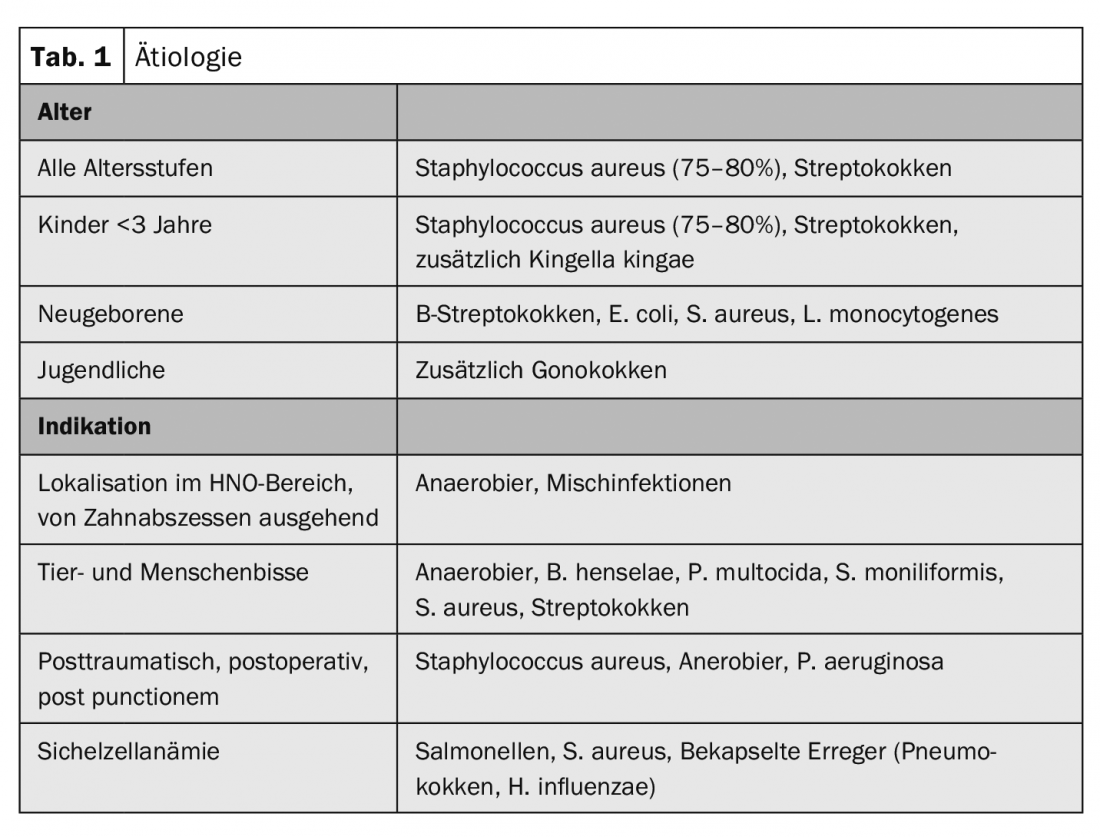
However, even without knowledge of the pathogen, a calculated therapy can be derived: Thus, in children >3 years, flucloxacillin or cefazolin is indicated because of the high probability of staphylococci. In those under 3 years of age in whom Kingella kingae is a concern, cefuroxime is switched to because Kingella kingae is not flucloxacillin sensitive. But please keep an eye on the dosage, the expert warned. “We have high dosing in the treatment of staph infections because we need a really good active level. Once we get into an area where we’re also meeting with anaerobic pathogens, we would then recommend ampicillin/sulbactam as primary therapy.”
Once the pathogen has been identified, of course, it becomes easy: in the case of staphylococci, one can stick to flucloxacillin, while MRSA plays practically no role in the pediatric sector in German-speaking countries. If it does occur, it is somewhat difficult to treat. Here, Dr. Armann advises getting help if you don’t have experience with it yourself. “With vancomycin, you need to make sure you’re giving enough but also not doing any damage.” For strep, penicillin is the best and penicillin usually works for Kingella kingae, otherwise cefuroxime is the alternative.
With regard to the duration of therapy, the pediatrician explained that he and his colleagues in Dresden initially treat all patients parenterally. Regarding the question of when to switch, according to him, quite a lot has happened in the last 10-15 years. “Uncomplicated arthritis/osteomyelitis is a term that orthopedists don’t like because they say every bone and joint infection is complicated per se. But from an infectious disease perspective, there are osteomyelitides that are relatively classic, without major complications, where we think you can switch to oral antibiotic therapy as early as 96 hours, four days.” For this to happen, however, all of the following criteria must be met:
- clinical improvement
- at least 24 hours afebrile
- CrP <20 mg/l or already decreased by 2/3
- oral medication possible
- no vertebral osteomyelitis/spondylodiscitis
If patients have vertebral osteomyelitis/spondylodiscitis, they would generally be treated longer in Dresden, according to Dr. Armann, because they are often prone to complications “and we don’t dare change over too early.”
Cefadroxil as a compromise
However, if all the above points are fulfilled – what do you treat the patients with? Staphylococcus as the main pathogen needs a good orally available staphylococcal effective drug. Cefadroxil is the best choice here. Clindamycin is certainly not bad as an alternative, but has the disadvantage that resistance rates for S. aureus are around 20-30% according to figures in Germany. If the pathogen is not determined, the expert therefore advises not to use clindamycin, but cefadroxil. For streptococci that are penicillin-sensitive, amoxicillin is indicated. “I wouldn’t take penicillin V because it doesn’t have good bioavailability. It’s perfectly adequate for strep throat, but for invasive strep infection, it’s not my first-line agent.”
If the pathogen remains unknown, which can also happen, staphylococcal treatment is also recommended for children over the age of three, while cefuroxime is recommended for children under the age of three without evidence of the pathogen, which is clearly inferior to cefadroxil in terms of bioavailability, which is why it is not the first choice for older children. However, because Kingella kingae cannot be excluded, it is used here as a compromise. And last but not least: If the suspected infection is not confirmed, the therapy can simply be discontinued. “There is no minimum duration of useless antibiotic therapy.”

The total duration of therapy is distinguished in two ways: firstly, between bacterial arthritis from osteomyelitis – osteomyelitis is always treated a little longer – and secondly, between the uncomplicated cases and the complicated ones (Tab. 2) “If you have uncomplicated arthritis or osteomyelitis, you’re actually through in 2-3 weeks, because these infections are well and safely treatable.”
Source: 47th Congress of the German Society for Rheumatology, Dresden (D)
HAUSARZT PRAXIS 2019; 14(10): 28-29 (published 10/24/19, ahead of print).
InFo PAIN & GERIATURE 2019, 1(1): 34-35.











