About half of balanoposthitides and vulvovaginitides are allergic. In addition to a careful anamnesis regarding hygiene habits and products used, sexual anamnesis is of great importance.
In the case of inflammatory changes in the genital area, an infection – whether sexually transmitted or not – is often thought of first and foremost. Even if it is correct to look for and exclude such infectious causes, about 50% of balanoposthitides and an even larger proportion of vulvovaginitis are noninfectious. Other inflammatory dermatoses may also manifest in the genital area. Part of it has allergic causes. In addition to a precise anamnesis with regard to hygiene habits and the products used, the sexual anamnesis in daily (family) practice is of essential importance in the clarification of the causes of such allergic reactions. Although more than 90% of patients request such a sexual history, it is performed in less than half.
According to the immunological mechanism of sensitization and the resulting clinical reaction, three main forms of allergic reactions in the genital area can be distinguished: Immediate type reactions (type I), late type reactions (type IV) and fixed drug exanthema (type IV reaction mediated via resident CD8+ T lymphocytes).
Late type reactions
Late type reactions are likely to be the most common, resulting in eczema. In the genital area, irritant and allergic contact eczema are of particular importance. However, atopic and seborrheic eczema in the genital area can also be observed, which must be differentially diagnosed. The typical eczema morphology with lichenification and scaling (Fig. 1) may not always be evident. Uniform pruriginous erythema is common, with occasional edema (Fig. 2) . Lichenification and excoriation may occur in the area of the labia majora. Atopy can be looked for by history and prick test.
A detailed, careful history regarding irritation, whether mechanical as in prolonged and repeated sexual intercourse/masturbation or chemical, e.g., due to ammonia in the urine, is essential. Therefore, in addition to the sexual history, incontinence problems should also be asked about.

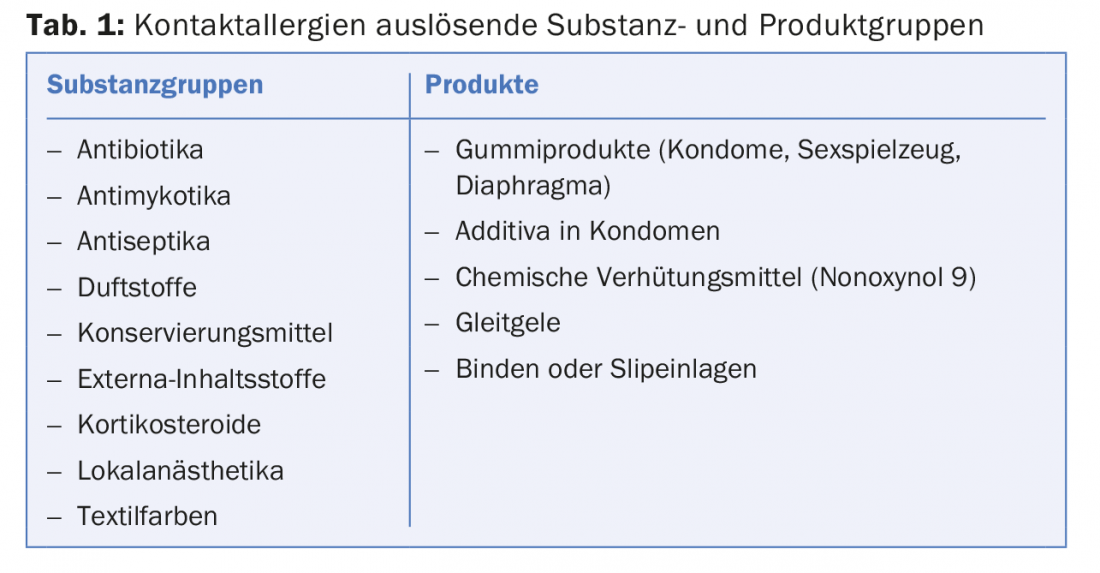
When searching for contact toxins, ask specifically about condoms (latex, rubber accelerators), lubricants, and sex toys (Tab.1). It is not sufficient to note that condoms were used, for example – the brand and the specific product must also be known in order to record the respective coatings, which can range from spermicides to fragrances to (fluorescent) dyes. As far as substances applied beyond this are concerned, there are hardly any limits to the patients’ imagination: The spectrum ranges from local anesthetics to prolong sexual performance to the application of tiger balm in the context of sadomasochistic practices. Sometimes the noxious agent must be sought in the sexual partner. Patients often conceal genitally applied care, lubrication or other aids out of a sense of shame, which is why the topic must be specifically addressed. Out of the same sense of shame, self-therapy often already takes place, which in turn can lead to a non-sexual contact allergy. The previous therapy should therefore be recorded anamnestically and, if possible, clarified in the epicutaneous test.
After elimination of causative factors, mild cleansing, lipid-replenishing care and topical steroids may be used as far as possible. It should be borne in mind that cream bases are more likely to burn in the mucous membrane area than ointments. Also, cream bases contain more preservatives, which again can cause irritation or secondary contact allergy.
Patients should always be brought into a therapeutic balance with regard to their hygiene habits, in which lack of cleansing must be avoided as well as over-care with frequent use of irritant detergents. This is especially important if pretreatment has already taken place. Inappropriate or too intensive therapy, often with rapid change of preparations if there is no response, can lead to perpetuation of the eczema, which is why in these situations any therapy may have to be temporarily paused.
