In addition to certain risk and trigger factors, psoriasis is associated with various comorbidities, such as metabolic syndrome, cardiovascular disease, and depression. This is particularly true for patients with moderate and severe psoriasis. Loss of quality of life and reduced life expectancy are possible consequences. Therefore, these factors should be included in disease management.
The term psoriasis is derived from the Greek word “psora”, which means itch or scabies [1]. For a long time, no distinction was made between psoriasis and scabies caused by mites. Confusion with leprosy was also said to be common. Ferdinand von Hebra (1816-1880) was one of the first to distinguish psoriasis vulgaris from leprosy. Until the middle of the 20th century, the etiology and pathogenesis of psoriasis were unknown, so that no targeted therapeutic approaches were developed for a long time. Thus, until modern times, the treatment of psoriasis consisted mainly of topical treatments, such as tar or arsenic. It was not until the 20th century that evidence-based therapies such as phototherapy, oral antipsoriatic drugs, and specific cortisone ointments were used. However, the real breakthrough did not occur until the end of the 20th century with the introduction of biologics [2].
Groundbreaking advances in psoriasis research
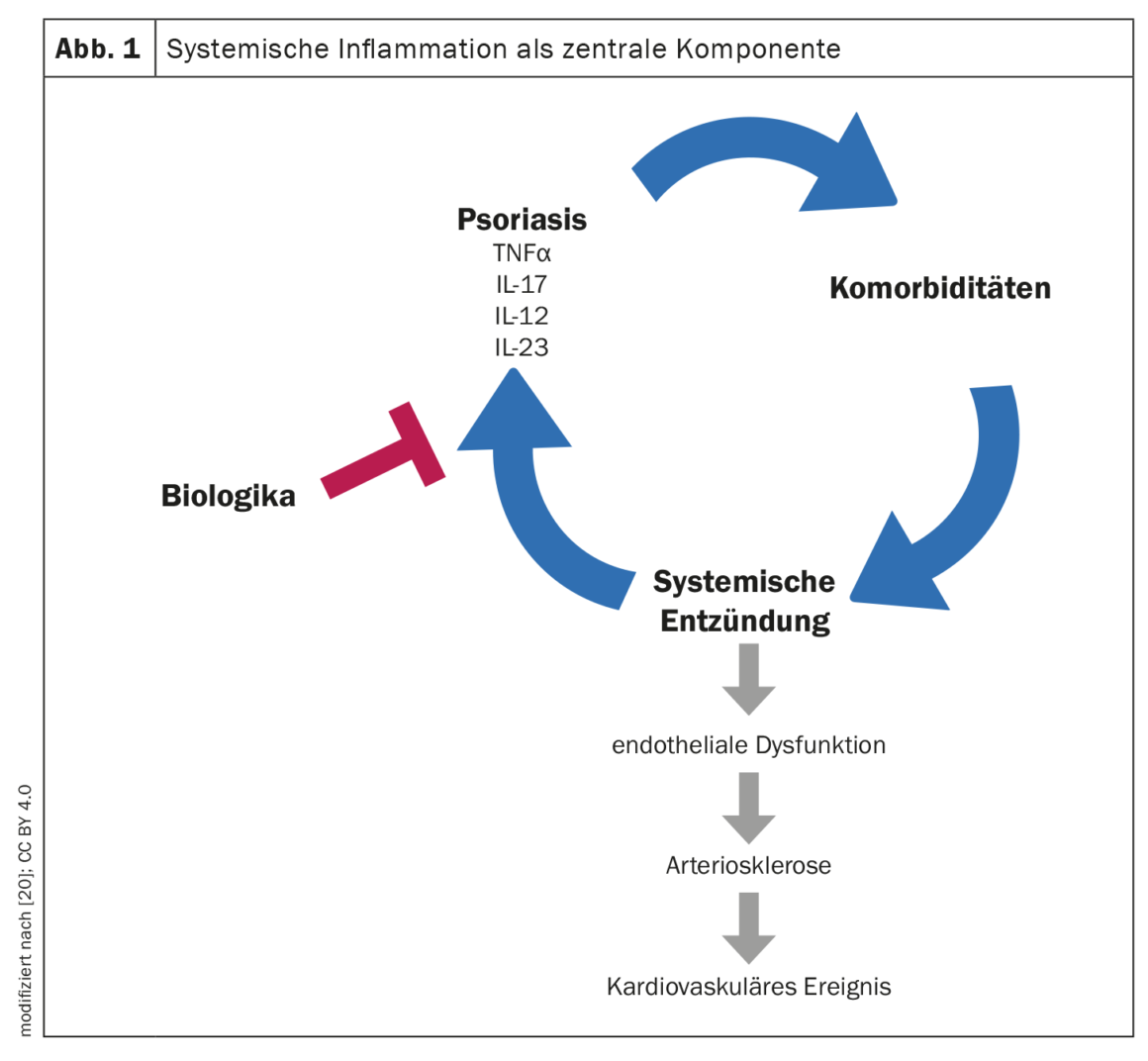
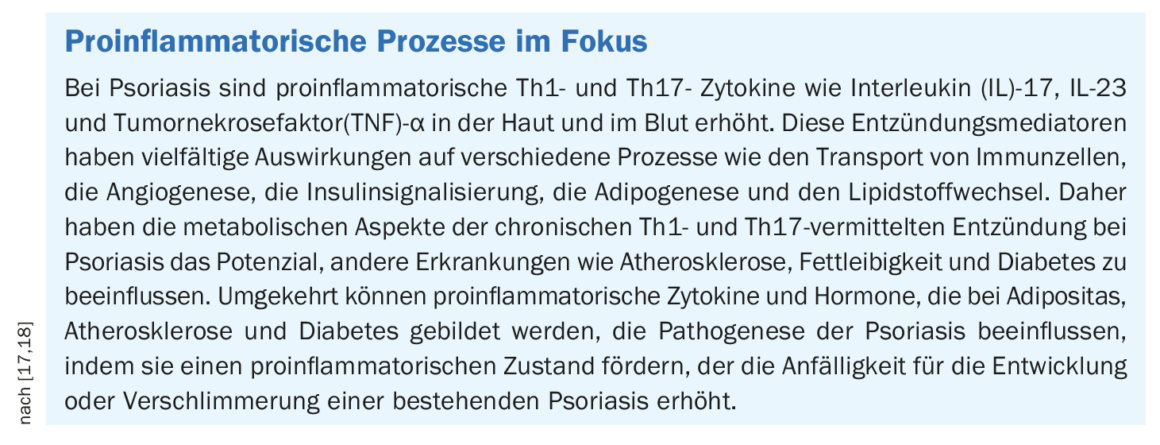
In recent years and decades, research in the field of psoriasis has been able to make considerable progress. With the discovery of the importance of proinflammatory cytokines, the scientific community has come to believe that psoriasis is not a disease of the skin alone. In terms of systemic treatment options, much has happened since the early days of TNF–α inhibitors to the highly potent anti-interleukin (IL)-17 and anti-IL-23 antibodies. The latter two groups of agents are now considered the holy grail of treatment options for moderate to severe psoriasis. “We can positively influence all important domains of the psoriasis disease with these drugs,” summarizes Prof. Ulrich Mrowietz, MD, from the Psoriasis Center Kiel at the University Hospital Schleswig-Holstein, Germany, the great scope of the therapeutic effects of these system therapeutics [3]. As is now known, the pathogenesis of psoriasis is dominated by proinflammatory Th17 cells and, in addition to TNF, IL-17 and IL-23 are central cytokines of the psoriatic inflammatory cascade [4].
