Defects of the immune system can have devastating consequences [1]. However, because the symptoms are very diverse, the diagnosis of primary immunodeficiency often occurs late [2]. However, early detection is essential to initiate adequate therapy and to decisively improve patients’ quality of life, as Prof. Mike Recher of the University Hospital Basel explains in the following interview.

Prof. Mike Recher
Senior physician and head of the consultation for primary immunodeficiencies
FMH Internal Medicine/Allergology and Clinical Immunology
Medical Polyclinic
University Hospital Basel
What is primary immunodeficiency?
Immunodeficiency means that the immune system does not function properly. Basically, our immune system has two tasks: Firstly, protection against infections and secondly, immune tolerance. In the case of immunodeficiency or immunodeficiency, at least one of these tasks cannot be fulfilled, often even both. When the patient presents or the first examinations are performed, it is usually not known whether the immunodeficiency is primary or secondary. Primary immunodeficiency means that the cause of the immunodeficiency is genetic. Often, however, the underlying genetic changes are not known or would have to be searched for years. Only in individual cases is the genetic basis for the immune system’s inability to perform its tasks known. In contrast, in secondary immunodeficiency, the immunodeficiency is not congenital but due to an external factor. A classic example of this would be HIV or the measles virus, where immune deficiency occurs after infection. Beyond that, however, there are countless other factors. Thus, secondary immunodeficiency is a broad term and occurs primarily in adults.
What signs should an attending physician think about immunodeficiency?
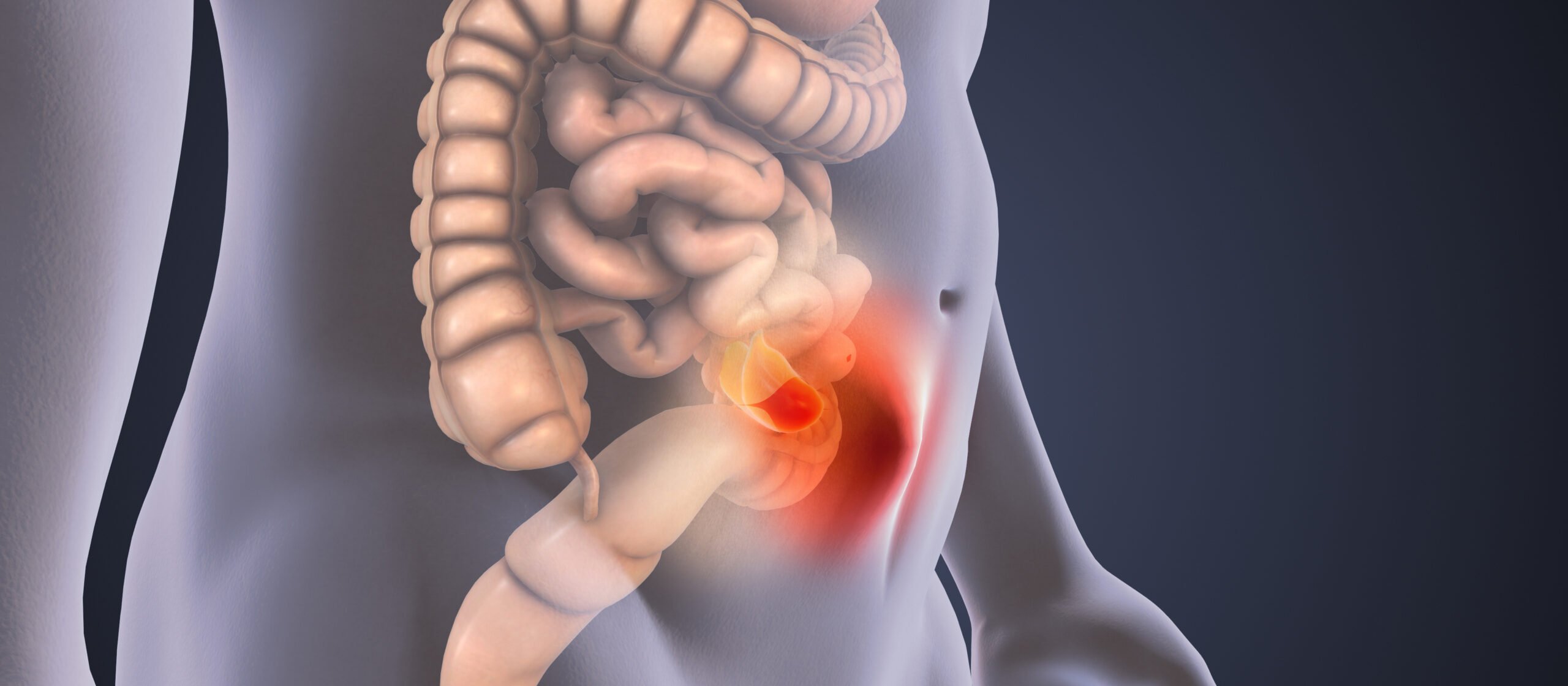
I always tell my patients that humans have about 20,000 genes, which can be thought of as building instructions for various components in a mechanical watch. Each individual gene is a blueprint for such a component and if any one of these parts is not working properly, then the clock is not running properly. Of the 20,000 genes, about 3,000 to 5,000 genes have a role in the immune system. Consequently, every fourth complaint of a patient is possibly caused by the immune system. Of course, this is formulated somewhat mathematically, but it is intended to show that the alarm symptoms are extremely diverse. A classic example would be a patient who has recurrent colds, such as multiple pneumonias, recurrent sinusitis, or prolonged bronchitis. However, this is far from being the only symptomatology. Chronic diarrhea, for example, can also indicate an immune deficiency, as can an enlarged spleen or enlarged lymph nodes. Likewise, there are patients in whom changes in the blood count, dyspnea, or elevated liver enzymes are the first manifestation. In addition, the question always arises in oncology: Could the cause of a cancer, such as lymphoma, possibly be a defective immune system? All in all, therefore, there is a wide variety of symptoms that can indicate an immune deficiency.
