Surgical remediation of hypercalcemia caused by parathyroid dysfunction remains a special chapter in surgery. The frequency of “frustrated explorations,” i.e., unsuccessful search for an adenoma of the parathyroid glands in hyperparathyroidism, is between 1% and 5%. Specialization is in demand.
Surgical remediation of hypercalcemia caused by parathyroid dysfunction remains a special chapter in surgery and is readily left to the specialist. Primary hyperparathyroidism (pHPT) is usually due to a solitary adenoma of one of the four parathyroid glands. More rarely, hyperplasia of all four glands is present, mainly in genetic disorders.
Surgical management of hypercalcemia is primarily curative. Cure rates reach at least 98% in specialized centers. Nevertheless, 5-10% of all patients, especially from less specialized institutions, experience either persistence or recurrence of the disease. This is caused by either an overlooked adenomatous parathyroid gland or hyperplasia of all four glands.
Through progressive specialization and ever-improving localization diagnostics, it is now possible to a large extent to correctly locate and remove the enlarged parathyroid gland leading to hypercalcemia with surgical exploration of the appropriate regions of the neck (Fig. 1). Thus, frustrated exploration in pHPT is becoming increasingly rare. However, the management after a frustrated surgery, the indication for a revision surgery, the necessary localization diagnostics beforehand and the intraoperative procedure are still very challenging.
Specialization
The specialty of “Endocrine Surgery” has developed because the special problems of glandular diseases require a high degree of knowledge. This is especially true for the enlarged parathyroid glands and, in particular, for the variables of their anatomical position in the cervical region. Both the size and the nature of the gland can vary greatly. Understanding about the endocrine diseases that require surgical therapy has given rise to the specialty of “Endocrine Surgery”:
– Requirements in “Surgical Endocrinology” (Endocrine Surgery):
- Knowledge of the variability in the nature and location of the organs
- Knowledge of the individual radicality of the operation
- Knowledge of recurrence prevention to the fullest extent of surgical options.
- Knowledge of the physiological relationships and genetic causes of endocrine diseases.
Preoperative aspects of primary hyperparathyroidism.
Once the diagnosis has been confirmed by laboratory chemistry, the indication for surgical sanitation must be clearly defined on the basis of the symptom complex.
Symptomatic forms (renal, osteologic, neurologic, hypercalcemic symptoms) still present a clear, especially immediate indication. Observations of the oligo- or “asymptomatic” forms tend to result in deterioration, especially increases in blood pressure.
Whether a particular algorithm should be initiated to identify the adenoma in the presence of hypercalcemia is by no means uniformly regulated. Numerous centers with high experience are content to confirm the diagnosis by laboratory chemistry and operate without further imaging. More important, he said, is to have the surgery performed by an endocrine-savvy surgeon. This is justified by the fact that hyperparathyroidism is almost always caused by an orthotopically located adenoma and is therefore readily available to the specialist. If the orthotopic positions were explored, then expertise in exploring the ectopic positions would be sufficient to successfully complete the surgery. Only very rarely are unsuccessful operations to be accepted.
