Catheter-based therapy for vascular disease has changed significantly in recent years. Rapid technical progress and greater clinical experience now allow recanalization of even severely calcified and long-stretch arterial occlusions. A range of catheters allows active elimination of thrombotic and embolic pathologies, so that complex procedures that were technically infeasible a few years ago can now be performed safely.
Interventional angiology has again made strong progress in recent years. Although wire, balloon catheters and manometers are still the most important utensils of the interventionalist, they have evolved to such an extent that interventions are now feasible that were thought to have reached the horizon a few years ago.
That there is more going on beyond the horizon has been impressively demonstrated by the development of refined wires, “re-entry” devices [1], ultra-thin lubricious balloon catheters, atherectomy devices, lysis and aspiration catheters. At the same time, interventional procedures have also become significantly more demanding and take up much more time and resources.
The problem today is not so much to recanalize long-standing occlusions, but to keep them open for a longer period of time. Many questions remain unanswered: platelet function inhibition with monotherapy? Dual platelet function inhibition? Anticoagulation? If so, with what? Large randomized trials similar to those in cardiology are practically non-existent, so here in Switzerland we are guided by expert opinion [2] or cardiology intervention studies. But there are also developments emerging in the pharmacological sector that we expect will significantly reduce this problem in the future. New platelet function inhibitors act more specifically at those sites where their effect is needed [3].
In the following article, we would like to present a few exceptional cases from our daily practice that are representative of the new developments.
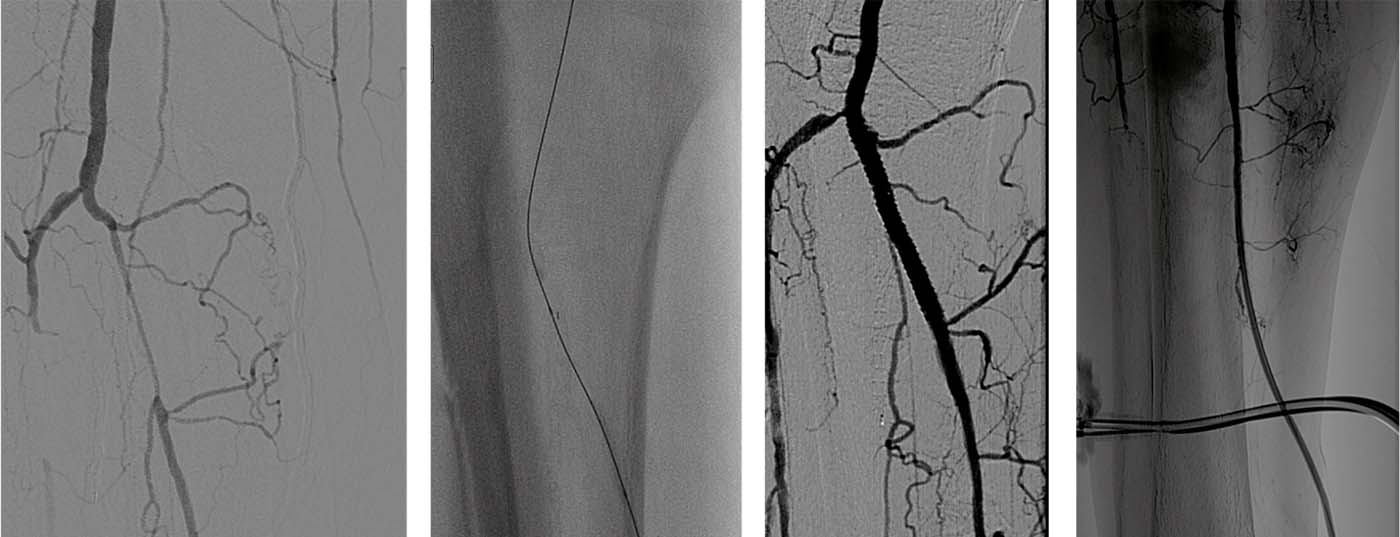
Case 1
This was an 84-year-old female patient with critical ischemia of the right leg, rest pain for three weeks, multiple ulcerations on the right lower leg and foot, right ABI of 0.3, duplex sonographic long-stretch occlusion of the right superficial femoral artery, and minimal postocclusive flow in the popliteal artery. The lower legs cannot be assessed conclusively. Angiography the next day confirms duplex sonography.
