The diagnosis of atypical fibroxanthoma and pleomorphic dermal sarcoma is made as a histologic diagnosis of exclusion. The new guideline published this year summarizes the most important aspects of diagnosis and therapy of these rare neoplasms of the skin.
Atypical fibroxanthoma (AFX) and pleomorphic dermal sarcoma (PDS) typically occur in chronically light-exposed locations, most commonly the capillitium, and rarely other locations such as the forearms or dorsum of the hands [1]. They appear as skin- to flesh-colored, sometimes indurated, and often ulcerated nodules that can be up to several centimeters in size. The surrounding skin usually shows signs of chronic photodamage. AFX is usually a well-circumscribed tumor, whereas PDS may be blurred and often has more aggressive infiltrative growth. The majority of patients have additional skin tumors in the chronically light-exposed skin areas, such as primarily actinic keratoses, basal cell carcinomas and squamous cell carcinomas (PEK), often in the immediate vicinity of the AFX/PDS (field carcinization) [2,3].
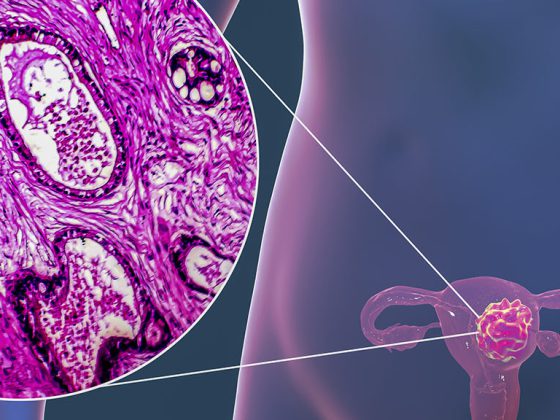
Morphology: atypical spindle-shaped and epithelioid cells
Tumor cell morphology includes a variable spectrum of atypical spindle-shaped and epithelioid cells with pleomorphic, vesicular, or hyperchromatic nuclei, as well as atypical multinucleated giant cells and often atypical mitoses that remain confined to the dermis in the case of AFX, but capture significant portions of subcutaneous adipose tissue or other deeper structures in the case of PDS [1]. Therefore, differentiation between AFX and PDS based on a superficial biopsy is not possible. A deep spindle biopsy must be performed to make a definitive diagnosis. Unlike AFX, PDS are more indistinctly demarcated, more aggressively infiltrating neoplasms with invasion of the subcutis, skeletal muscle, and/or fascial structures. Furthermore, tumor necrosis, lymphovascular infiltration, and/or perineural infiltration may be present, which is not the case with AFX. The tumor stroma may show myxoid, desmoplastic, or keloid changes. In addition to infiltration of deeper structures, lymphovascular or perineural invasion and the presence of zones of necrosis have been associated with a more aggressive clinical course [4–7].

Immunohistochemistry Diagnosis of exclusion
Because of the nonspecific histology, diagnosis requires immunohistochemical exclusion of other tumors such as dedifferentiated cutaneous PEK, melanomas, vascular tumors, and other sarcomas, as well as reticulohistiocytomas and atypical fibrous histiocytomas [2]. To exclude these differential diagnoses, an immunohistochemical panel of at least two melanocytic markers (such as S100, Sox10), two cytokeratin markers (such as AE1/3, MNF116, KL1, or CAM5.2), and one muscle marker (desmin), supplemented if necessary by additional markers such as CD10, a vascular marker (CD34, ERG), or additional myocytic markers (alpha-smooth muscle actin, α-SMA) is recommended [4,8,9]. The treatment of choice is microscopically controlled surgery [1]. In AFX, healing can be assumed after complete excision. As far as PDS were operated with a safety distance of 2 cm, the local recurrence rate is also low. Locoregional metastases may occur in very thick or incompletely excised tumors; distant metastases rarely occur. No approved effective drug therapy is known to date [1].
Literature:
- Helbig D, et al: S1 guideline atypical fibroxanthoma (AFX) and pleomorphic dermal sarcoma (PDS). JDDG 2022; 20(2): 235-245.
- Calonje E, et al: Spindle-cell non-pleomorphic atypical fibroxanthoma: analysis of a series and delineation of a distinctive variant. Histopathology 1993; 22: 247-254.
- Li YY, et al: Genomic analysis of metastatic cutaneous squamous cell carcinoma. Clin Cancer Res 2015; 21: 1447-1456.
- Luzar B, Calonje E: Morphological and immunohistochemical characteristics of atypical fibroxanthoma with a special emphasis on potential diagnostic pitfalls: a review. J Cutan Pathol 2010; 37: 301-309.
- McCalmont TH: Correction and clarification regarding AFX and pleomorphic dermal sarcoma. J Cutan Pathol 2012; 39: 8.
- Miller K, Goodlad JR, Brenn T: Pleomorphic dermal sarcoma: adverse histologic features predict aggressive behavior and allow distinction from atypical fibroxanthoma. Am J Surg Pathol 2012; 36: 1317-1326.
- Henderson MT, Hollmig ST: Malignant fibrous histiocytoma: changing perceptions and management challenges. JAAD 2012; 67: 1335-1341.
- Hall JM, Saenger JS, Fadare O: Diagnostic utility of P63 and CD10 in distinguishing cutaneous spindle cell/sarcomatoid squamous cell carcinomas and atypical fibroxanthomas. Int J Clin Exp Pathol 2008; 1: 524-530.
- Tardio JC, et al: Pleomorphic dermal sarcoma: a more aggressive neoplasm than previously estimated. J Cutan Pathol 2016; 43(2): 101-112.
DERMATOLOGIE PRAXIS 2022; 32(5): 55