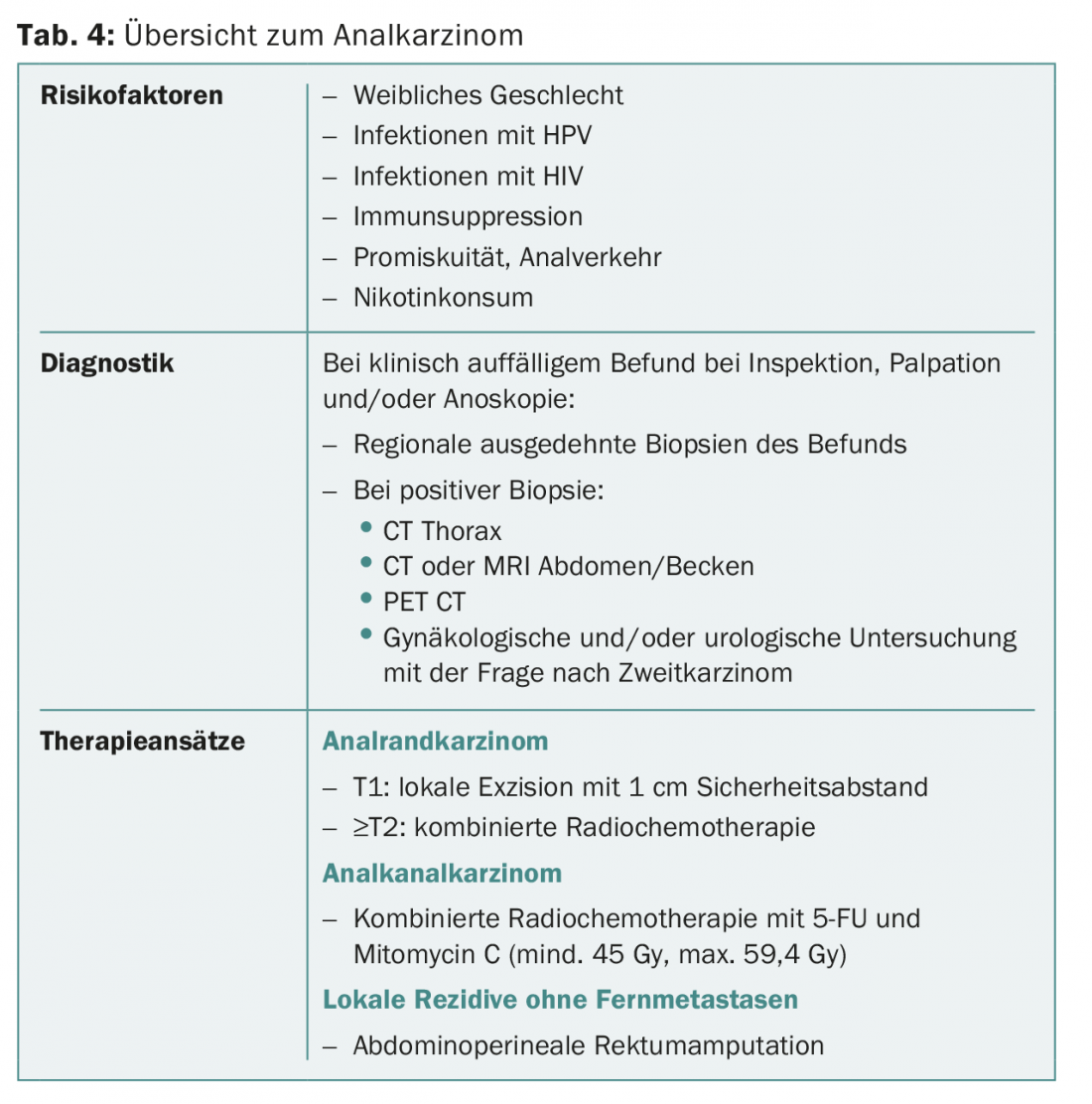
Risk factors for anal carcinoma include female sex, human papillomavirus infections, promiscuity/anal intercourse, smoking, and immunosuppression (e.g., HIV infection). If there are abnormal findings on inspection, palpation, and/or anoscopy, the suspicious region should be biopsied. Stage T1 anal marginal carcinomas can be excised locally. From stage T2, combined radiochemotherapy is performed. Anal canal carcinomas are primarily treated with combined radiochemotherapy (5-FU and mitomycin C, minimum 45 Gy, maximum 59.4 Gy). For local recurrences without distant metastases, abdominoperineal rectal amputation as salvage surgery is appropriate.
