The diagnosis of chronic insomnia-one of the most common disorders in sleep medicine-is made clinically and requires a careful review of the medical and sleep history. When selecting a treatment strategy, it is important to consider patient preferences in addition to potential comorbidities. In addition to medicinal measures, psychotherapeutic procedures should also be offered.
According to the International Classification of Sleep Disorders (ICSD-3) and the Diagnostic and Statistical Manual of the U.S. Psychiatric Association (DSM-V), chronic insomnia is said to occur when patients suffer from difficulty falling asleep or staying asleep for ≥3 months on at least three days per week and it adversely affects daytime performance**. Furthermore, the insomnia should not be explained by another disease or environmental factors$ [1–3].
** Fatigue/discomfort; attention/concentration/memory disturbance; impairment in social, family, occupational functioning; limitations in performance; mood swings; irritability; daytime sleepiness; behavioral disturbances such as hyperactivity, impulsivity, aggression; decreased motivation/energy/drive; susceptibility to errors and accidents; concern about unrestfulness of sleep; dissatisfaction with sleep.
$ Lack of adequate sleep opportunity (e.g., sufficient time for sleep) or inadequate sleep circumstances (e.g., lack of a safe, dark, quiet, and comfortable sleep environment)
If patients develop chronic sleep disorders, a referral to a sleep center may be appropriate, according to PD Dr. med. Marc Spielmanns, Head Physician Pulmonary Rehabilitation & Medical Director of the Zurich Rehab Centers, Wald Clinic and Medical Director at the Center for Sleep Medicine Zurich Oberland [1]. There, a careful anamnesis and assessment of findings is first carried out. Standardized sleep-related screening questionnaires can be used for this purpose, such as the Sleep Quality Questionnaire (PSQI), the Insomnia Severity Index (ISI), and the Epworth Sleepiness Scale (ESS). Psychiatric questionnaires such as the Beck Depression Inventory (BDI) are also available. It is also important to exclude other somatic diseases.
