In current consensus recommendations of the European Hypertension Society. (ESH), the importance of blood pressure measurements outside the physician’s office is emphasized in the context of diagnosis and treatment. For measurements performed at home, the use of validated equipment is critical. With regard to antihypertensive therapy, the treatment algorithm proposed by ESH has proven effective. This gives high priority to combination therapies.
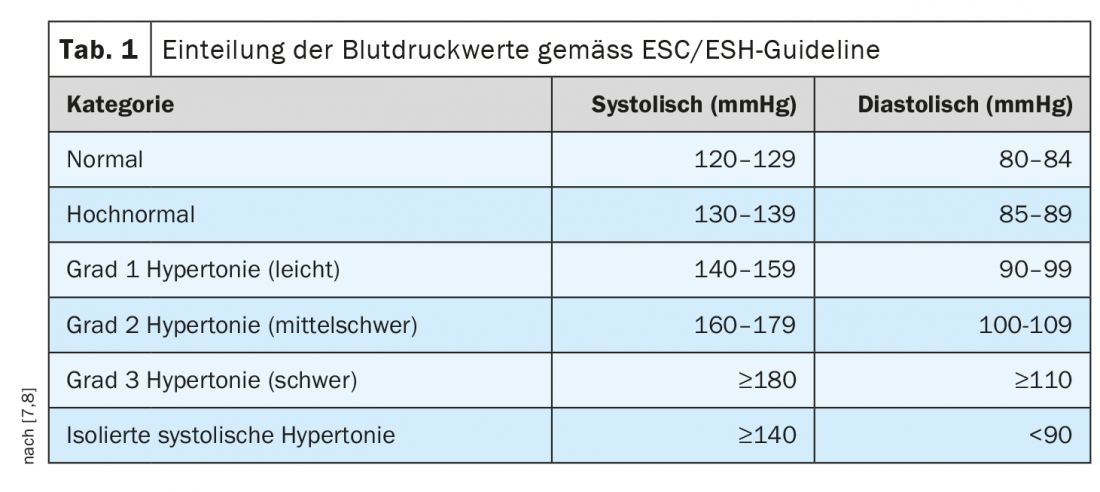
Elevated blood pressure rarely causes symptoms in the early stages but leads to accelerated atherosclerosis and arteriosclerosis in the long term, resulting in organ damage (e.g., heart, brain, kidneys) and associated morbidity and mortality risks [1,2]. In a consensus paper published in 2021, the ESH recommends blood pressure measurements in the home setting, particularly for patients in whom blood pressure values measured in the physician’s office are in the range 140-159/90-99 mmHg, because of possible white coat hypertension, and for those with high-normal values (130-139/85-89 mmHg) because of an increased likelihood of masked hypertension (Table 1) [3]. In order for the measurements to be meaningful, it is advisable that blood pressure measurements at home be performed in as standardized a manner as possible, explained Thilo Burkard, MD, deputy chief physician and head of the hypertension consultation at the University Hospital Basel [4]. Patients should use a validated electronic oscillometric upper arm cuff device. An ESH-endorsed list of blood pressure monitors evaluated according to an established protocol is available at the following Web link: www.stridebp.org [3]. Second, the speaker recommends using a measurement protocol in which patients record morning and evening readings for at least 3-7 days [4]. Two measurements should be taken each time after 5 minutes of rest [4,5]. Providing patients with written instructions for correct blood pressure measurement, as well as a template for a blood pressure protocol, has proven effective, according to the director of the hypertension consultation [4].
“Wearables” for BP measurement currently not sufficiently evidence-based
In connection with blood pressure measurements at home, the question nowadays also arises whether hypertension can be clarified with “wearables,” according to Dr. Burkard [4]. Digital transformation has now entered all areas of life and some of the smartphones and digital gadgets available on the market enable the measurement of vital parameters such as heart rate or blood pressure. The principle of the methodology used is based on the fact that by means of cameras of the mobile devices a photoplethysmographic curve is created and from the shape or change of the curve changes in blood pressure can be tracked. Currently, however, there is a lack of valid studies evaluating the accuracy of the devices and information on how the data collected by the mobile devices correlate with the values measured by traditional means [4]. Therefore, “wearables” for blood pressure measurement are not recommended by professional societies at this time. The conclusion of a consensus paper published in 2022 by an ESH working group is that cuffless blood pressure monitors have great future potential, but fundamental questions about their accuracy, performance, and use should be carefully addressed before they can be recommended for clinical use [6].