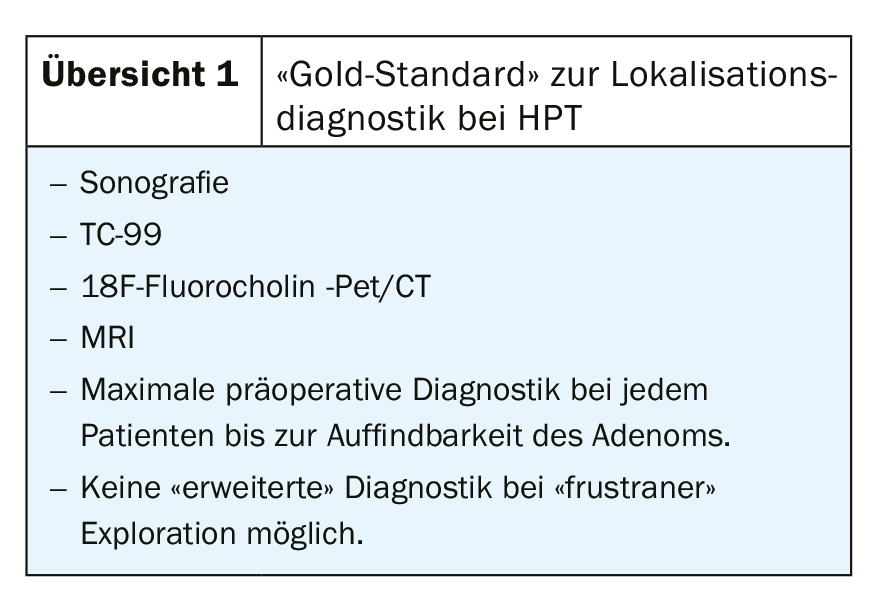
However, it has become accepted that the capabilities of modern diagnostics are fully applied in substance to provide the surgeon with maximum precision in finding the adenoma. Blind exploration causes significantly higher complication rates and potentially unsuccessful surgery. The diagnostic algorithm – after confirming the diagnosis – consists first of all of laboratory, ultrasound, scintigraphy, usually Tc-99-mibi, possibly MRI.
Usually, diagnostics are stopped there when functionally active tissue is clearly detected. However, repeat and supplementary examinations are very often performed even though the localization has already been determined.
In general, the entire program of localization is usually applied, so that in the event of a frustrated exploration, prior to a revision procedure, there is then no method in reserve that has not yet been performed.
It must be stated that the indication for a neck exploration is already given by the clinical and laboratory confirmation of a pHPT and does not depend on the outcome of the morphological and functional examinations. It happens that clearly indicated explorations are omitted because the localization diagnosis remains negative. In such a situation, no discontinuation of treatment or controls are necessary, but immediate referral to an endocrine surgery center where the appropriate expertise exists for successful surgery despite negative preliminary tests.
Future
Modern functional topographic examination methods, e.g. 18Fluorocholine, Pet, CT, improve the preoperative localization possibilities and enable precise targeted exploratory surgery. Recent reports on the use of intraoperative fluorescence imaging also appear promising for reducing the number of “occult” (undetectable) pathologic parathyroid glands.
The “frustrating exploration
Despite the use of modern tools for localization (e.g., 18F-fluorocholine or intraoperative fluorescence), “frustrated” neck exploration may occur. This means that either – despite positive localization diagnosis – the adenoma is not found intraoperatively, or that in the absence of localization (so-called “occult” adenoma) no adenoma or 4-gland hyperplasia can be identified. This is becoming increasingly rare, but remains challenging.
