An effective method that can reliably and quickly relieve back pain is infiltration. Without surgical intervention, the patient’s mobility and freedom from pain can thus be restored, and further multimodal therapy measures can be applied. If the pain is very severe or has lasted for a long time, infiltration therapy is a way of transporting the painkiller directly to where its cause is located.
Back pain is often nociceptive pain triggered by degenerative changes or wear and tear in the facet joints. This pain is usually sharp or throbbing, but can also be dull and occurs in the lumbar spine. Alternatively, the pain may be caused by tension in the muscles. If, on the other hand, the pain arises from compression of the nerve, it is neuropathic pain localized in the dermatome, explained Dr. Julia Wölfle-Roos, Department of Orthopedics/Pain Therapy, Fachklinik Ichenhausen (D) [1]. Neuropathic pain may be perceived as burning or tingling sensations or as hypersensitivity to touch or cold. As a result, there may be an amplification of pain stimuli associated with increased pain sensitivity, which can easily develop into chronic pain.
Physiological reaction of the body
If a pain impulse is transmitted along the ascending pain pathways, the reaction is not only the sensation of pain, but an inhibitory process is also triggered at the same time. The body’s normal response is to suppress the pain. The transmission of nociceptive signals by the projection neuron is prevented by the activity of an inhibitory interneuron, namely by the information arriving through the affected dermatome. Touch sensitivity is transmitted via Aβ-fibers and these inhibit pain intensity via interneurons (segmental inhibition). There are also corresponding functions in the brainstem that reduce the intensity of the transmitted pain via serotonin, norepinephrine and interneurons (descending inhibition).
Pathophysiology of chronic pain
Chronic pain, on the other hand, has become disconnected from acute nociceptive processes and has become a pathological entity in its own right. For example increased activity takes place in the nociceptor. Increased excitability of the nerve follows. Sodium channels are highly regulated and, accordingly, neuropathic signals are transmitted much more strongly. More transmitters than usual are released in the posterior horn neuron, resulting in hyperalgesia. If, in addition, the synapses of the neighboring pain fibers and the Aβ-fibers interconnect on the posterior horn neuron, an enlargement of the receptive field occurs and pain is felt just by touching the skin area, resulting in so-called allodynia. The thalamus is activated for a long time and the descending pain inhibition does not work anymore, serotonin and noradrenalin are in short supply.
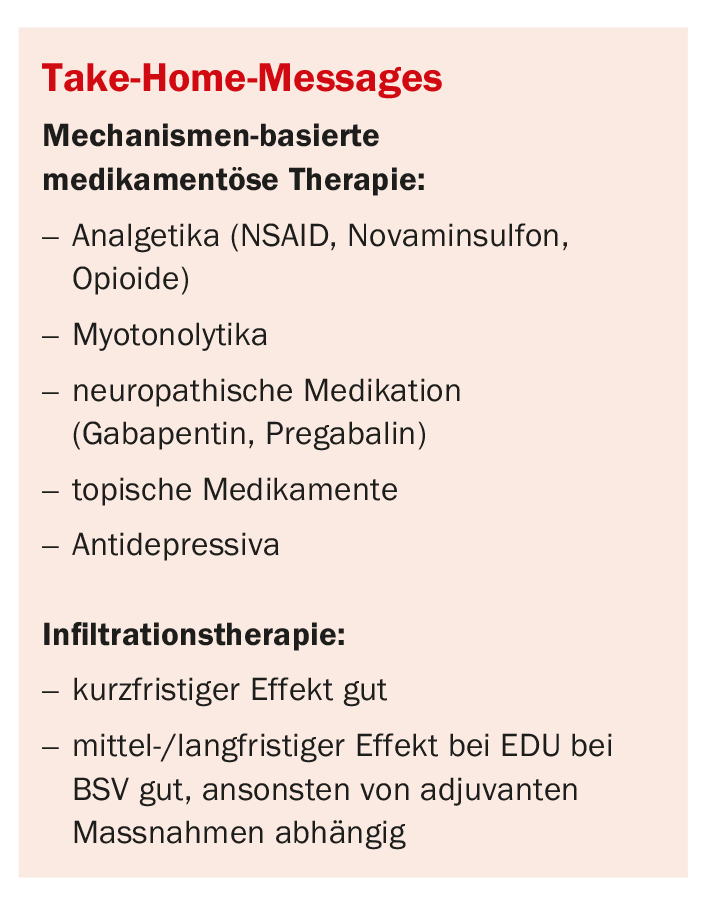
Intervention options – analgesics and coanalgesics.