Anal carcinoma accounts for approximately 2.5% of all gastrointestinal malignancies [1], with the incidence doubling from 10 to 20 cases per million population over the past 30 years [2]. An increased incidence of anal carcinoma is observed in women, human papillomavirus (HPV) infections, promiscuity and anal intercourse, nicotine use, immunosuppression (e.g., after transplantation), and HIV infection [2]. When the causes and risk factors of anal carcinomas are considered, they are more similar to genital carcinomas than to gastrointestinal malignancies.
Histologically, anal carcinomas are squamous cell carcinomas in more than 90% of cases. Adenocarcinomas occur in less than 5% of patients. These are classified in the group of deep rectal carcinomas and are treated as such. In rare cases, verrucous carcinomas, melanomas, and basal cell carcinomas occur with anal marginal carcinomas.
Risk factor HPV
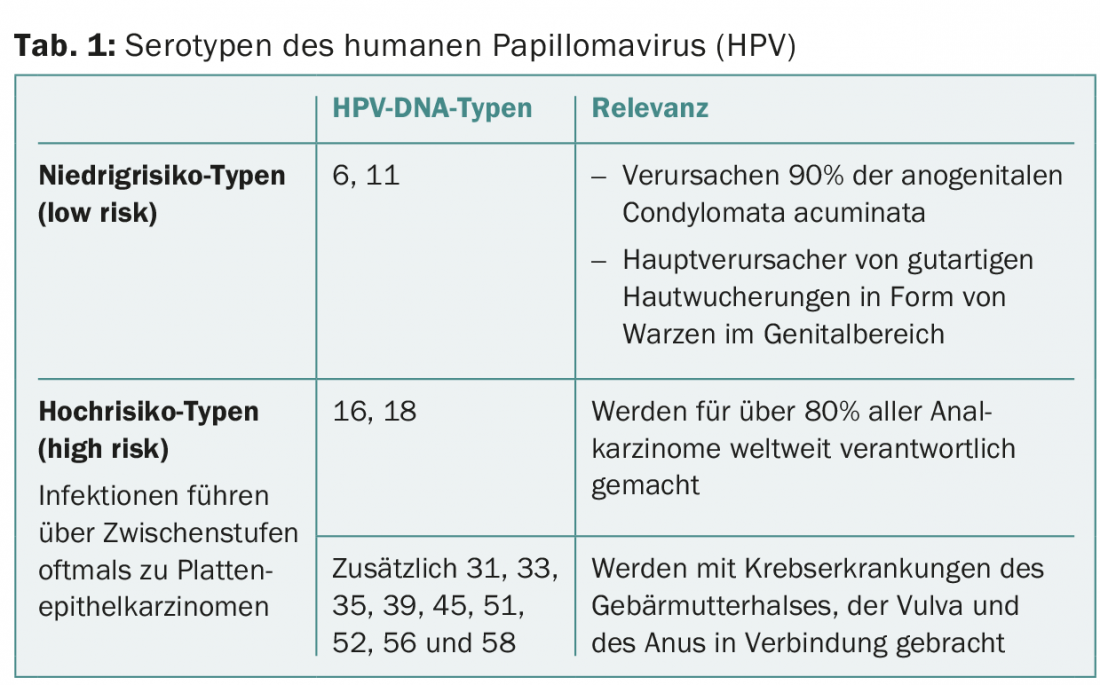
HPV DNA is detectable in 85-90% of patients with anal carcinoma. The causal relationship between HPV infection and the development of anal intraepithelial neoplasia (AIN) or anal carcinoma has been demonstrated by numerous papers [2]. The association between some high-risk HPV types (serotypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, and 58) and the development of high-grade dysplasia or anal carcinoma is considered established (Table 1) [3]. HPV-16 (in up to 75% of tumors) and HPV-18 (approximately 7% of tumors) can be detected most frequently in anal carcinoma [3,4]. Anal carcinomas are more frequently HPV DNA positive in homosexual or bisexual men (97.7%) than in heterosexual men (78%) [5].