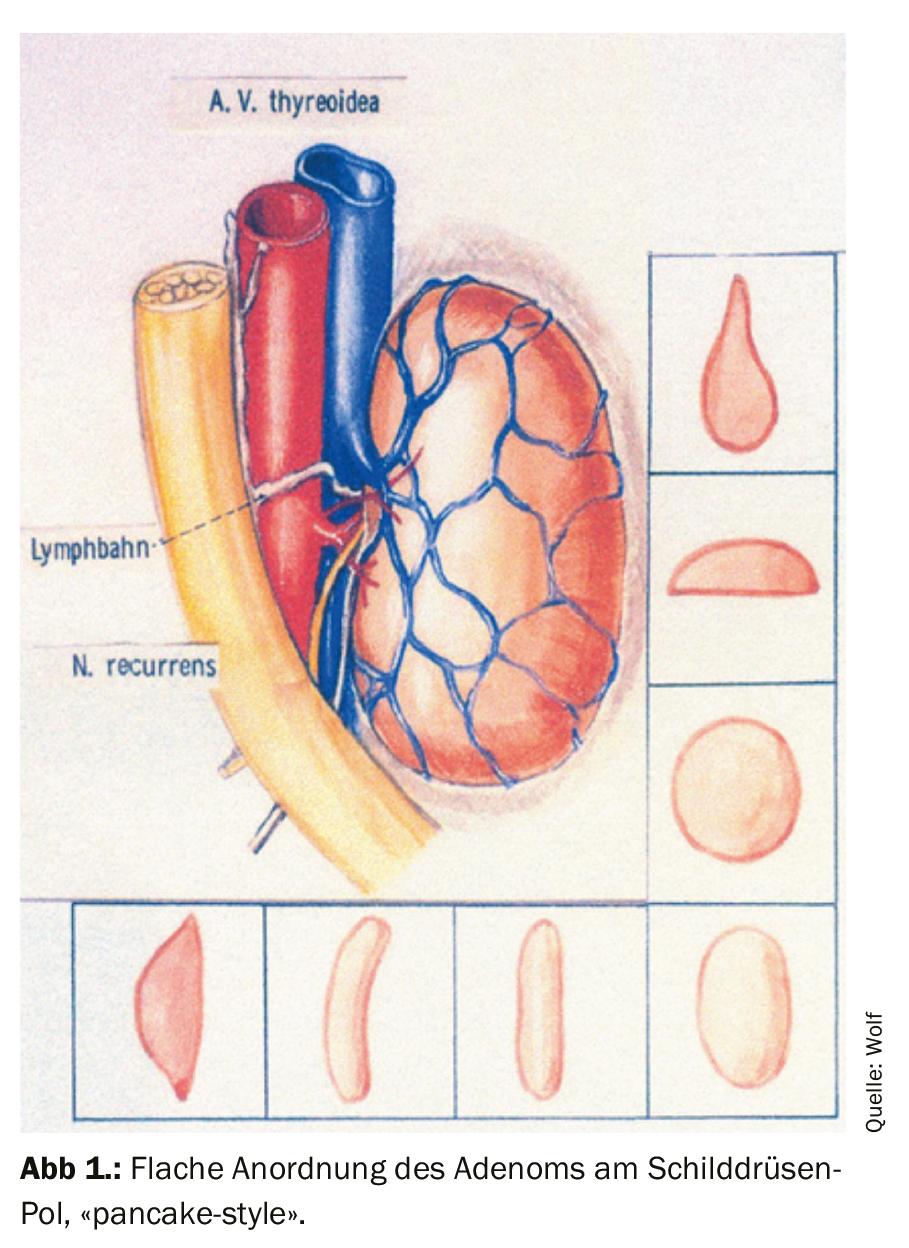
The reason for an overlooked adenoma on sonography and a negative scintigraphy may be that the NSD adenoma lies flat against the thyroid gland or the usual fatty lamina between these two glands is absent and leaves no space between them, so that ultrasound cannot detect the thin parenchymal layer as an adenoma. Similarly, a flat spread adenoma may be completely outshone by the thyroid gland on scintigraphy (so-called pancake-style adenoma).
Causes of unsuccessful surgery:
- An “overlooking” of an existing gland.
- Intraoperative misinterpretation; thymic remnant, thyroid gland.
- Flat arrangement of the adenoma against the thyroid (“pancake style”) or by elongated shape along the art. thyr. inferior).
- Confusion with a nodule of the thyroid gland.
- Inaccessibility in the mediastinum if no primary sternotomy was scheduled and cleared.
This can occur in 5-10% in different institutions, especially when no occlusive diagnosis was possible preoperatively. However, in specialized centers, the success rate (identification of the adenoma despite negative diagnosis) is up to 98%. This is another argument for specialization in this field.
Guidelines on when to stop a neck exploration do not exist, but it is strictly recommended to avoid complications especially on the recurrent nerve. Thus, when all ortho- and ectopic regions have been subtly dissected to no avail, the recommendation is to stop the procedure and perform a re-evaluation. Likewise, a questionable lesion of the lar. nerve. recurrens or a loss-of-signal in neuromonitoring are reasons to stop the procedure.