- Retrograde puncture of the left common femoral artery was performed. Review angiography of the iliac arteries illustrates that they show no relevant stenosis. There is complete, long-stretch occlusion of the right superficial femoral artery (Fig. 1a).
- The popliteal artery is severely sclerotically altered with multisegmental stenoses (Fig. 1b).
- On the lower leg, there is a severely sclerotized anterior tibial artery with multisegmental stenoses, a severely sclerotized fibular artery with multisegmental stenoses, and occlusion of the posterior tibial artery (Fig. 1c).
- A sophisticated recanalization with multiple CTO wires is performed. Multiple overlapping dilations of the entire AFS follow. Control angiography after multiple balloon angioplasties showed a patency but still multisegmentally stenosed superficial femoral artery ( femoralis superficialis) (Fig. 1d).
- This is followed by implantation of a 5/200 mm SMARTflex stent, an EverFlex 6/150 mm stent, and a Pulsar 6/150 mm stent. The entire section is post-dilated several times overlapping with a 5/100 mm balloon (Fig. 1e).
- Follow-up angiography after PTA and stenting showed significantly better outflow to the lower leg (Fig. 1f).
- After a procedure time of 3.5 hours and a fluoroscopy time of 58 minutes, the puncture site is closed with a StarClose. The patient can be discharged to home care the next day, and there is no longer any rest pain. After three months, all ulcerations have healed (Fig. 1g).
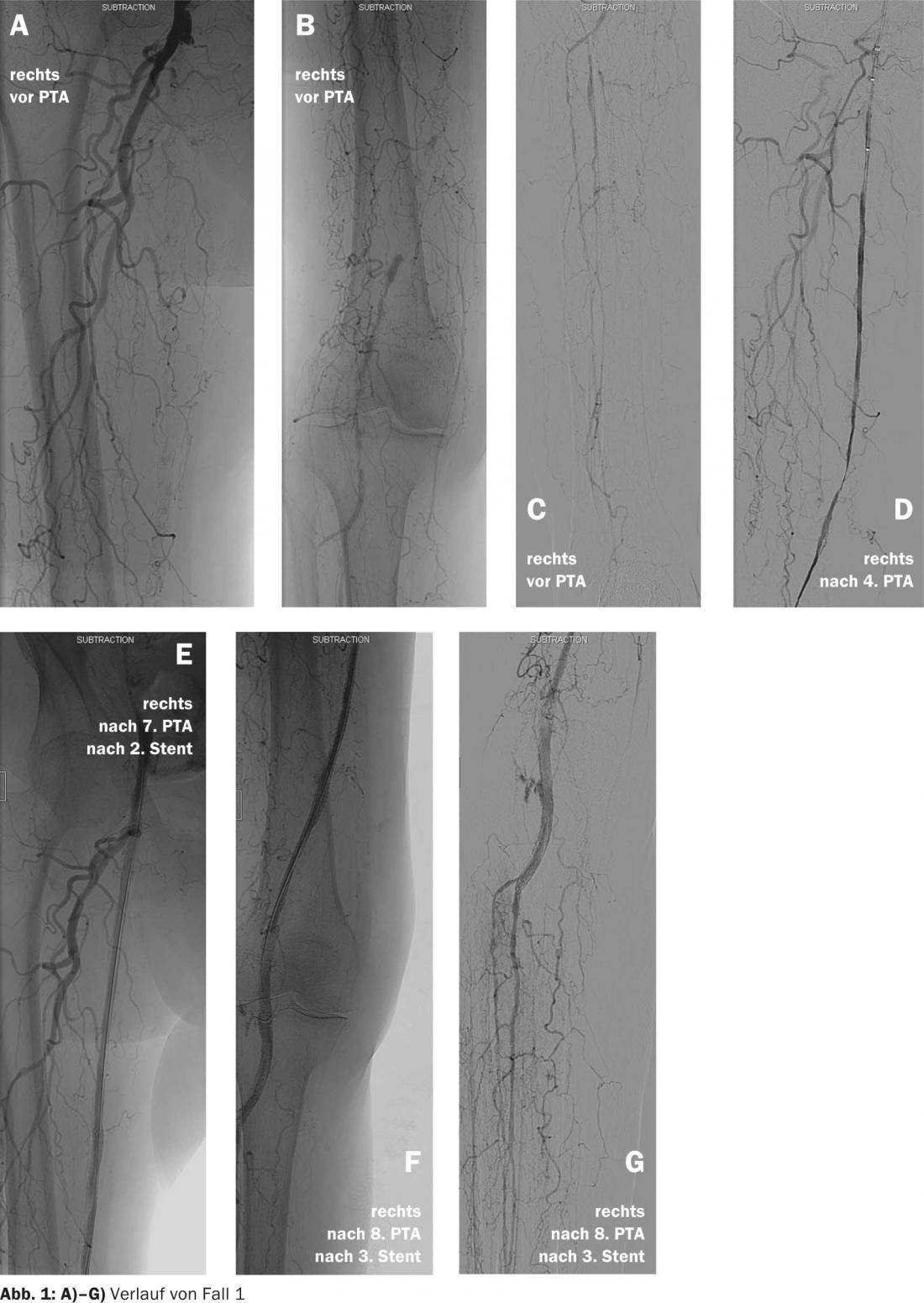
Case 2
