Cardiac imaging has contributed substantially to the understanding of CHD. It has become a cornerstone of diagnostics and management. However, the benefits of imaging must always be weighed against the costs and any risks. Essential here is the right modality for the corresponding question.
The differential diagnosis in patients with thoracic complaints is extensive, ranging from benign entities to potentially life-threatening conditions. In Switzerland, a good 3% of visits to the general practitioner are due to thoracic complaints, and one in five patients with such complaints is referred to a specialist before a diagnosis is made [1]. Since coronary artery disease (CAD), in particular, is a potentially threatening cause with corresponding morbidity and mortality, there is a great demand for efficient and non-invasive diagnostic modalities to exclude or treat it. Evidence of such. In this environment, imaging modalities in particular have developed rapidly in recent years, driven by substantial technological evolutions. However, precisely because of the increasingly frequent use of these modalities, questions also arise regarding the associated costs, the potential risks for patients, and, last but not least, the appropriate application in everyday clinical practice [2].
Imaging modalities
Stress echocardiography: stress echocardiography is based on the detection of ischemia-induced wall motion abnormalities that can be provoked with physical or pharmacological stress. With the use of dobutamine, stress echocardiography can be further used to provide an indication of myocardial viability [3]. Recent developments such as “strain imaging” and 3D echocardiography have the potential to further improve the diagnostic accuracy of stress echocardiography. The main limitation of the method is especially the dependence on the examiner and sound quality (e.g. in obesity, emphysema, funnel chest, etc.).
Cardiac CT: Cardiac CT allows an anatomic/morphologic assessment of the heart and in particular also of the coronaries, comparable to the information that invasive coronary angiography can provide. In the context of CHD, the strength of the method lies particularly in its ability to exclude CHD due to its excellent sensitivity and near-perfect negative predictive value in patients with low pretest probability. [4,5] (Fig. 1 and tab. 1). The specificity, on the other hand, is rather moderate, since CT leads to an overestimation of the degree of stenosis. The prognostic value of cardiac CT has been demonstrated in several trials and large multinational registries [6].


It is worth mentioning that the technology has made immense technological progress in recent years, which in the meantime allows acquiring high-resolution images with very low radiation exposure. The average radiation exposure is in the range of 2-5 millisieverts (mSv) [7]; in specialized centers, average values of well below 1 mSv are now routine [8]. The limitation of the method is especially the necessary patient selection. Thus, in patients with marked or absolute arrhythmias, the coronaries can be examined only to a limited extent, depending on the type of scanner. Furthermore, the usual contraindications for contrast-enhanced CT examinations apply, namely iodine allergy and severe renal insufficiency.
Single Photon Emission Computed Tomography (SPECT): Myocardial perfusion SPECT is based on the principle of perfusion-dependent tracer uptake into viable myocytes and detection of γ-radiation ultimately emitted during radionuclide decay. Today, mainly 99m-technetium-based tracers are used, such as sestamibi or tetrofosmin, as they allow better image quality at lower radiation exposure in contrast to 201-thallium (Fig. 2). The latter could be significantly reduced, especially with the introduction of modern detectors, and is in the range of 2-5 mSv [9].

Loading can be done physically or by intravenous administration of dobutamine or adenosine. Finally, perfusion deficits induced by exercise or already existing at rest allow the detection of ischemia or ischaemia. Myocardial scars and thus the detection of CHD with high diagnostic accuracy [10]. Simultaneous ECG triggering also allows for left ventricular volumes and contractility to be assessed. In contrast to other modalities, SPECT has data on its prognostic value for many tens of thousands of patients, underscoring the role of this method also for risk stratification of patients with CHD [11,12].