Wide-ranging mechanisms of chronic inflammation
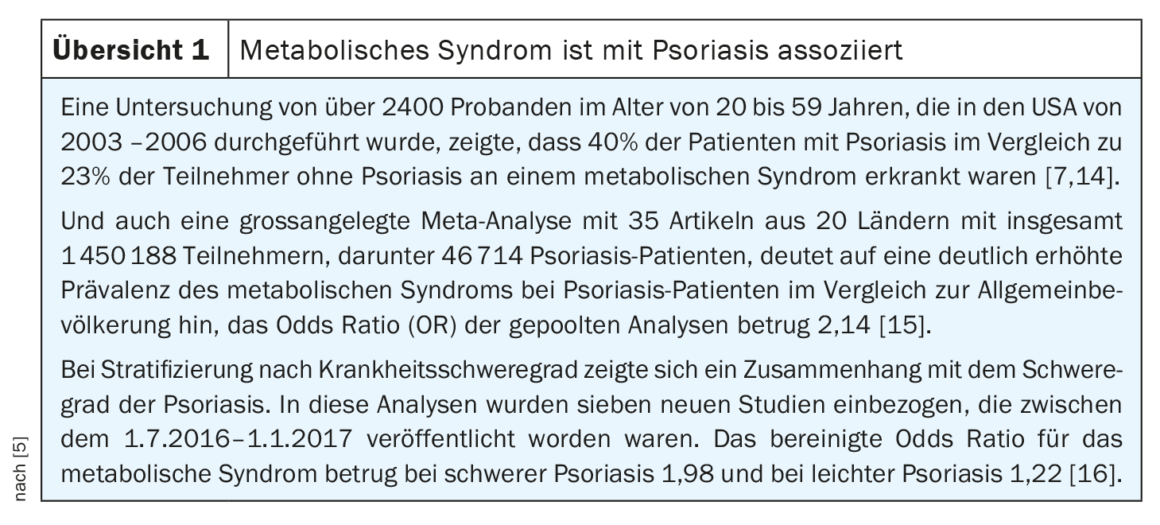
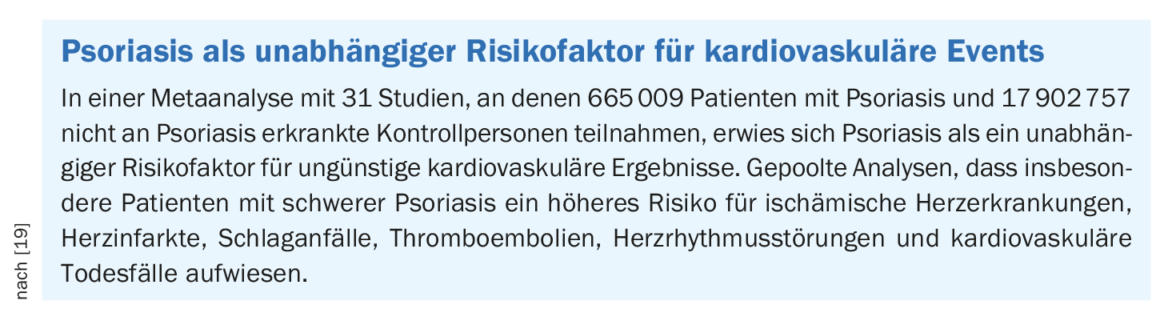
In addition to psoriatic arthritis, numerous comorbidities may occur, such as metabolic syndrome, cardiovascular disease, and depression [5]. Studies show that patients with psoriasis have a higher than average incidence of metabolic syndrome and its components (abdominal obesity, dyslipidemia, and arterial hypertension) (Review 1) [6,7]. While not every psoriasis patient is obese, the prevalence of obesity is higher in psoriasis patients than in the general population [8]. These associations are thought to be explained by chronic inflammatory processes in the body, among other factors [7]. There are findings showing that systemic inflammation (elevated CRP levels) correlates with low HDL cholesterol and a high total/HDL cholesterol ratio [9]. In any case, chronic inflammatory processes that can fuel each other seem to play a central role [10]. Prof. Mrowietz emphasized that psoriasis is associated with vascular inflammation and that this promotes atherosclerosis, which can ultimately lead to myocardial infarction or stroke and reduced life expectancy (box) [3]. As a preventive measure, in addition to a healthy lifestyle, blood pressure and blood lipid levels should be checked regularly by a doctor and treated if necessary.
Stress as a significant trigger factor
In addition, risk factors such as obesity and tobacco smoking should be avoided. “Because these are both factors that significantly worsen psoriasis,” explained Prof. Mrowietz [3]. Trigger factors of psoriasis include stress, with stressors found in both the school/work and home environments of patients. Stress and central nervous changes may contribute to an exacerbation of psoriasis symptoms via a bidirectional interaction between the nervous system and skin immune cells [11]. Scientific findings show that stressful life events play a role in triggering or exacerbating psoriasis [12,13]. “Stress is not only a trigger for increased plaques on the skin,” the speaker emphasized [3]. Stress increases vascular inflammation and affects the central nervous system. As a result, inflammatory cells are mobilized from the bone marrow, which migrate into the bloodstream and eventually promote arteriosclerotic changes, e.g. in the coronary arteries.