Sleep medical clarifications – OSAS or RLS are also possible
The type of sleep disorder (e.g. insomnia, obstructive sleep apnea syndrome, restless legs syndrome, hypersomnia, parasomnia) is determined in the sleep center using actimetry, sleep diary and other methods. Sleep disorders are not only associated with reduced well-being, but also with increased morbidity and mortality. For example, the risk of weight gain and that diabetes mellitus will develop increases. However, mental health often suffers as well, which can manifest as anxiety, depression, and suicidality [4]. It is also possible that psychological problems are the cause of sleep disorders. If appropriate, a referral to psychotherapy will be initiated.
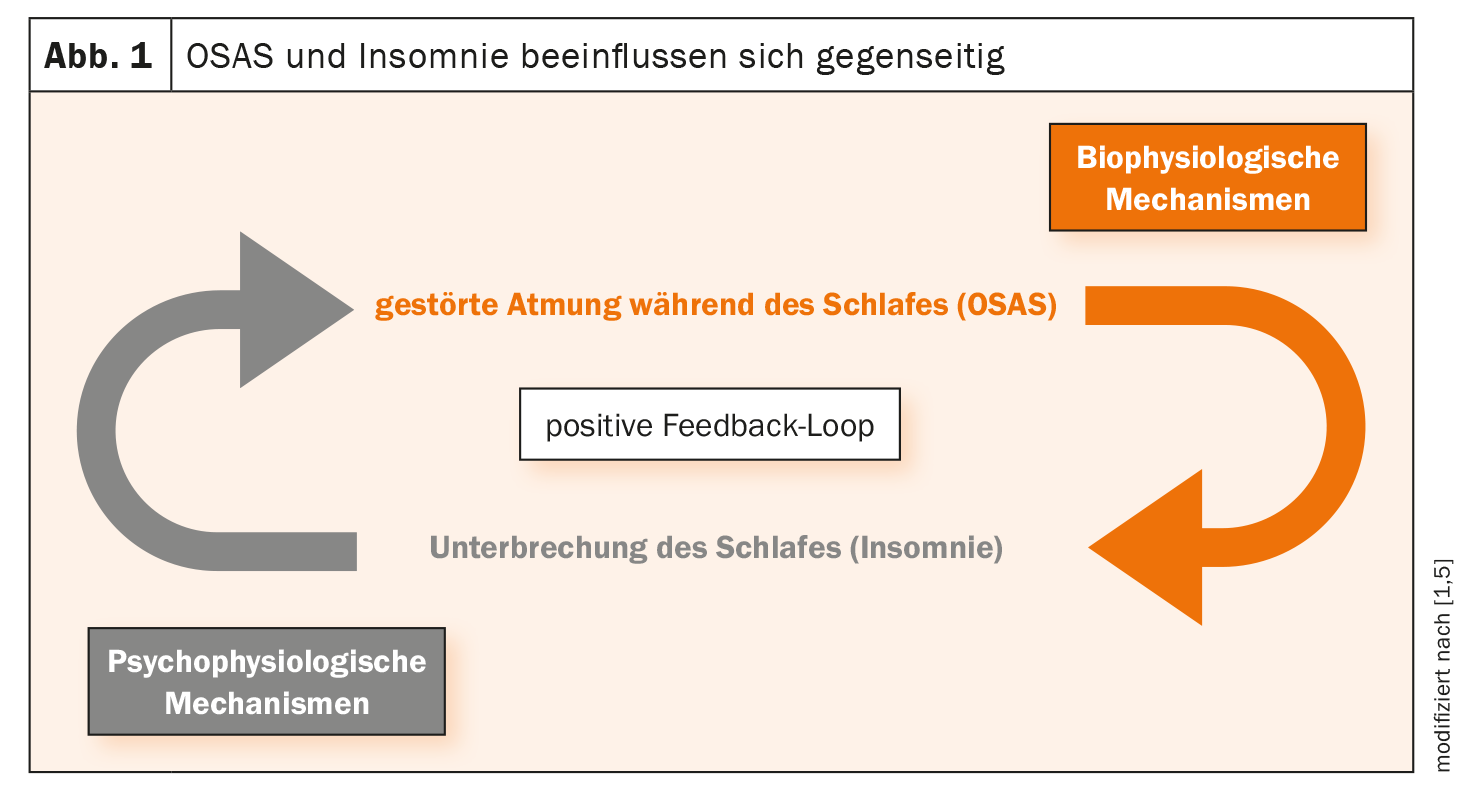
Insomnia has a high coincidence with obstructive sleep apnea syndrome (OSAS), Dr. Spielmanns reported [1,5]. About 20-25% of OSAS patients suffer from relevant insomnia. In affected individuals, both should be treated if possible (Fig. 1) .
Biopsychosocial explanatory model: vulnerability factors present?
Helen Slawik, MD, senior physician, co-director of the Center for Sleep and Chronomedicine at Basel University Hospitals, University Psychiatric Clinics (UPK) Basel explained the risk factors for chronic sleep disorders: in addition to female gender and a familial disposition, these include a biological vulnerability described as hyperexcitability or increased HPA axis activity. But psychological vulnerability factors were also observed such as neuroticism, perfectionism, emotion suppression, introversion, reduced resilience. The presence of other sleep disorders such as sleep apnea syndrome, narcolepsy or restless legs disease and mental illnesses (depression, anxiety disorders, substance use, gambling addiction) also increase the risk of chronic insomnia.