Positron emission tomography (PET): Like SPECT, PET examination is also based on the detection of radioactive decay. However, the methods differ fundamentally with respect to the type of radionuclides used: While radionuclides with γ-decay and relatively long half-lives (e.g., 6 h for 99m-technetium) are used, those used in myocardial perfusion PET are those with β+-decay and comparatively short half-life (e.g., 10 min for 13N-ammonia), which implies the availability of a cyclotron for their immediate on-site production; an exception is 82-rubidium, which can be produced with a generator. The resolution of PET is significantly better than that of SPECT and the attenuation correction is more robust, resulting in PET offering some of the highest diagnostic value of all imaging methods (Table 1) [13]. In addition, PET allows absolute quantification of myocardial blood flow in ml/min/g (Fig. 3), which improves detection of any balanced coronary three-vessel disease or microcirculatory dysfunction [14]. The prognostic value of myocardial perfusion imaging with PET has been demonstrated in several large studies [15–17]. The radiation exposure of a 13N-ammonia myocardial perfusion study is 1-3 mSv.

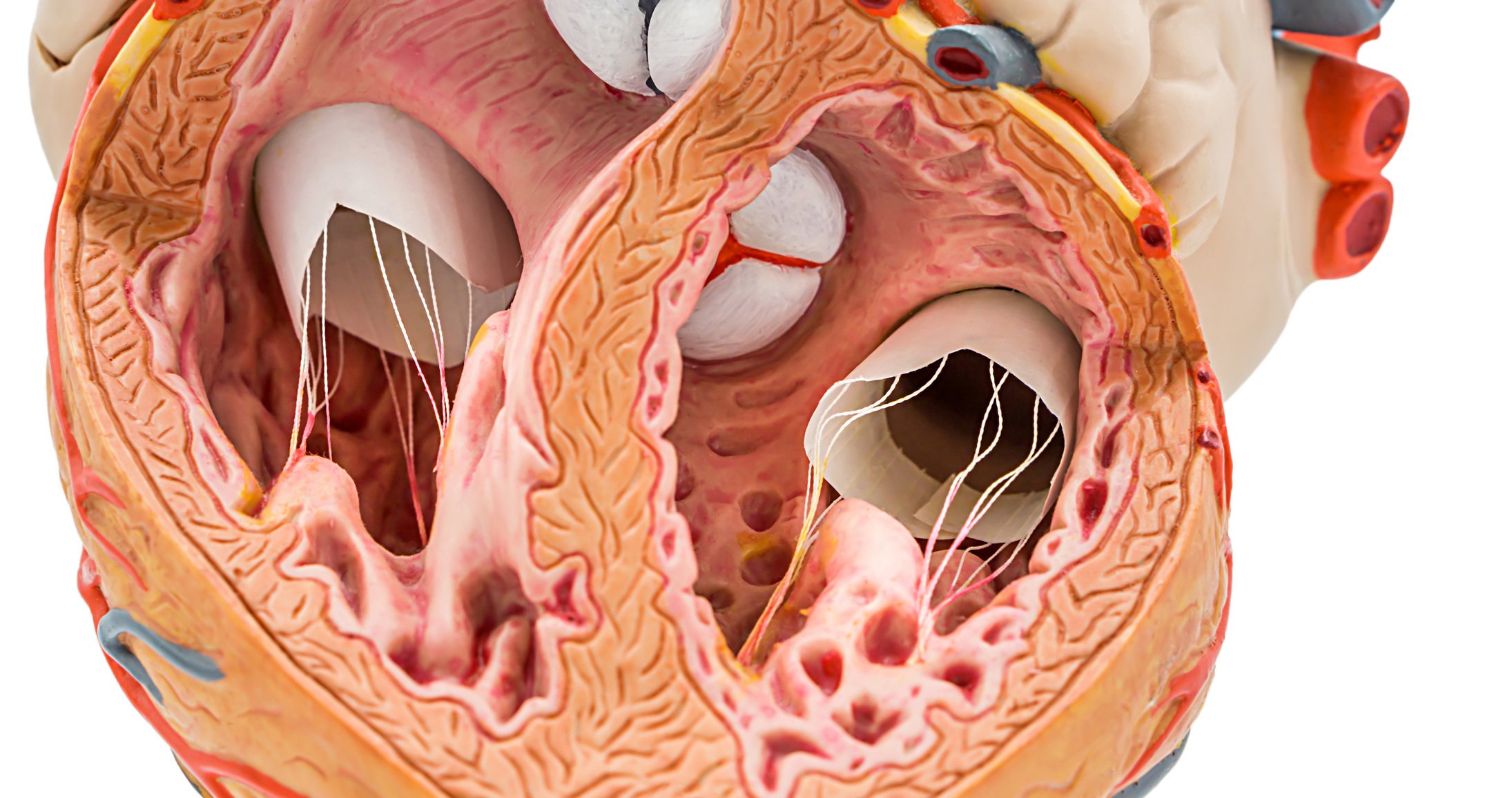
Magnetic resonance imaging (MRI): Cardiac MRI not only provides excellent information on cardiac function and morphology, but also allows qualitative information on myocardial perfusion with good diagnostic accuracy by image acquisition during application of gadolinium-containing contrast medium at rest and under pharmacological stimulation with adenosine (Fig. 4 and Table 1) [13,18]. When dobutamine is used as a stressor, additional ischemia-induced wall motion abnormalities can be detected. Finally, tissue characterization can be performed using late-gadolinium enhancement (LGE) imaging. In the context of CHD, this is particularly true for the detection of infarct scars and, conversely, for the detection of viable myocardium. Contraindications for cardiac MRI are mainly metal implants (including most of the implanted pacemakers or CRT and ICD devices), severe renal insufficiency and claustrophobia. Arrhythmias and limited cooperation in breath holding also affect image quality.

Hybrid Imaging: Hybrid imaging describes the integration and fusion of multimodal imaging with co-registration. Currently, the greatest clinical benefit is obtained by combining anatomic/morphologic and functional information, e.g., combining cardiac CT with myocardial perfusion SPECT or PET. This allows simultaneous assessment of the severity of stenoses and their hemodynamic relevance as well as visualization of the affected supply area (Fig. 5). A number of smaller studies have demonstrated the diagnostic superiority of hybrid imaging using SPECT and PET/CT over the individual modalities alone [19] as well as their prognostic value [20,21].