When non-steroidal anti-inflammatory drugs (NSAIDs) are taken, there is interference with the inflammatory mediator balance via selective or non-selective COX-2 inhibition, which directly affects nociception. The use of paracetamol and novamine sulfone shows a more peripheral effect but spinal and supraspinal effects have also been noted. In the case of muscle tension, it is also possible to intervene causally by reducing the tension with appropriate medication. Classically, methocarbamol, for example, is used, which directly reduces muscle tension, but long-term experience is still lacking for pridinol. Tizanidine should be used with caution for back pain, as the drug is usually used in spasticity patients in cases of paraplegia or stroke.
In the case of neuropathic pain, there is also the possibility of attacking the periphery. If there is a specific area, for example, on the arm or leg, where allodynia or hyperalgesia occurs, this area can be treated with local anesthetics. Lidocaine gel/patches or capsaicin patches, which contain the active ingredient of the chili, are used in this case. The resulting burning sensation relaxes the neuron and releases the transmitters, leaving the pain patient pain-free for eight to twelve weeks. At the posterior horn neuron, gabapentinoids can still be used to intervene in neuropathic pain. These act specifically at the NMDA receptor, i.e., at excitatory transmission. In addition, there is the option of transcutaneous electrical nerve stimulation (TENS), in which the Aβ-fibers are stimulated with electricity so that a tingling sensation is produced. Tingling reduces the transmission of pain via interneurons. In this case, we also speak of the so-called gate control mechanism.
Specific antidepressants can also be used to specifically address descending pain inhibition. These drugs are used because a specific mechanism descending, via serotonin and especially norepinephrine, inhibits the transmission of pain intensity at the posterior horn. Classic active ingredients here are amitriptyline from the tricyclic series and duloxetine from the SNRIs. Opioids act, spinal and supraspinal as well as peripheral, especially in inflammatory situations. They are divided into low-potent (e.g., tilidine or tramadol) and high-potent such as buprenorphine or tapentadol. Tramadol and tapentadol have an additional mechanism of action as norepinephrine reuptake inhibitors and also act on descending pain inhibition.
Meaning subjective pain perception
Evidence from behavioral reports suggests that patients’ beliefs and expectations may influence both the therapeutic and adverse effects of a given drug and that regulatory brain mechanisms differ as a function of expectation [2]. It is therefore necessary to integrate patients’ beliefs and expectations into the drug treatment regimen, in addition to traditional considerations, to optimize treatment outcomes, she said.