Anal canal and anal margin carcinomas
Anal carcinoma is classified into anal canal carcinoma or anal marginal carcinoma based on its location. Anal canal carcinomas are about two to three times more common than carcinomas of the anal verge. These occur more frequently in the female sex, whereas anal verge carcinoma is about four times more common in the male sex than in women [2,5]. The peak age of incidence for anal canal carcinoma is in the 6th-7th week of life. Decade, for anal marginal carcinoma in the 5th-6th decade. Decade of Life.
Anal intraepithelial neoplasia (AIN)
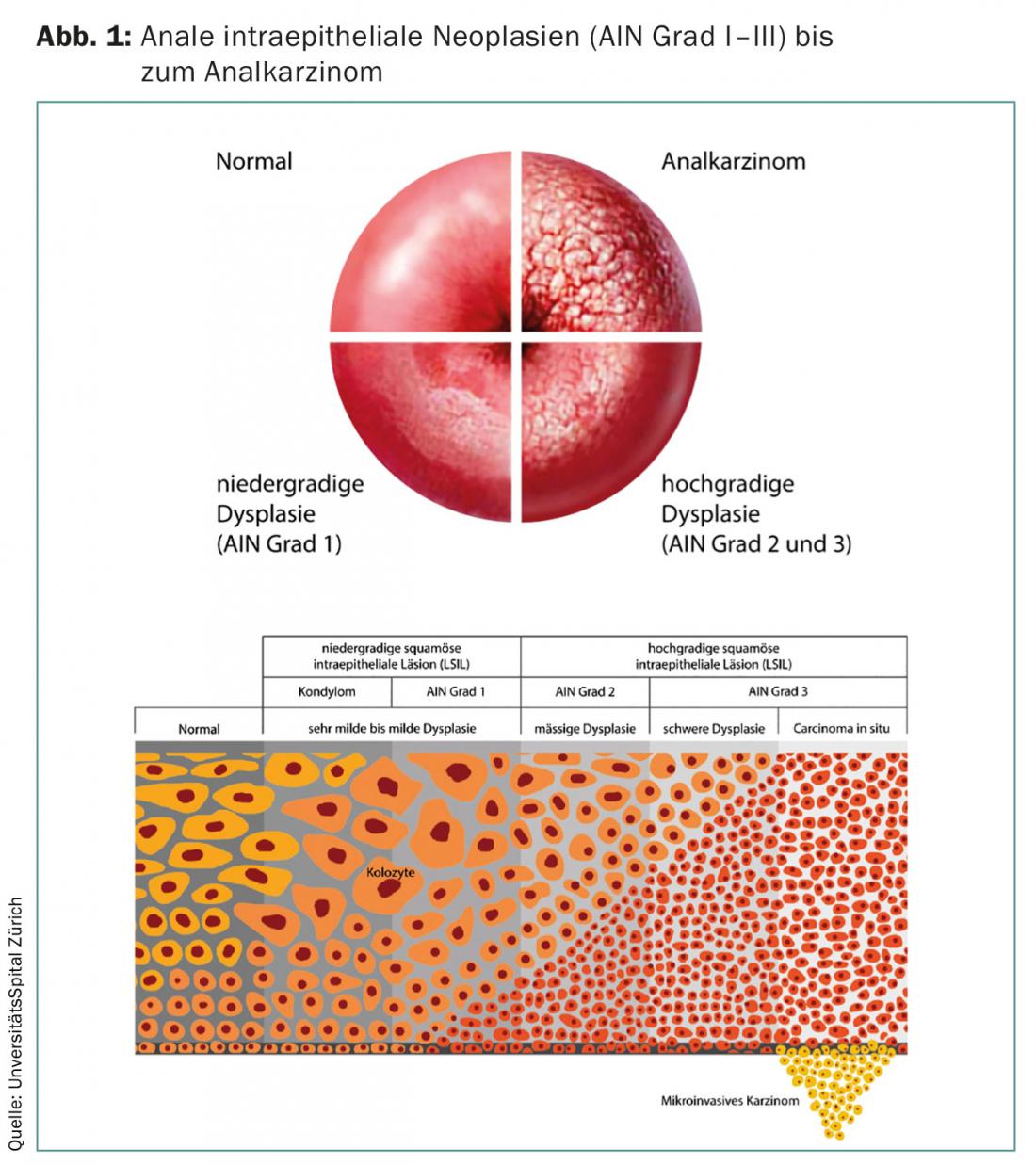
Anal intraepithelial neoplasia (AIN) is classified into three grades (grade I to III) and is considered precancerous. The three grades can merge and develop into anal carcinoma (Fig. 1). While grade I and II AINs may regress spontaneously, a grade III AIN is considered a carcinoma in situ: There is a high risk – especially in immunocompromised individuals – for transition to invasive carcinoma.