|
Combination therapy as therapy standard
|
Hypertension Treatment: ESH Recommends Early Fixed Combination (“Single Pill”)
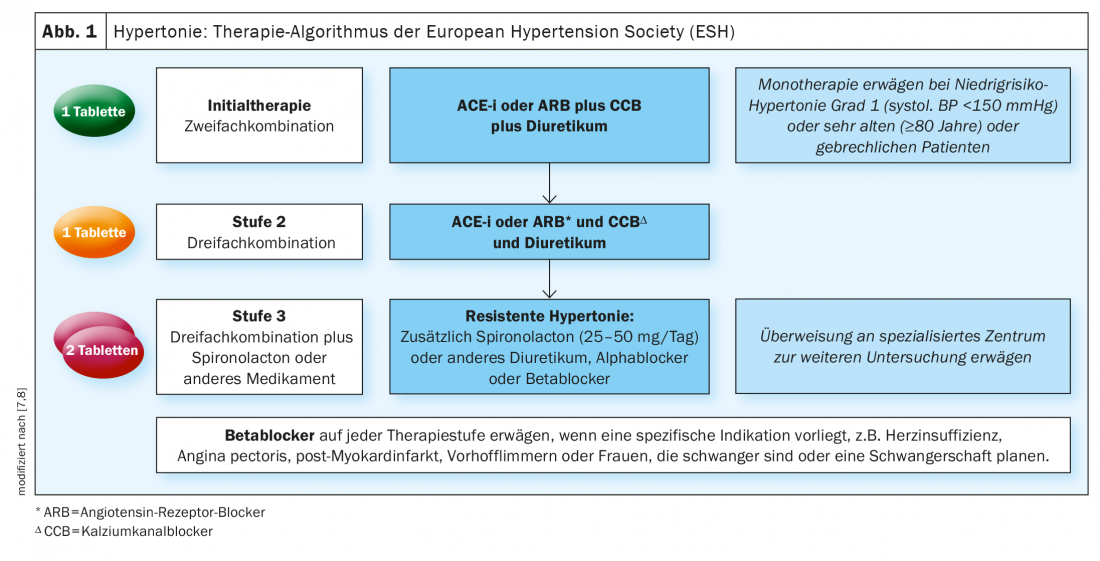
“We actually have a very simple scheme, we have very good preparations on the market,” Dr. Burkard emphasizes. According to current recommendations of the European Society of Hypertension, a dual combination therapy – a RAAS inhibitor plus a calcium antagonist or a RAAS inhibitor plus a thiazide diuretic – is the new standard and should initially be used directly, preferably as a fixed combination (“single pill”) (Fig. 1) [7]. Initial monotherapy should now be considered only in stage I hypertensives and in elderly patients, so it is now the exception (Box). If blood pressure cannot be regulated with a two-drug combination, it is recommended to increase to a three-drug combination, usually a RAAS inhibitor plus a calcium antagonist plus a thiazide diuretic – preferably also as a single tablet [8]. “According to the studies, we can achieve very high control rates like this,” emphasized the speaker [4]. In cases in which hypertension proves resistant to treatment with a triple combination, spironolactone can be added as an add-on.
Why combination therapy should be used has to do with considerations of benefits and side effects, the speaker said. Doubling the dose of a single antihypertensive agent yields only a 20% increase in effect, but significantly more potential for side effects. If you combine two drugs in a smaller dose, you have the full effect of each of the two active ingredients, i.e. an additive effect. “Specific side effects can be reduced by combining them,” the speaker added. For example, combining a RAAS inhibitor with a calcium antagonist can reduce the incidence of leg edema by 30-75%. As shown in a large meta-analysis, “single-pill” regimens have advantages over free combinations in terms of adherence and achievement of blood pressure goals [9].
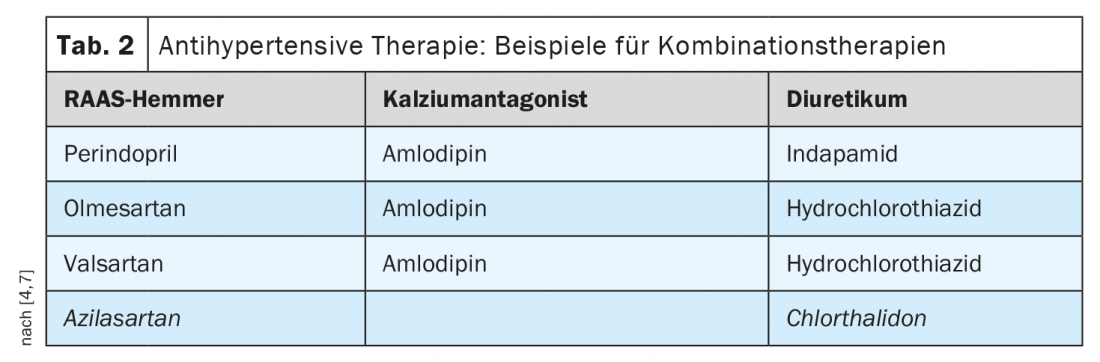
The question remains which drugs to select from the plethora of available active substances [7]. The speaker recommends the selection of combinations shown in table 2, these have proven themselves in practice [4]. Fixed combinations approved in Switzerland include Olmetec® (olmesartan plus hydrochlorothiazide), Sevikar® (olmesartan plus amlodipine), Exforge HCT® (valsartan plus amlodipine plus hydrochlorothiazide) or Coveram® (perindopril plus amlodipine plus indapamide).
Congress: medArt
Literature:
- Olsen MH, et al: A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet 2016; 388: 2665-2712.
- Weber T, et al: Austrian blood pressure consensus 2019. Wien Klin Wochenschr 2019; 131 (Suppl 6), 489-590.
- Stergiou GS, et al: 2021 European Hypertension Society recommendations for in-office and out-of-office blood pressure measurement. Renal and Hypertensive Diseases, vol. 50, no. 11/2021: 490-504.
- “Hypertension,” Thilo Burkard, MD, medArt, medArt June 20-24, 2022,
- Unger T, et al: 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020; 75(6): 1334-1357.
- Stergiou GS, et al; European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2022; 40(8): 1449-1460.
- Williams B, et al; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39(33): 3021-3104.
- Medix: Hypertension, www.medix.ch/wissen/guidelines/herz-kreislauf-krankheiten/hypertonie, (last accessed Sept. 01, 2022).
- Gupta AK, Arshad S, Poulter NR: Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010; 55: 3 99-407.
- MacDonald TM, et al: Combination therapy is superior to sequential monotherapy for the initial treatment of hypertension: a double-blind randomized controlled trial. JAHA 2017; https://doi.org/10.1161/JAHA.117.006986.
- Corrao G, et al. Reduced discontinuation of antihypertensive treatment by two-drug combination as first step. Evidence from daily life practice. J Hypertens 2010; 28: 1584-1590.
HAUSARZT PRAXIS 2022; 17(9): 39-40