Intervention options – infiltrations
Diagnostic infiltrations are usually done with local anesthetic and only to specific sites of pain to find out where the pain is coming from. Therapeutic infiltrations, on the other hand, are a way to create low-pain intervals during which other therapeutic measures can take effect. “However, in order not to create excessive expectations in the patient, one should always point out that an injection alone is usually not enough,” the expert warned. A classic infiltration is facet joint infiltration, an intra- or extra-articular injection under BV (ramus posterior/dorsalis). However, it is also possible to address not the joint per se, but the ramus medialis, which arises from the ramus dorsalis and supplies the facet joint nociceptively, as opposed to the ramus lateraris. The ramus medialis is also infiltrated under BV, using an oblique projection (20 degrees) considering the landmarks: proc. art. superior, Proc. transversus and the pedicle eye. Facet joint infiltration can also be performed on the cervical spine, but in this case it is performed intraarticularly in the lateral radiographic pathway while the patient is lying down or sitting. In epidural flooding, the target is the epidural space. On the one hand, pain in the ramus anterior/ventralis can be addressed bilaterally; on the other hand, the ramus meningeus can be addressed and thus also structures in the posterior longitudinal ligament, dorsal annulus, and to some extent the facet joints. Epidural reflux can be performed interlaminar, transforaminal, or via the sacral hiatus, BV- or CT-guided. The indication for a herniated disc shows good results even after a long period of time. If infiltration is performed only for back pain without nerve compression or, for example. in failed-back surgery syndrome, the result is satisfactory to poor. In nerve root infiltration (PRT), the nerve is flooded in the area of the neuroforamen, which shows a unilateral effect on the specific dermatome. This infiltration is also BV- or CT-guided and can be performed in the lumbar or cervical spine. The results are similar to those of epidural flooding. Intraarticular ISG infiltration shows a similar picture as facet joint infiltration: diagnostically good, with short-term effect, therapeutically poor.
Study results
The efficacy of infiltrations was reviewed in a study that evaluated the quality and clinical relevance from a total of 2400 studies [3]. For each infiltration, it was individually classified whether a positive result was obtained. For randomized controlled trials, the outcome had to be clinically relevant and significant; for observational studies, there had to be at least a therapeutic improvement in pain at >40%; at one, three, six, or 12 months; and for diagnostic infiltrations, pain had to be relieved by at least >75%. Evidence was categorized as good (at least two controlled-randomized trials that demonstrated a positive effect), satisfactory (at least one controlled-randomized trial or multiple observational studies that demonstrated a positive effect), or poor (either no evidence or the evidence showed no difference from the control group). Diagnostic facet joint infiltration has resulted in short-term relief of symptoms in both the lumbar spine, cervical spine, and thoracic spine. Intraarticular outcomes were poor for therapeutic facet joint infiltrations. Only the medialis block achieved a satisfactory to good result. Conclusion: short-term effect to be expected, not suitable as the only measure in the long term, according to Dr. Wölfle-Roos.
Furthermore, multimodal therapy measures can be used to strengthen self-efficacy through active therapy, such as physiotherapy, manual medicine, exercise therapy, relaxation, acupuncture, behavioral therapy.
Pain has many factors!
Hospital records of patients recovering from cholecystectomy have shown that assigning a room with a window view of a natural environment can have a restorative effect. Patients housed in rooms with a window view of a natural environment had a shorter postoperative hospital stay, received fewer negative comments in nurses’ notes, and took fewer strong pain medications than similar patients in similar rooms with windows facing a brick wall [4].
The aim of another study was to determine the relationship between marital interaction and spouse caring to the perception of acute pain stimuli and psychophysiological reactivity. Patients with chronic low back pain and control subjects participated with their cohabitants in two cold pressor tests (one in the presence, one in the absence of the spouse) and one neutral as well as one conflict verbal interaction. The results suggest that spouse caring is associated with increased pain perception in chronic pain patients, but muscular reactivity seems to be related only to patient status [5]. “You can thus see: Drug treatment is always only one part of the therapy; in addition, there are a large number of factors to consider,” was the speaker’s conclusion.
Congress: German Rheumatology Congress 2021
Literature:
- PD Dr. med. Julia Wölfle-Roos, Update Schmerztherapie bei Rückenschmerzen, Lecture German Rheumatology Congress 2021, 17.09.2021.
- Bingel, et al: The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci Transl Med 2011, doi: 10.1126/scitranslmed.3001244.
- Manchikanti, et al: An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician 2013, doi: 10.36076/ppj.2009/12/699.
- Ulrich: View through a window may influence recovery from surgery. Science 1984, doi: 10.1126/science.6143402.
- Flor, et al: A psychophysiological analysis of spouse solicitousness toward pain behaviors, spouse interaction, and pain perception. Behavior Therapy 1995, doi: 10.1016/S0005-7894(05)80105-4.
InFo PAIN & GERIATry 2021; 3(2): 24-25.