Symptoms
The leading symptoms of anal carcinoma correspond to the symptoms of hemorrhoidal disease and rectal carcinoma, so there is often a delay in diagnosis. Patients usually present to the office with fresh blood discharge ab ano. Pain on defecation and perianal pruritus are also occasionally reported. Stool irregularities may also occur. In case of enlarged inguinal lymph nodes and the symptoms mentioned above, anal carcinoma should always be considered. If the examination findings are abnormal, appropriate biopsies should be taken.
Diagnostics
After taking the medical history, the patient is clinically examined by inspection, palpation and anoscopy. The inspection must be carried out in order to check for any spatial lesions, verrucous changes and changes in color. On palpation, look for a mass and/or induration. In addition, the inguinal lymph nodes must always be palpated. Proctoscopically, the anal canal is viewed and examined for space-occupying lesions, verrucous changes, and leukoplakia. In this context, both peri-anal and endoanal biopsies (possibly even anal mapping) must be taken in case of abnormalities.
If a carcinoma is confirmed histologically, staging imaging studies follow. These include CT thorax, CT or MRI of the abdomen and pelvis, and positron emission tomography (PET CT) at most. In female patients, a gynecological examination to exclude cervical carcinoma is essential. In advanced carcinomas (T4), gynecological and urological control is obligatory. For fertile men who wish to have children, it is important to think about cryopreservation before starting therapy for anal carcinoma.
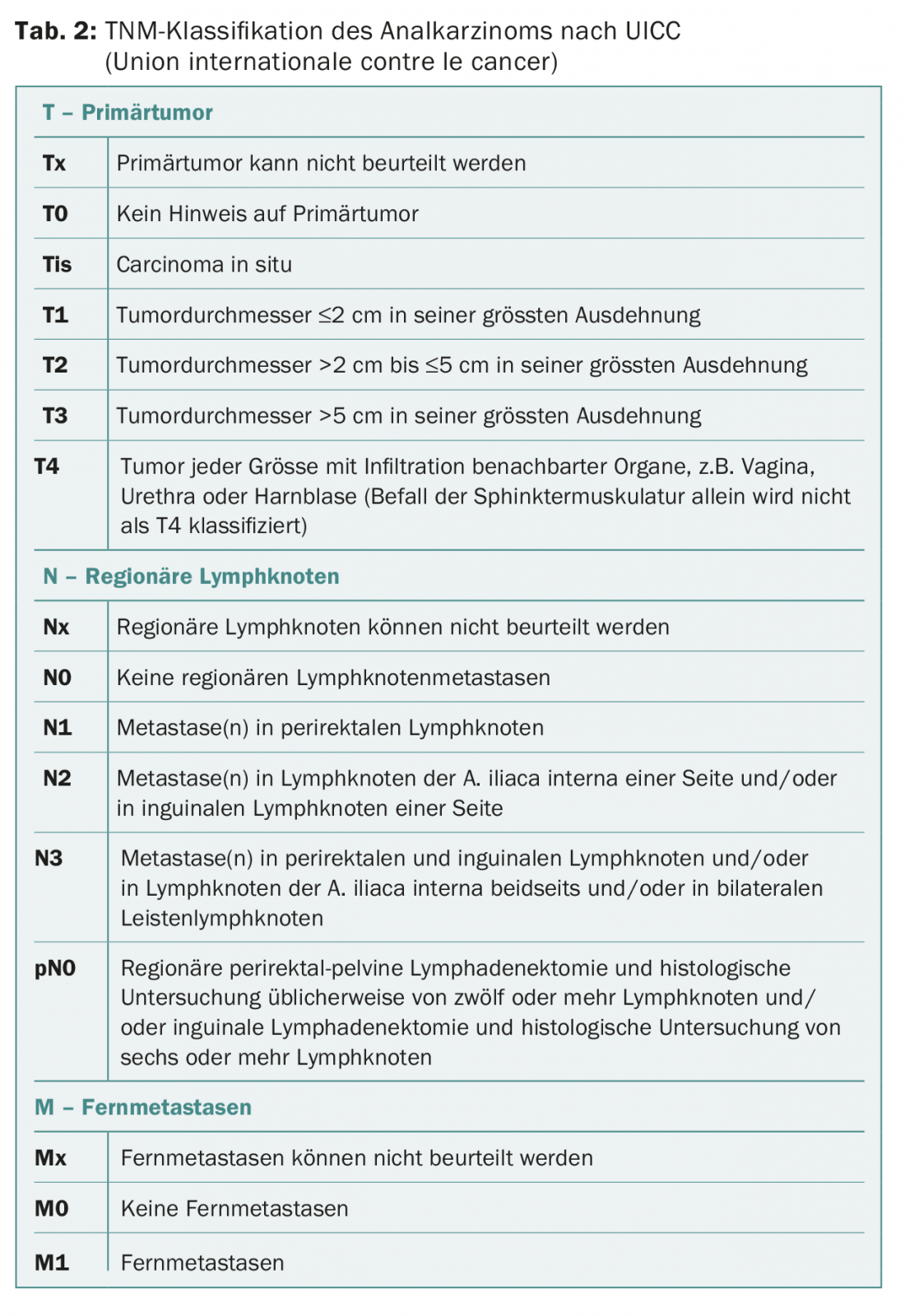