These patients require careful continued care and appropriate observation of their disease. Most importantly, another clear indication for revision surgery needs to be developed. The decision to re-operate follows an appropriately defined algorithm.
Further procedure after frustrated exploration
If the adenoma was not detectable at the initial surgery, the following algorithm is used today:
- Strict observance of renal and osteologic symptoms.
- If possible, 3 to 6 month interval and re-evaluation of all localization diagnostics.
- Immediate re-operation in case of positive findings.
- Further intervals 3(-6) months.
- Repetitive, multiple localization diagnosis until detectable.
Ultrasound and Tc-99 sestamibi have sensitivities of 72% to 87% and 54% to 90%, respectively, in this situation.
In principle, the indication for revision surgery is as follows: If the indication for an intervention was primarily present, then this is also unchanged for a revision intervention. Nevertheless, there are several criteria to consider for this subtle second operation. The risk/benefit ratio is dramatically biased against surgery if the localization diagnosis remains negative.
Special problem of neck exploration in pHPT.
Remediation of hypercalcemia remains a subtle procedure that requires high surgical care and knowledge. The operation takes place at a surgically challenging site in the body, nearby structures such as the vocal cord nerve (N. laryngeus Recurrens), Art. Carotis, esophagus or thoracic duct require precise, tissue-sparing surgery. Complications that hit these structures lead to serious disorders and even catastrophic courses.
Anatomical variable
Removal of a solitary adenoma of the parathyroid gland in hypercalcemia is not a major procedure per se if the adenoma is located loco typico. However, the high number of variables still leads, in the absence of knowledge, to frustrating exploratory operations on the neck. The rarer cause of hyperplasia of all four glands, especially in genetic diseases, requires multiglandular exploration as well as tissue reduction leaving a parenchymal residue, possibly with re-transplantation of previously removed parts of the gland (“auto-transplantation”). This requires individualized indication and laboratory chemistry tools (so-called Quick-PTH; intraoperative PTH rapid test) [1,5]. However, a high level of knowledge of the interpretation possibilities of this method is required. In most cases, its use is not goal-directed because the flow conditions at the perithyroidal venous plexus vary greatly after dissection and do not permit precise topographical assignment. Only for determining which side of the neck has an elevated level of PTH, thus allowing unilateral exploration, it should be defined as a true tool.
Specific complication possibilities
Lesion of the laryngeal recurrent nerve (vocal cord nerve) is a Mayor complication of thyroid and parathyroid surgery. Their frequency is virtually the measure of the quality of the operation. With appropriate visualization of the adenomatous gland in preoperative diagnosis, the risk of lesion is low, even if the nerve and the parathyroid region are in close contact. Appropriate anatomical knowledge and the obligatory identification of all structures in the surgical area keep the risk low in this situation. Technical aids (“neuromonitoring”) for electrophysiological control of the conductivity of the nerve during surgery further reduce this risk. However, a lack of expertise, with a lack of experience, can make even this situation, which is clear in itself, difficult – and frustrating.