Psychotropic drugs and non-drug measures
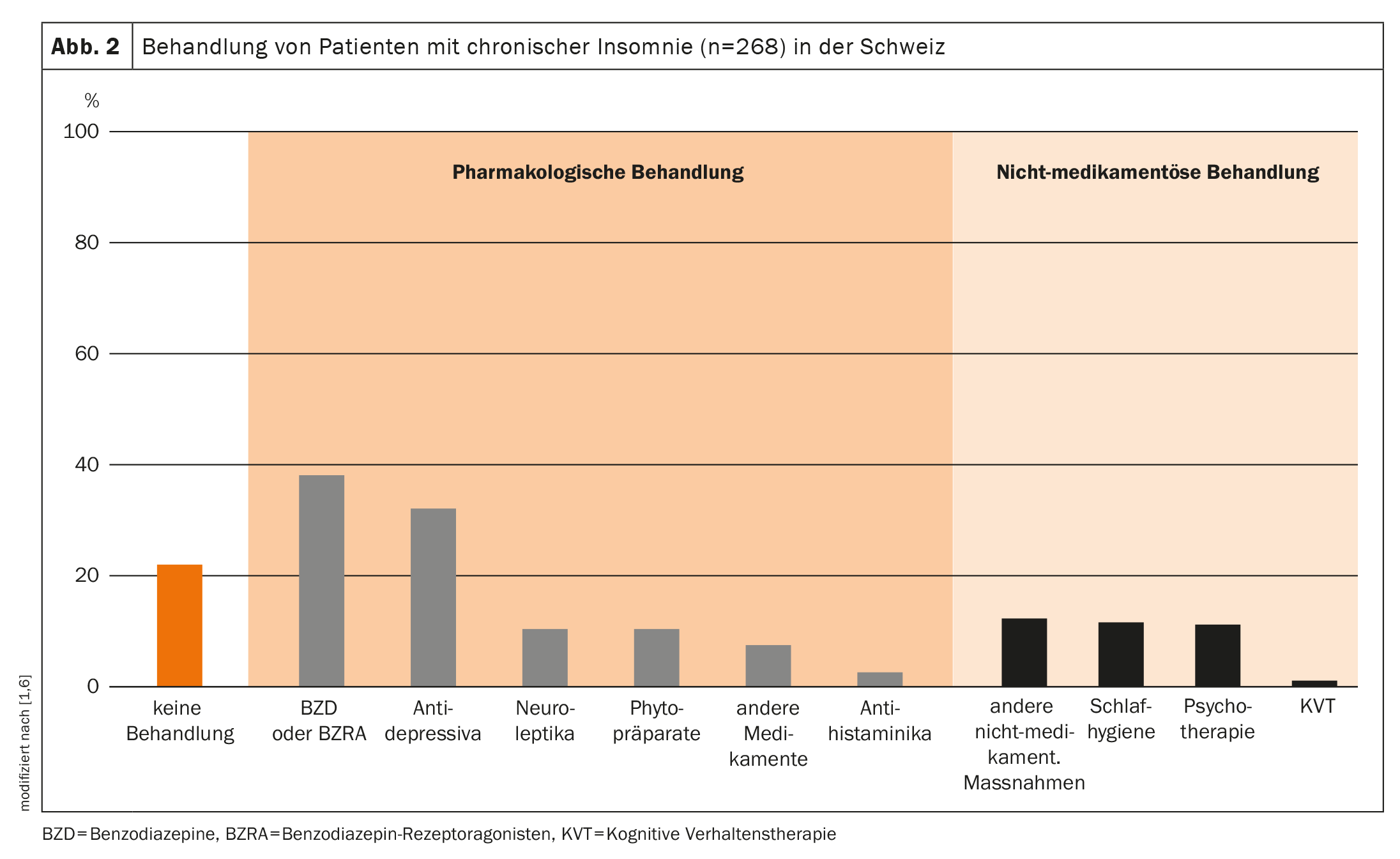
In a study published in 2020 by Maire et al. the care situation of patients with chronic insomnia in Switzerland was investigated [6]. It was found that about one fifth remained untreated and the majority of pharmacologically treated patients received either benzodiazepines, benzodiazepine receptor agonists or antidepressants (Fig. 2) . Further analysis showed that benzodiazepines were often taken for longer than 1 month and more than once a week. This is problematic in terms of tolerance development and dependence, the speaker said. The use of hypnotics can bring about rapid symptom reduction, but one must accept certain side effects.