Based on the TNM classification (Table 2), anal carcinoma is divided into four stages (stages I-IV), which directly correlate with long-term survival. Patients with stage IV carcinoma have the worst 5-year survival (45%) compared with patients with stage I or II (86%) [6]. At the time of diagnosis, the tumor is still localized in 90% of patients. Most commonly, anal carcinoma metastasizes to the liver (50%), peritoneum (25%), or lungs (15%) [6]. Advanced tumor (T3 and above) is lymphogenically metastatic in 30-60%, whereas patients with T1 or T2 carcinomas have lymph node metastases in only 10-15%.
Therapy of the anal verge carcinoma
Therapy of squamous cell carcinoma of the skin consists of local excision with a safety margin of 1 cm. Occasionally, plastic surgical flap coverage is also indicated for T1 tumors (≤2 cm).
Locally advanced anal marginal carcinomas (≥T2) are primarily treated with combined radiochemotherapy according to the Nigro regimen for anal anal carcinomas [7]. If radical excision involves the sphincter muscles, primary combined radiochemotherapy is also recommended [8].
Therapy of anal canal carcinoma
Combined neoadjuvant radiochemotherapy with 5-fluorouracil (FU) and mitomycin C is considered the international standard of care for squamous cell carcinoma of the anal canal and squamous cell carcinoma of the anal verge ≥T2 [7]. Combined radiochemotherapy is superior to radiotherapy alone in terms of longer disease-free survival, lower local recurrence rate, and longer colostomy-free survival. Only in the absence of a chemotherapy indication (e.g., elderly patients and/or many relevant comorbidities) should radiotherapy alone be considered and discussed in an interdisciplinary board.