Diagnostics before primary intervention
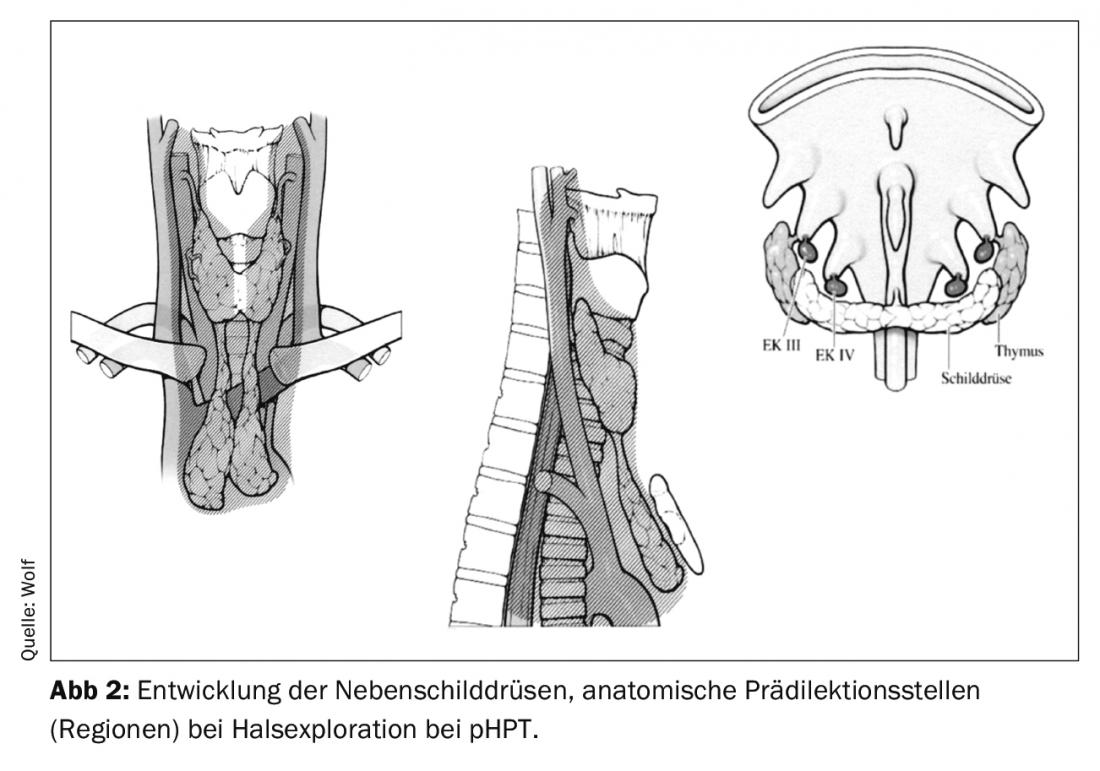
Now, if – with a confirmed diagnosis of hyperparathyroidism with hypercalcemia – an adenoma escapes preoperative examination and thus the adenoma must be “searched for,” then bilateral neck exploration is required. This must then be performed at all “orthotopic” locations as well as at the “ectopic sites” (along the possible location after embryonic development) (Fig. 2).
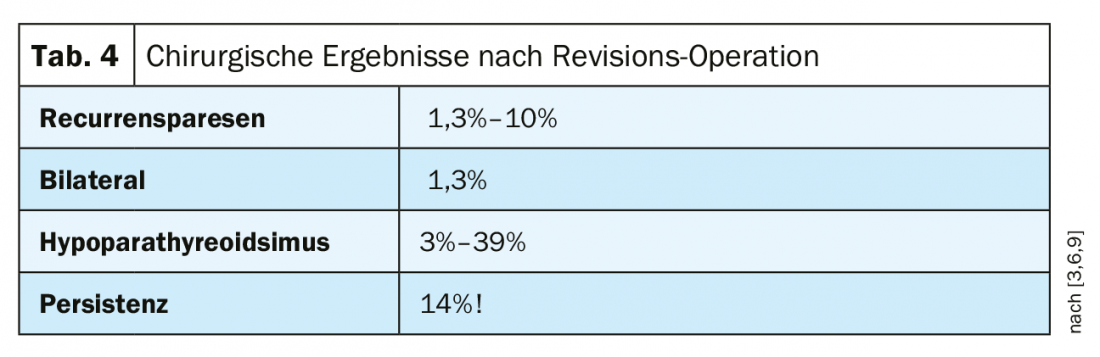
The extent of the surgical area is enormous, and the exposure of the cervical fascial spaces, including the mediastinum if necessary, means a considerable risk of a complication occurring. Bilateral neck exploration for “occult” (non-demonstrable) adenoma is the neck surgery with the highest risk of voice dysfunction. Exploration per se is laborious, there is a great constraint to success and, above all, the need to seek out and safely assess all possible positions of the adenoma. This is one reason why this operation is preferably left to the specialist. However, even in the hands of the specialist, damage to the recurrent nerve is a complication that cannot be excluded and foreseen, and this has a significant impact on the assessment of the indication for surgery when considering the overall approach, algorithm in the treatment of parathyroid hyperfunction (especially in the case of negative presentation).