Instant type reactions
Immediate type reactions in the genital area are much rarer than late type allergies. Symptomatology may be localized and manifest as edema or urticaria, but is much more pronounced in nearly three-quarters of patients with a systemic reaction, which may extend to anaphylaxis. Seminal plasma allergies exist mostly to the major allergen prostate-specific antigen (PSA), which has sequence homology to Can f 5, the major allergen of dog hair allergy. This cross-reaction may also explain the occurrence of symptoms during the first unprotected sexual intercourse, if a dog hair allergy is already present. Detection of specific IgE against seminal plasma and a positive prick-to-prick test are diagnostic.
Other immediate-type allergens relevant in the genital area are latex (condoms) with the main allergens Hev b 1 and Hev b 6, against which specific IgE can also be detected.
Immediate-type allergens from food (e.g. peanut, Brazil nut) and drugs (e.g. amoxicillin) can also be transferred by sperm in the sense of a heterotransfer and thus trigger reactions.
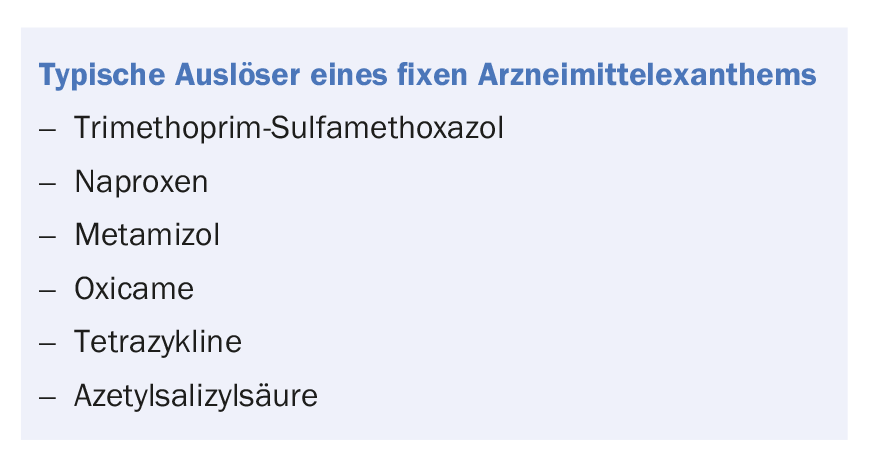
Fixed drug exanthema
The genital area is a predilection site for fixed drug exanthema, accounting for over 50%. In men, blisters on livid erythema occur on the glans or in the sulcus coronarius, in women on the vulva. Often, blisters are no longer visible, but only erosions or ulcerations with a livid rim are present (Fig. 3) . Accordingly, the differential diagnostic clarification can be difficult, especially in the first episode, if it is not thought of. In case of repeated episodes with a suitable drug history, the diagnosis becomes easier (box). In addition to re-exposure with reaction, the positive epicutaneous test performed intralocularly is conclusive, but by its nature is not always practical. Therapeutically, only allergen abstinence remains.

Take-Home Messages
- More than half of balanoposthitis and vulvovaginitis are noninfectious. Among them are also allergic
- Reactions. These can be divided into three forms: Immediate type reactions, late type reactions and fixed drug exanthema.
- Late type reactions, especially allergic contact dermatitis, are most common. Atopic and seborrheic eczema must be differentially diagnosed.
- More rarely, immediate type reactions occur, mostly with systemic symptomatology. Allergic reactions can be triggered by semen (prostate specific antigen, food, medication) and latex.
- Fixed drug exanthema manifests on the glans or sulcus coronarius in men and on the vulva as blisters or erosions on livid erythema in women.
Further reading:
- Yale K, et al: Genital Allergic Contact Dermatitis. Dermatitis 2018; 29(3): 112-119.
- Marfatia YS, et al: Genital contact allergy: A diagnosis missed. Indian J Sex Transm Dis AIDS 2016; 37(1): 1-6.
- Eubel J, Diepgen TL, Weisshaar E: Allergies in the genital area. Dermatologist 2015; 66: 45-52.
- Borelli S, Lautenschlager S: Differential diagnosis and.
- Management of balanitis. Dermatologist 2015; 66(1): 6-11.
- Bauer A, Oehme S, Geier J: Contact sensitization in the anal and genital area. Curr Probl Dermatol 2011; 40: 133-141.
- Kügler K, et al: Anogenital dermatoses. Allergic and irritant trigger factors. Analysis of data from the IVDK and literature review. J Dtsch Dermatol Ges 2005; 3(12): 979-986.
- Bhate K, et al: Genital contact dermatitis: a retrospective analysis. Dermatitis 2010; 21(6): 317-320.
- Moraes PS, Taketomi EA: Allergic vulvovaginitis. Ann Allergy Asthma Immunol 2000; 85(4): 253-265.
- Meystre-Agustoni G, et al: Talking about sexuality with the physician: are patients receiving what they wish? Swiss Med Wkly 2011; 141: w13178.
DERMATOLOGIE PRAXIS 2018; 28(6): 8-10