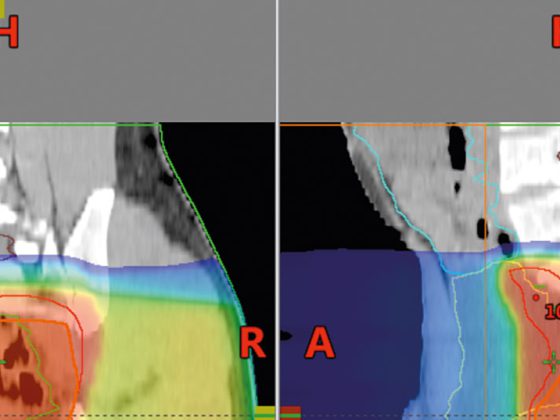
Radiation therapy is usually administered five times a week as conventional fractionated irradiation with a single dose of 2 Gy/d. In addition to treatment of the region of the primary tumor, irradiation of the locoregional lymphatic drainage pathways is both elective and therapeutic. The target volume and target volume dose (CVD) are determined by the radiation oncologist. Unaffected lymph node regions are treated with a ZVD of 45-50 Gy. Affected lymph nodes as well as the primary tumor region are selectively up-dosed with appropriate safety margin up to a ZVD of 59.4 Gy [9].
Combined with radiotherapy, chemotherapy is given with 5-FU on days 1-4 and 29-32 and mitomycin C on day 1 and when the radiation dose of 30 Gy is reached [7,9]. The application of chemotherapy is performed under inpatient conditions via a central access and is managed by appropriately trained oncologists. The creation of a temporary colostomy (e.g., double-barreled sigmoidostomy) is often advisable in cases of stenosing anal carcinoma or restrictive fecal incontinence before combined neoadjuvant radiochemotherapy is performed.
Abdominoperineal rectal amputation is considered the last curative therapeutic option (salvage surgery) for anal canal carcinoma and is performed for biopsy-proven persistent tumor (at least 26 weeks after successful combined radiochemotherapy) or local recurrence. Only if an R0 resection can be achieved is abdominoperineal rectal amputation warranted. Additional inguinal lymphadenectomy is performed for clinical symptoms (e.g., compression), persistent or recurrent disease.
Therapy of adenocarcinoma of the anal canal
Rare adenocarcinoma of the anal canal (<5%) should be treated according to the guidelines for deep-seated rectal cancer. In this case, neoadjuvant radiochemotherapy followed by resection is indicated. We refer to the relevant literature on rectal cancer.
Therapy of metastatic anal carcinoma
Overall, the primary tumor is rather rarely already metastatic at diagnosis (10%) [6], therefore the data regarding palliative chemotherapy is limited. The only first-line palliative chemotherapy regimen involves combination therapy with cisplatin and 5-FU (cisplatin 100 mg/m2 day 1, 5-FU 1000 mg/m2 day 1-5; repeat day 29) [10]. The effect of further combination therapies with e.g. mitomycin C, doxorubicin and cisplatin or paclitaxel, carboplatin and 5-FU has been described in individual studies, but evidence-based data are still lacking to make recommendations.
Local resection of metastases of anal carcinoma has not been established and is therefore primarily not explicitly recommended. Nevertheless, local resection as well as radiotherapy of metastases can be discussed in an interdisciplinary tumor board as part of the overall oncological concept and may be individually appropriate for the patient.
Therapy concepts in the event of a recurrence
In the absence of distant metastases, a curative therapeutic approach should be pursued for local or regional recurrence. Depending on the primary therapy, the surgical options (abdominoperineal rectal amputation) as well as radiooncological therapy reserves are to be evaluated and defined in the interdisciplinary tumor board as therapy procedure. In the case of a locally non-curable recurrence, an individualized, particularly symptom-oriented and interdisciplinary approach (surgery, radiotherapy vs. systemic chemotherapy) must be defined and coordinated.
Aftercare
According to European guidelines, the first clinical follow-up is indicated three months after completion of radiochemotherapy [9]. Follow-up includes clinical examination (inspection, palpation, and anoscopy) and palpation of inguinal lymph nodes. This examination should be performed at three- to six-month intervals for the first two years after initial therapy (whether primary combined radiochemotherapy or local excision). After two years, it is recommended to continue clinical tumor follow-up every six to twelve months until a total of five years after primary therapy (Table 3).