Procedure after frustrated exploration
Non-operative management: Basically, it is postulated today that there is actually no such thing as an “asymptomatic” HPT, but that HPT-specific changes are always found upon close evaluation. Often, neurological symptoms are also not appropriately appreciated. In the course after a negative neck exploration in HPT, patients with mild oligosymptomatic courses can undoubtedly be treated observationally. In patients with symptomatic course and biochemically significant disease who refuse reoperation or in whom co-morbidities make the surgical risk very high, drug therapy may also be considered. Options include bisphosphonates, which inhibit bone resorption, or cinacalcet, a calcium mimetic that lowers PTH and, consequently, calcium levels.
In principle, however, consistent preparation for curative surgery is the method of choice in such a situation.
Preoperative indication and preparation for revision surgery
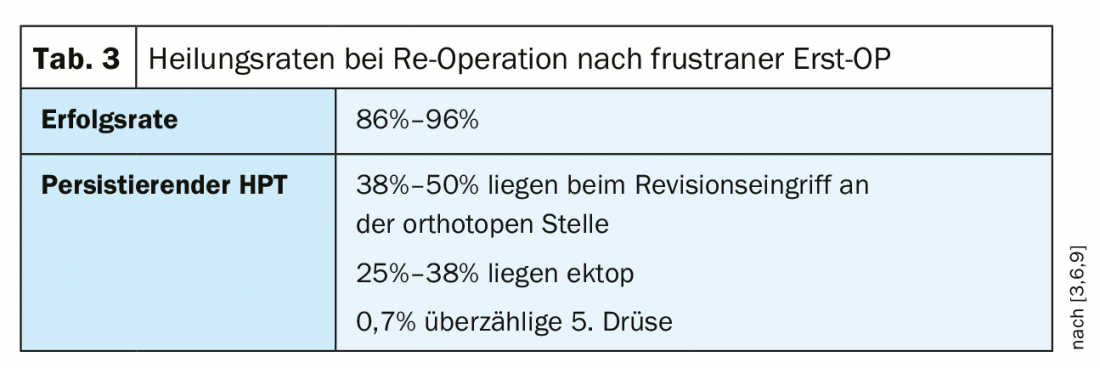
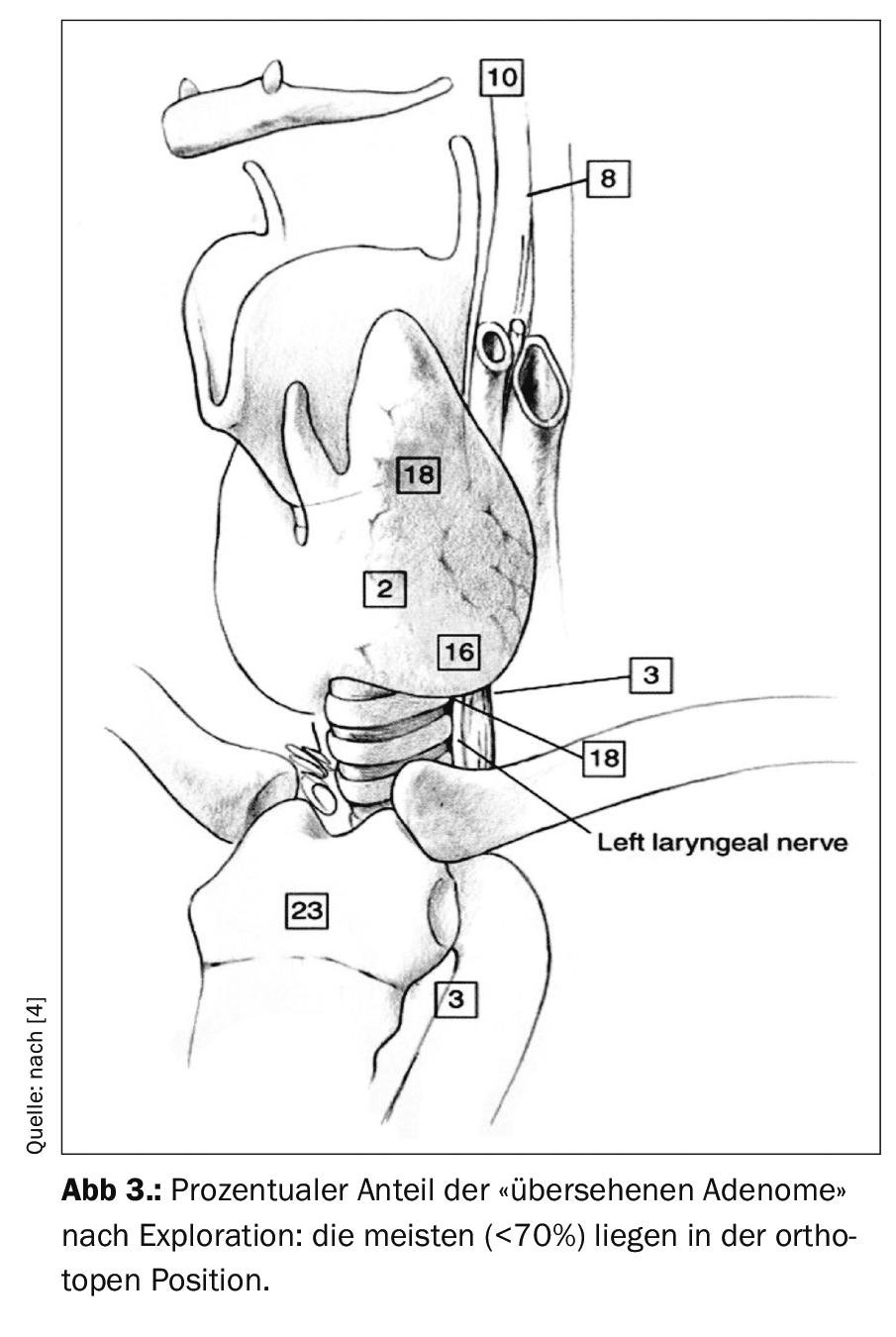
Re-operation after frustrated initial surgery: pHPT is caused by a solitary adenoma in 80-90%. It follows that a single adenoma is also present as the cause of persistence in 57-83% with frustrated initial exploration, and that this was in the orthotopic position in 50-70%. Figure 3 shows that the majority of “overlooked” adenomas are present in their eutopic position.
Re-operation requires careful indication and planning. Accurate knowledge of the results of the initial surgery, the regions explored, the number and location of glands identified or left in place, and the function of the recurrent nerve bds. is absolutely necessary. The entire repertoire of localization diagnostics, from the skull base to the mediastinum, is to be applied. Of course, it is advantageous if one of these investigations is positive and re-exploration can be carried out in a targeted manner. If this localization is negative, the risk/benefit ratio clearly and massively shifts against surgical intervention. Nevertheless, it may be essential in case of impending hypercalcemic crisis or massive symptomatic HPT. In principle, surgery should not be performed until a surgical target is present.