Differential use of methods for the diagnosis of CHD
Pretest probability and Bayes’ theorem: Sensitivity and specificity are the terms usually used to determine diagnostic accuracy. However, both are per se inadequate to describe how the accuracy of the method fares in a real clinical setting. In abstract form, Bayes’ theorem formulates in this situation how the pretest probability for a disease is related to the sensitivity resp. Specificity of a given examination method interacts. Thus, pathologic examinations are often false positive in patients with very low pretest probability, whereas normal workups are often false negative in patients with high pretest probability. In terms of imaging modalities for the evaluation of CHD, this means that their diagnostic value is highest with a moderate pretest probability of 15-85%. Among symptomatic patients, these are those with atypical angina and middle-aged female patients with typical angina (Table 13 in reference [13]). These patients should primarily undergo noninvasive imaging [13].
Comparison of modalities and recommendations: Attempts to compare the diagnostic accuracy of the different methods are limited in many cases by the different surrogate markers for ischemia of the different modalities (eg, anatomic/morphologic assessment by CT, wall motion abnormalities by stress echocardiography, and perfusion imaging by PET, SPECT, or MRI) and by the different local expertise for one modality. It is therefore not surprising that the reported values for sensitivity and specificity show a wide spread and overlap considerably in some cases (Tab. 1) . While there are individual studies that suggest a superiority of individual modalities [22,23]published, partly pooled data rather lead to the assumption that the real differences are probably smaller than assumed. [24,25]. However, there is consensus on the recommendation of the current ESC guidelines that the diagnostic accuracy of imaging is superior to that of the stress electrocardiogram and should therefore be preferred to the latter whenever available [13]. Figure 6 provides an overview of the imaging strategy recommended by the ESC for suspected CHD. It should be noted that differential imaging plays a particularly important role in this context: Table 2 is intended to provide a concluding guide here.