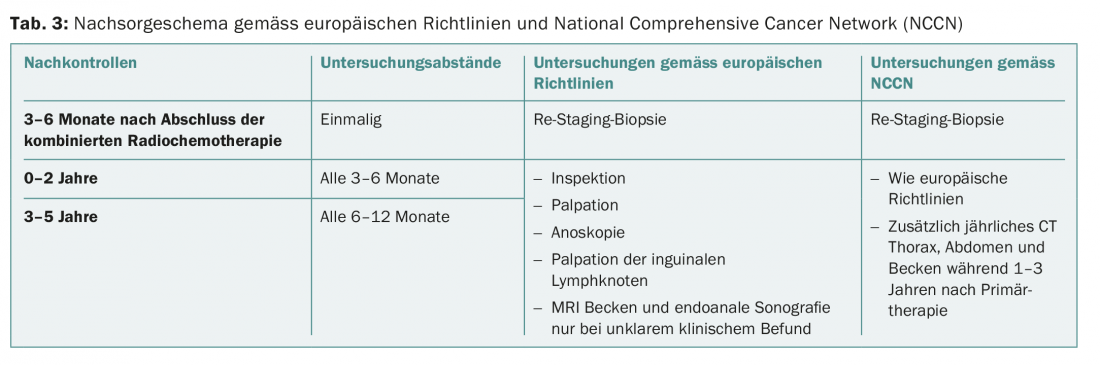
In European guidelines, regular CT follow-up is controversial because recurrences of anal carcinoma are more often locoregional than distant metastases [9]. In contrast, the National Comprehensive Cancer Network (NCCN) recommends annual CT scans of the thorax, abdomen, and pelvis for the first three years after primary therapy. Otherwise, the NCCN guidelines coincide with the European guidelines (Table 3). In our tumor center, we adhere to the NCCN guidelines. MRI of the pelvis and/or endoanal ultrasonography are performed during follow-up only if the clinical findings are unclear [9].
Re-staging biopsy after completion of combined radiochemotherapy for anal canal carcinoma is indicated after three months at the earliest and six months at the latest. Residual tumors on re-staging biopsy and macroscopic tumors warrant re-biopsy six months after completion of primary therapy. If the tumor remains positive, salvage surgery is indicated; the further procedure should be determined in the interdisciplinary tumor board.
Table 4 provides an overview of the diagnosis and treatment of anal carcinoma.
Literature:
- Siegel RL, Miller KD, Jemal A: Cancer Statistics, 2015. Ca-a Cancer Journal for Clinicians 2015; 65(1): 529.
- Johnson LG: Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973-2000. Cancer 2004; 101(2): 281-288.
- Cogliano V, et al: Carcinogenicity of human papillomaviruses. Lancet Oncol 2005; 6(4): 204.
- Bouvard V, et al: A review of human carcinogens–Part B: biological agents. Lancet Oncol 2009; 10(4): 321-322.
- Abramowitz L, et al: Anal squamous intraepithelial lesions and condyloma in HIV-infected heterosexual men, homosexual men and women: prevalence and associated factors. AIDS 2007; 21(11): 1457-1465.
- Klas JV, et al: Malignant tumors of the anal canal: the spectrum of disease, treatment, and outcomes. Cancer 1999; 85(8): 1686-1693.
- Nigro ND, Vaitkevicius VK, Considine B: Combined therapy for cancer of the anal canal: a preliminary report. Dis Colon Rectum 1974; 17(3): 354-356.
- Khanfir K, et al: Patterns of failure and outcome in patients with carcinoma of the anal margin. Ann Surg Oncol 2008; 15(4): 1092-1098.
- 9. Glynne-Jones R, et al: Anal cancer: ESMO-ESSO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014; 25 Suppl 3: iii10-20.
- Jaiyesimi IA, Pazdur R: Cisplatin and 5-fluorouracil as salvage therapy for recurrent metastatic squamous cell carcinoma of the anal canal. Am J Clin Oncol 1993; 16(6): 536-540.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(8): 11-15.