Preoperative localization after unsuccessful initial surgery
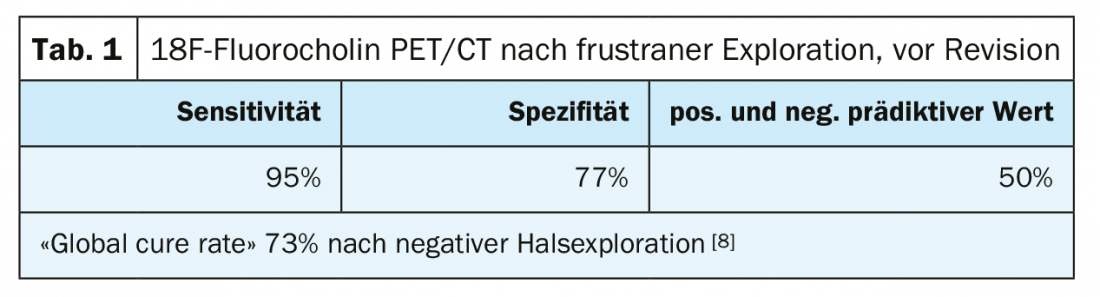
Positive localization is of utmost importance, but not always achievable. It is recommended to repeat the diagnostic procedure until a result is available, if the clinical course allows it. In the literature, the rate of positive localization before reoperation is only 73%, and the sensitivity of ultrasound and Tc-99 mibi is 72% to 87% [4]. 18F-fluoro-choline improves the results, but still the cure rate remains only 73% [8].
Conclusion
The indication for re-operation: the indication for persistent HPT is not always clear-cut, it is the increased difficulty of re-operation coupled with lower success rate. The risk/benefit ratio favors re-operation in the presence of significant symptoms (recurrent nephrolithiasis, osteopenia, or impending hypercalcemic crisis). In patients with mild oligosymptomatic disease, the risk of surgery is greater than the benefit. The rate of re-frustrated surgery can be as high as 50% [2]. These patients are candidates for conservative management.
Take-Home Messages
- The frequency of “frustrated explorations,” i.e., unsuccessful search for an adenoma of the parathyroid glands in hyperparathyroidism, is between 1% and 5%.
- The rate decreases sharply with improved scintigraphic tools (18F-choline) or intraoperative fluorescence and with professional specialization by the “endocrine surgeon.”
- Only the “mild,” oligo- or asymptomatic HPT should be treated observationally.
- Symptomatic HPT (nephrolithiasis, osteopenia, neurologic symptoms) or impending hypercalcemic crisis absolutely require revision surgery.
- The second operation should be considered only if the localization is positive, otherwise the risk of a frustrated revision can be up to 15%.
Literature:
- Reiher AE, Schaefer S: Final intraoperative PTH level. Ann Surg Oncol 2012; 19(6): 18862-18867.
- Charlett SD, Aye M, Atkin SL: Defining failure after parathyroidectomy for primary HPT. J.Laryngol, Otol 2011; 25(4): 394-398.
- Shin JJ: Impact of localization studies and clinical Scenario in Patients with HPT. Arch Surg 2011; 146(12): 1397-1403.
- Powell AC, et al: Reoperation for parathyroid adenoma: a contemporary experience. Surgery 2009; 146(6): 1144-1155.
- Karakas E, et al: Reoperation for Primary Hypeparathyroidism. Surgeon 2005; 76(3): 207-216.
- Hessman O: High success rates of parathyroid reoperation may be achieved with improved localisation Studies World J Surg 2998; 32(5): 774-781.
- Mortensen MM, et al: Parathyroid exploration in the reoperative neck: improved preoperative localization with 4D computed tomography. J Am coll Surg 2008; 206(5): 888-896.
- Corelle A: WJS 2019; 43: 1232-1242.
- Dotzenrath C: Langenbecks Arch. Chir. 379: 218
- Michaud L: Medicine 2013; 94; 91.
HAUSARZT PRAXIS 2020; 15(1): 10-14