|
10 warning signs of primary immunodeficiency in children
See Jeffrey Model Foundation: |
When should an attending physician refer a patient to your consultation?
There is a simple test to determine the immune system’s defense capacity that any family doctor or pediatrician can perform. For this purpose, blood is taken and analyzed in the laboratory for immunoglobulins – IgG, IgM and IgA – in the serum. The analysis does not require a special laboratory and is also very inexpensive at about CHF 6. Therefore, measurement of immunoglobulins should really be offered in a very low-threshold way. I am always amazed at how little this is done – sometimes even in patients in hospital who are clearly suspected of having an immune disorder. Immunoglobulins can be measured very well and have very clear normal values. Normal serum immunoglobulin levels do not rule out immunodeficiency, but when levels deviate from normal, a diagnosis of immunodeficiency is made. In this case – if it is not exactly clear what is behind it – a referral to a specialist makes sense. This is because it is known that the life expectancy of patients with immune insufficiency may be reduced. Compared with diabetics, for example, patients with immunodeficiency also have a poorer quality of life, as has been demonstrated in studies. Therefore, one should not wait with a clarification.
How do you proceed when a patient is referred to you?
As usual in a consultation, the first thing you do is listen to the patient’s whole story. Why is he here now? Why was he assigned? This is usually followed by a physical examination focusing on the immunological organs. This includes palpation of accessible lymph nodes, i.e., under the armpits, by the groin, and on the neck, to detect abnormal enlargement. The spleen in the left upper abdomen is then examined, which should not normally be felt. If it does, it is enlarged. In addition, there are certain other findings, such as skin inflammation, that are clustered in patients with immune disorders. Therefore, one always looks at the skin, the hands, for example, could have viral warts. By means of eye diagnosis on the elbows, on the other hand, an allergic tendency can be concluded. In addition, one listens to the heart and lungs. Furthermore, additional laboratory tests are made, which check the function of the immune system.
What does the diagnosis of “primary immunodeficiency” mean for the child?
Immune disorders can vary widely in terms of severity. In the most severe form, the child is at risk of dying from a severe infection. In such a case, you need to act quickly. So there are immunodeficiencies where you should actually replace the bone marrow immediately. Therefore, since 2019, every newborn will also be screened for such severe defects in the heel blood that is drawn. More often, however, a child is simply often cold and sick. It is more vulnerable, may also need to go to the hospital for pneumonia. Another sign is that the child is not gaining enough weight or has gastrointestinal symptoms, such as the chronic diarrhea mentioned earlier. However, the focus need not always be on the tendency to infection; blood count changes may also be involved. Anemia, for example, manifests itself as shortness of breath, or skin bleeding and nosebleeds occur when there are too few platelets. Thus, even in childhood, the clinical presentation is very diverse.
In your experience, what are the biggest challenges around primary immunodeficiency?
An important point is still the transfer of knowledge about these disorders. On the one hand, this must be communicated to the general population. On the other hand, it is also important to inform primary care providers that these types of conditions exist. This makes sense especially because there are very effective therapies for immunodeficiencies. An important therapeutic approach is the substitution of immunoglobulins. This immune protection must be administered again and again, because it is broken down over a period of several weeks. In this way, infections can now be well controlled or even prevented in patients who previously would have died from recurrent pneumonia. Due to regular immunoglobulin infusions, most patients have a normal life expectancy.
What else would you like pediatricians and primary care providers to know about this topic?
As I said, the biology of the immune system is already influenced by so many genes that it is very likely that immune disorders are also common in pediatricians and primary care. “He or she is somewhat susceptible,” as people used to be fond of saying, is really just the clinical term for an immune deficiency that has not yet been discovered. There are patients who have had to wait 69 years or more from the first symptom until the correct diagnosis is made and adequate therapy is initiated. All I can say is keep this in mind. Screening for immunodeficiencies is simple, inexpensive, and has a positive impact on life expectancy as well as patient quality of life.
Literature
This article was written with the financial support of Takeda Pharma AG.
C-ANPROM/CH/CUVI/0008 05/2021
Contribution online since 09.06.2021