This is a 73-year-old patient with critical ischemia of the right lower extremity. The ABI is not usable because of mediasclerosis. Duplex sonography revealed high-grade stenoses of the external iliac artery, common femoral artery, and superficial right femoral artery. The transtibial arteries cannot be assessed conclusively in the presence of marked calcifications. The pelvic floor, AFC, and AFS were dilated at an out-of-town hospital.Due to persistent rest pain, the patient is referred to our clinic.
- Survey angiography shows successful PTA in the proximal vessel segments. On the lower leg, the anterior, posterior, and fibular tibial arteries are occluded. The posterior tibial artery fills via collaterals in the proximal third of the lower leg and is the only continuous artery in the lower leg that is severely sclerotized and moderately stenosed distal to the ankle. After numerous attempts with various CTO wires and a long sheath, it is not possible to recanalize the posterior tibial artery through an antegrade approach via the common femoral artery (Fig. 2a).
- This is followed the next day by ultrasound-targeted puncture of the posterior tibial artery and insertion of a 4F sheath. Retrograde effortlessly passes the closure of the proximal posterior tibial artery with a CTO wire. Pre-dilation with a 1.5/40 mm balloon is followed by implantation of a XIENCE 3.5/38 mm “drug eluting” stent (Fig. 2b).
- The final angiography shows a very good result (Fig. 2c).
- The patient is symptom-free immediately after the procedure and can be discharged home the following day (Fig. 2d).
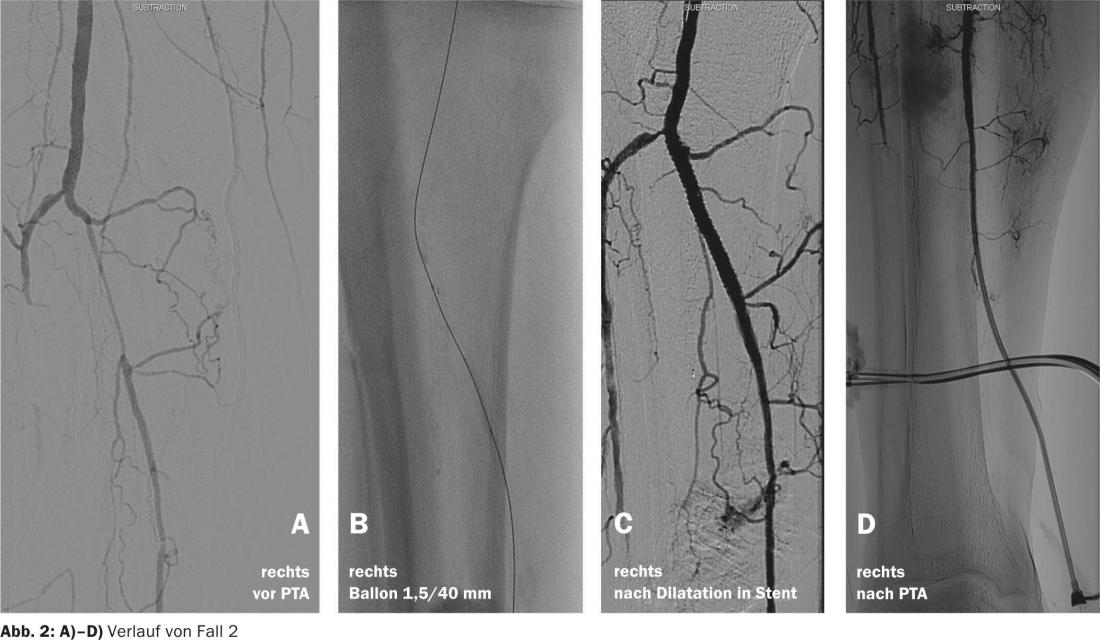
Case 3
As a third case, we would like to present a 53-year-old patient with multiple PTAs and stenting of a long-stretch occlusion of the left superficial femoral artery. Acute stent occlusion with critical ischemia, rest pain, and an ABI li=0.46 are present.
