The high prevalence makes acne a popular topic at dermatology congresses – including this year’s EADV conference in Amsterdam. Several small studies were devoted to epidemiology, discussed modifications in therapy, and dealt with the unpleasant long-term consequences of acne, scars.
(ag) Current prevalence data were provided by Prof. Pierre Wolkenstein, MD, Créteil. In a representative sample consisting of 8000 teenagers and young adults (15 to 24 years) from Spain, Italy, Poland and France, the researchers assessed the frequency and severity of acne by means of questionnaires completed by the subjects.
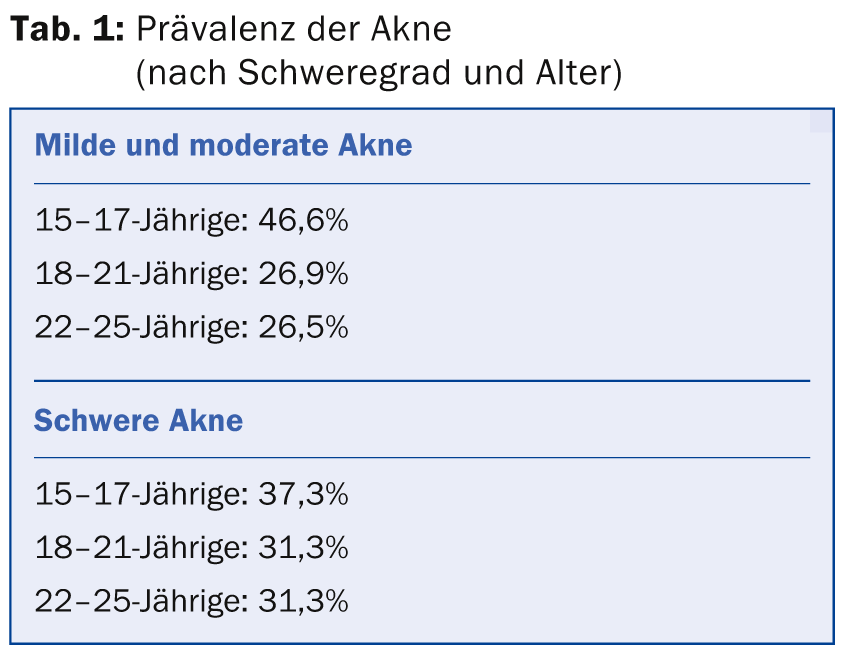
The lifetime prevalence was 65.5%. The point prevalence at the time of the survey was 31.06%, and of these patients, approximately one-third had severe forms of acne. The frequency, broken down by age and severity, is shown in detail in Table 1 .
What was the medical procedure? 38.7% with mild to moderate acne and 43.4% with severe forms were treated primarily by dermatologists. Only 13.4% of the first group stayed with their primary care physician, while 19.2% did so in the second group.
“All these prevalence data largely correspond to what we already know from the literature. With a multivariate analysis, we therefore wanted to find out more precisely which factors show a correlation,” says Prof. Wolkenstein. Here, it was shown that age and family history were particularly decisive: The younger the person examined, the greater the probability of acne. Compared to the comparison group without affected parents, the risk also increased by a factor of 7.87 if the mother already had or still has acne, and by 6.41 if this applied to the father. If both parents suffered from acne, the risk was 31.08 times higher than in the comparison group. As in other studies based on self-reporting, an inverse relationship was shown for the smoking factor: Nicotine consumption reduced the probability of acne by 33%.
Very low-dose isotretinoin effective in the long term?
At the 2012 EADV Congress, Prof. Marius Rademaker, MD, Hamilton, had already presented surprising results of a study demonstrating good efficacy of very low-dose isotretinoin (5 mg/day) in 60 adults with persistent minor acne. The treatment reduced the number of lesions, improved quality of life, and showed minimal side effects. “However, we were concerned that patients might relapse quickly, so we observed them in a follow-up for another 30 to 36 months,” Prof. Rademaker said. The results of the follow-up were now presented at the EADV Congress 2014 – again with promising implications. Three quarters of patients could be evaluated for follow-up. They were demographically similar to the baseline population: 38 years old on average and predominantly women. All had received 5 mg/d isotretinoin for either 16 or 32 weeks in the original study protocol and then stopped.
40% of patients remained free of acne during follow-up. The remainder showed mild recurrence at an average of 6.6 months after the end of therapy. Almost half of those affected by the relapse, although minimal acne, started treatment again with the same dose. On average, this follow-up lasted 12.4 months, and in many cases it took place with interruptions. Neither age nor initial duration of therapy (16 vs. 32 weeks) nor acne severity (at baseline or end of study) significantly influenced the likelihood of recurrence. The cumulative dose also did not play a role in this regard. “In our study, acne could thus be controlled quickly, effectively, and with few side effects using very low-dose isotretinoin,” the speaker said. “40% of patients are thus in long-term remission, and the remaining 60% have also been able to achieve good control again with renewed periodic initiation of treatment.”
Acne scars – what to do?
Philippe Martel, MD, Sophia Antipolis, presented the results of a study evaluating an antibiotic-free fixed combination of adapalene and benzoyl peroxide (BPO) for the treatment of atrophic acne scars. Specifically, they compared the gel to vehicle (each applied to one side of the face) in a randomized, blinded fashion over 24 weeks. The basic assumption of the study was that topical retinoids stimulate dermal fibroblasts to produce more procollagen. This finding comes from the field of light-aged skin. Since acne scars are also associated with a loss of dermal matrix, we wanted to test the extent to which adapalene-BPO could prevent atrophic scars or improve pre-existing forms. Thirty-eight adults (18- to 35-years-old) participated in the study, 31 of whom completed it. On average, those affected were 23.4 years old and each had 22.7 inflammatory and 21.2 noninflammatory lesions. In the Scar Global Assessment (SGA, between 0 and 4), they scored 2.1 on both halves of the face at baseline. There was a mean of 10.8 scars on the vehicle side and 11.1 on the verum side. Only scars larger than 2 mm were counted.
At week 24, on the one hand, the rate of inflammatory lesions on the adapalene BPO half had decreased highly significantly (p<0.001). The SGA score was significantly lower than with vehicle (1.71 vs. 2.1, p=0.003). The number of scars also remained stable under the verum, while it increased on the vehicle side (mean 11.6 vs. 13.6, p=0.04). The scar volume did not change as a result of the treatment. “Our exploratory study thus showed stabilization of scar development under the fixed combination adapalene-BPO,” the speaker concluded.
Acne scars can also be addressed with chemical peels. George Kontochristopoulos, MD, Athens, spoke about the use of these procedures for different types of acne. Superficial as well as medium and deep chemical peels can be used for acne treatment, either alone or in addition to classical therapy. The principle is always based on a chemical-induced skin injury, which results in tissue regeneration and remodeling. The most commonly used substances include glycolic acid, mandelic acid, pyruvic acid, salicylic acid, trichloroacetic acid, Jessner’s solution and phenol. These agents have sebostatic, keratolytic, antibacterial and anti-inflammatory properties, besides they can induce neocollagenesis. According to the speaker, superficial peels are particularly suitable for acne with comedones, papules and pustules. For acne scars, in addition to superficial peels, deeper peels are also used.
Source: EADV Congress, October 8-12, 2014, Amsterdam
DERMATOLOGIE PRAXIS 2014; 24(6): 42-43