Psoriasis and depression – a vicious circle
“We know from studies in Northern Europe that one in five people with psoriasis suffers from depression,” Prof. Mrowietz elaborated [3]. In the past, it was assumed that depressive disorders could be explained primarily by stigmatizing experiences of psoriasis sufferers. However, this is only one of the decisive factors, says the expert and adds: “Depression is an inflammatory disease. There are now good studies showing that there is a particular pattern of inflammation going on in the central nervous system. This pattern favors the development of depression. Conversely, this means the following: If this pattern is known, a more targeted treatment can be initiated, which ideally also has a positive influence on the depressive symptoms. “With modern drugs, this is possible,” said Prof. Mrowietz [3]. This, he said, is evident from numerous scientific study findings. Why knowledge of these correlations is important for dermatologists: “If you are depressed, you are more susceptible to stress, and stress increases psoriasis. When you have stress, messenger substances are increasingly released. Then the immune system is activated”, summarized Prof. Mrowietz [3]. In summary, it is a vicious circle, whereby stigmatization also contributes to the fact that the persons concerned get under stress and the inflammatory scenario intensifies.
Congress: World Psoriasis Day
Literature:
- Meffert H, Rowe E: Psoriasis Akt Dermatol 2004; 30: 504-509.
- “A look at psoriasis through the ages,” Advance Spring 2011, National Psoriasis Foundation, www.psoriasis.org, (last accessed Jan. 19, 2023).
- “The latest on psoriatic disease”, Prof. Dr. med.
Ulrich Mrowietz, World Psoriasis Day 2022, German Psoriasis Association and Skin Network Leipzig/Western Saxony, Oct. 29, 2022. - Volc S, Ghoreschi K: Pathophysiological basis of systems therapies for psoriasis. JDDG 2016; 14(6): 557-573.
- “Aktuelles zur Psoriasis-Krankheit”, Prof. Dr. med. Michael Sticherling, World Psoriasis Day 2022, Deutscher Psoriasis Bund und Hautnetz Leipzig/Westsachsen, 29.10.2022.
- “S3 Guideline Obesity – Prevention and Treatment,” registry number 050-001, version 4. 2 (April 2014).
- Buhles N, Lantzsch H: Psoriasis and metabolic syndrome, www.psoriasisbund.de/fileadmin/images/Ehrenamt/Wissenschaftlicher_Beirat/Seite_des_WB/Heft_1-2018_-_Psoriasis_und_metabolisches_
Syndrome_-_Dr._Nobert_Buhles_and_Dr._Hanka_
Lantzsch .pdf, (last accessed Jan 19, 2023). - Toussirot E, Gallais-Sérézal I, Aubin F: The cardiometabolic conditions of psoriatic disease. Front Immunol 2022; 13: 970371.
- Eder L, et al: Increased burden of inflammation over time is associated with the extent of atherosclerotic plaques in patients with psoriatic arthritis. Ann Rheum Dis 2015; 74(10): 1830-1835.
- “Psoriasis: a disease of the whole body”,
www.weltpsoriasistag.de/wp-content/uploads/2020/
10/Press-release-Public_press_World-Psoriasis-Day-2020_lang.pdf, (last accessed 19.01.2023). - Hölsken S, et al: Common Fundamentals of Psoriasis and Depression. Acta Derm Venereol 2021; 101(11): adv00609.
- Patel N, et al: Psoriasis, depression, and inflammatory overlap: a review. Am J Clin Dermatol 2017; 18: 613-620.
- Mattei PL, Corey KC, Kimball AB: Cumulative life course impairment: evidence for psoriasis. Curr Probl Dermatol 2013; 44: 82-90.
- Love TJ, et al: Prevalence of the metabolic syndrome in psoriasis: results from the National Health and Nutrition Examination Survey, 2003-2006. Arch Dermatol 2011; 147(4): 419-424.
- Singh S, Young P, Armstrong AW: An update on psoriasis and metabolic syndrome: A meta-analysis of observational studies. PLoS ONE 2017; 12(7): e0181039.
- Langan SM, et al: Prevalence of metabolic syndrome in patients with psoriasis: a population-based study in the United Kingdom. Journal of Investigative Dermatology 2012; 132(3 Pt 1): 556-562.
- Sondermann W, et al: Psoriasis, cardiovascular risk factors and metabolic disorders: sex-specific findings of a population-based study. J Eur Acad Dermatol Venereol 2020; 34(4): 779-786.
- Davidovici BB, et al: Psoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditions. J Invest Dermatol 2010; 130: 1785-1796.
- Liu L, et al: Psoriasis increased the risk of adverse cardiovascular outcomes: A new systematic review and meta-analysis of cohort study. Front Cardiovasc Med 2022; 9: 829709.
DERMATOLOGIE PRAXIS 2023; 33(1): 22-23 (published 2/16/2013, ahead of print).