- Baseline angiography demonstrates long-stretch instent occlusion of the left superficial femoral artery. To avoid embolization, rheolytic thrombectomy with an angiojet catheter, thrombolysis with rtPA, balloon dilatation, and stenting are performed (Fig. 3a).
- Abundant thrombotic material can be removed with the angiojet (Fig. 3b).
- Residual thrombi are penetrated into the wall with 5 mg Actilyse via the angiojet catheter and lysed (Fig. 3c).
- A second pass with the angiojet further improves the angiographic result (Fig. 3d).
- A stenosis at the proximal end of the stent is dilated several times and finally stented, as shown in Figure 3e .
- The final angiography shows a very good result (Fig. 3f).
- On the lower leg, there is free contrast drainage with no evidence of embolization. The risk of distal athero-thrombotic microembolization during endovascular procedures has been reported to be as high as 98%, although only 1.6-3% are clinically relevant. The Angiojet is a hydrodynamic system for comminution and removal of thrombotic material based on Bernoulli’s principle and the Venturi effect (see section on Angiojet on gefaessmedizin.ch). Saline is injected at high speed, creating a vacuum that flushes the fragmented thrombus into the catheter’s side holes. These catheters are available with diameters ranging from 2.0-20.0 mm and in lengths up to 140 cm, giving a wide potential field of application from small transtibial arteries to larger lumen veins (Fig. 3g).
Case 4
This is an 80-year-old patient with claucicatio intermittens after 100 m of pain-free walking in the left leg. He has a classic risk profile (metabolic syndrome and 50 py cigarette smoking) and a left ABI 0.53. Duplex ultrasonography reveals a high-grade stenosis of the left popliteal artery due to an eccentric sclerotic plaque.
- Intra-arterial angiography confirms the duplex findings (Fig. 4a).
- Due to the eccentric sclerotic plaque, we decide to atherectomy with a TurboHawk with the primary goal of reducing plaque burden (Fig. 4b).
- A guidewire is used to pass through the stenosis, an embolic protection filter is placed distally, and the plaque is removed in multiple passes with the TurboHawk (Fig. 4c).
- The postinterventional result is so satisfactory that PTA can be omitted (Fig. 4d).
- Distal outflow is unchanged with no evidence of embolism. The aim of atherectomy is to reduce the plaque burden and thus increase the intraluminal diameter. One expects, lower reintervention rates and fewer “bail-out” stentings. On gefaessmedizin.ch under the Turbohawk section we show you the procedure of an atherectomy with the TurboHawk (Fig. 4e).

Case 5
A 70-year-old patient presents with massive swelling of the right upper and lower leg. He reports that he has had repeated venous thromboses, which were treated by the family doctor in each case with short-term heparin administration. After swelling of the leg had subsided after a few days, heparin administration had been stopped in each case. In addition to leg swelling, marked hemosiderin deposits on the inner ankle of the affected leg are noticeable. Duplex sonography reveals right iliac vein thrombosis with complete obstruction of the right external iliac vein , probable older thrombosis of the right common femoral vein, and partial thrombosis of the superficial femoral vein.