Take-Home Messages
- Cardiac imaging has contributed substantially to our understanding of CHD and has become a cornerstone of diagnostic and
- Management of CHD developed.
- Current guidelines recommend noninvasive imaging in stable patients whenever local expertise is available.
- At the same time, it is always important to carefully assess the benefits of imaging versus the associated costs and any risks. It is essential to choose the right modality for the appropriate problem in the right patient depending on the patient’s clinical characteristics and comorbidities as well as local expertise.
Literature:
- Verdon F, et al: Chest pain in daily practice: occurrence, causes and management. Swiss Med Wkly 2008; 138: 340-347.
- Fazel R, et al: Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361: 849-857.
- Sicari R, et al: Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 2008; 9: 415-437.
- Meijboom WB, et al: Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 2008; 52: 2135-2144.
- Budoff MJ, et al: Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008; 52: 1724-1732.
- Min JK, et al: Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011; 58: 849-860.
- Buechel RR, et al: Low-dose computed tomography coronary angiography with prospective electrocardiogram triggering: feasibility in a large population. J Am Coll Cardiol 2011; 57: 332-336.
- Benz DC, et al: Minimized Radiation and Contrast Agent Exposure for Coronary Computed Tomography Angiography: First Clinical Experience on a Latest Generation 256-slice Scanner. Acad Radiol 2016; 23: 1008-1014.
- Acampa W, Buechel RR, Gimelli A: Low dose in nuclear cardiology: state of the art in the era of new cadmium-zinc-telluride cameras. Eur Heart J Cardiovasc Imaging 2016; 17(6): 591-595.
- Verberne HJ, et al: EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging 2015; 42: 1929-1940.
- Shaw LJ, Iskandrian AE: Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004; 11: 171-185.
- Hachamovitch R, et al: Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J 2011; 32: 1012-1024.
- Montalescot G, et al: 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34: 2949-3003.
- Fiechter M, et al: Diagnostic value of 13N-ammonia myocardial perfusion PET: added value of myocardial flow reserve. J Nucl Med 2012; 53: 1230-1234.
- Murthy VL, et al: Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation 2011; 124: 2215-2224.
- Dorbala S, et al: Prognostic value of stress myocardial perfusion positron emission tomography: results from a multicenter observational registry. J Am Coll Cardiol 2013; 61: 176-184.
- Taqueti VR, et al: Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015; 131: 19-27.
- Schwitter J, et al: MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur Heart J 2008; 29: 480-489.
- Gaemperli O, Bengel FM, Kaufmann PA: Cardiac hybrid imaging. Eur Heart J 2011; 32: 2100-2108.
- van Werkhoven JM, et al: Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol 2009; 53: 623-632.
- Pazhenkottil AP, et al: Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J 2011; 32: 1465-1471.
- Schwitter J, et al: MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 2013; 34: 775-781.
- Greenwood JP, et al: Comparison of cardiovascular magnetic resonance and single-photon emission computed tomography in women with suspected coronary artery disease from the Clinical Evaluation of Magnetic Resonance Imaging in Coronary Heart Disease (CE-MARC) Trial. Circulation 2014; 129: 1129-1138.
- Jaarsma C, et al: Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: a meta-analysis. J Am Coll Cardiol 2012; 59: 1719-1728.
- Greenwood JP, et al: Effect of Care Guided by Cardiovascular Magnetic Resonance, Myocardial Perfusion Scintigraphy, or NICE Guidelines on Subsequent Unnecessary Angiography Rates: The CE-MARC 2 Randomized Clinical Trial. JAMA 2016; 316: 1051-1060.
CARDIOVASC 2017; 16(2): 23-30