Behavioral therapy is recommended by international guidelines
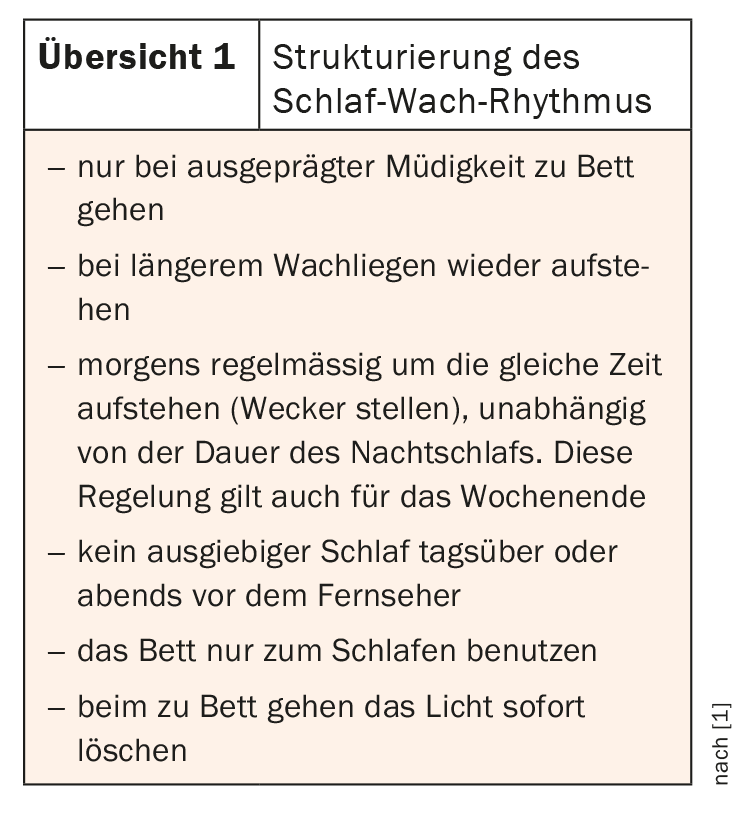
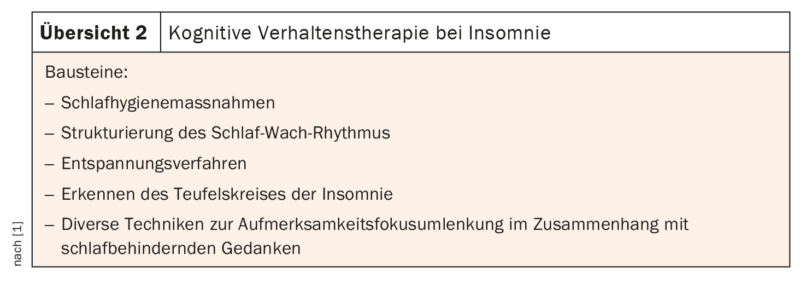
As an alternative or complement to medication, patients with chronic insomnia should be offered the option of cognitive behavioral therapy (review 1 and 2) .
At UPK Basel, these are conducted in an outpatient setting (8 sessions) or as a 14-day inpatient sleep training program, and the success rate is about 60%, the speaker said. In the American Academy of Sleep Medicine clinical practice guidelines, KVT is strongly recommended, whereas relaxation techniques alone, stimulus control, or sleep restriction are only conditionally recommended [7]. As an alternative therapy method, the speaker refers to “Acceptance and Commitment Therapy” (ACT). A basic assumption is that one neither fights against the insomnia nor resigns, but asks oneself what is possible despite fatigue. From a chronomedical point of view, melatonin and light should be used supportively to the respective chronotype. Accordingly, it makes sense for a morning type to use light in the late afternoon to support sleep restriction, while for a late type this should rather be scheduled in the morning.
Congress: Forum for Continuing Medical Education
Literature:
- «Linderung der Belastung durch chronische Insomnie», Forum für Medizinische Fortbildung (FomF), WebUp, 13.06.2023.
- The AASM International Classification of Sleep Disorders. ICSD-3 International Classification of Sleep Disorders. Darian: AASM 2014; 3rd ed. Diagnostic and coding manual.
- Heidbreder A: Chronische Insomnie – alte, neue und zukünftige Therapieoptionen. InFo Neurologie 2023; 25(5): 38–49.
- Grandner MA: Sleep, Health and Society. Sleep Med Clin 2017; 12(1): 1–22.
- Janssen HCJP, et al.: Management of insomnia in sleep disordered breathing. Eur Respir Rev 2019; 28: 190080.
- Maire M, et al.: Prevalence and management of chronic insomnia in Swiss primary care: Cross-sectional data from the «Sentinella» practice-based research network. J Sleep Res 2020; 29(5): e13121.
- Edinger JD, et al.: Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 2021; 17(2): 255–262.
InFo NEUROLOGIE & PSYCHIATRIE 2023; 21(4): 28–29