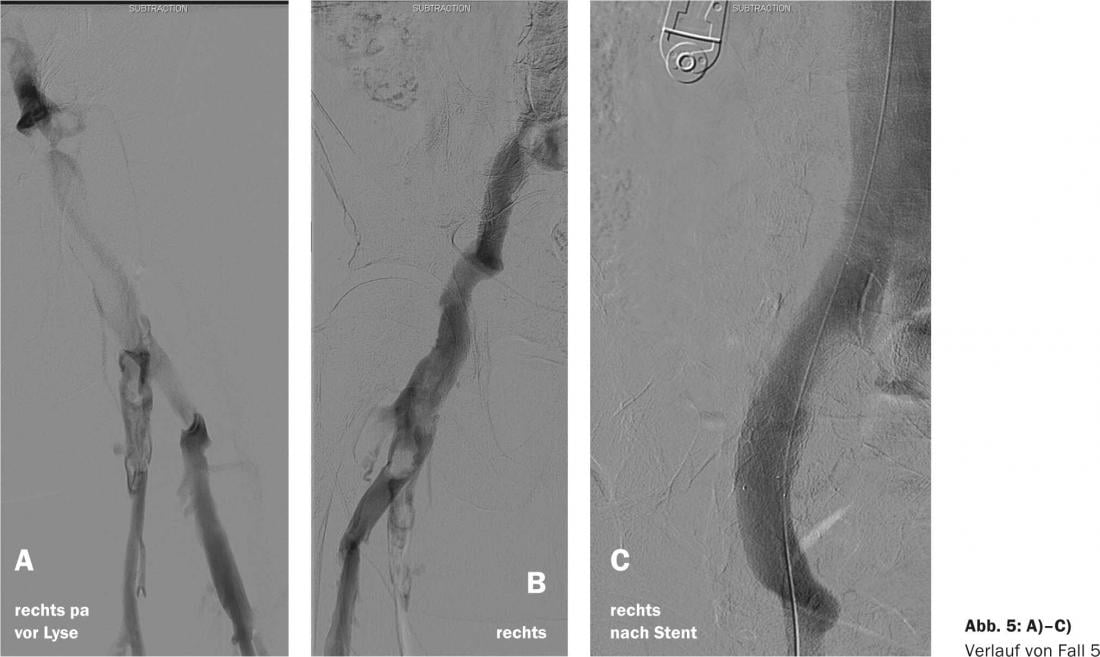
- Phlebography obtained in the prone position after ultrasound-guided puncture of the right popliteal vein confirmed these findings. We assume that the thromboses in the V. iliaca externa and the V. femoralis communis are older and show fresh thrombosis. Due to the pronounced leg swelling and trophic skin changes, the indication for catheter lysis is given. For this purpose, a lysis catheter is placed in the occlusion of the V. femoralis communis and lysed with a total of 20 mg rt-PA (Actilyse) for 15 hours. Just four hours after the start of lysis, the right leg again has the same diameters as the left (Fig. 5a).
- After completion of lysis, course phlebography shows a reduction in thrombus burden in the area of the common femoral vein. Chronic thrombosis in the pelvic axis region is unchanged (Fig. 5b).
- The iliac vein lesion is covered with a 16/60 Zilver Vena Stent to improve venous outflow. The catheter material is then removed and a pressure dressing is applied for three hours. The patient leaves the hospital the same evening without any complaints. Continuous anticoagulation with rivaroxaban is prescribed. Patients with ilio-femoral deep vein thrombosis are at high risk of developing postthrombotic syndrome. Direct catheter lysis and stenting of venous stenoses can successfully prevent this (Fig. 5c) [4].
Literature:
- Langhoff H, et al: J Cardiovasc Surg (Torino) 2013 Oct; 54(5): 553-559.
- Jäger KA, et al: Switzerland Med Forum 2009; 9(39): 690-693.
- Morrow DA, et al: N Engl J Med 2012; 366: 1404-1413.
- Karnabatidis D, et al: J Endovasc Ther 2006; 13: 269-280.
- Lin PH, et al: J Surg Res 2002; 103: 153-159.
- Karnabatidis D, et al: Cardiovasc Interv Radiol 2011; 34: 1123-1136.
- Zeller T, et al: J Am Coll Cardiol 2006; 48: 1573-1578.
- Shammas NW, et al: J Vasc Interv Radiol 2011; 22: 1223-1228.
- Engelberger RP, et al: Thromb Haemost 2014; 111: 1153-1160.
CARDIOVASC 2014; 13(5): 8-14